Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
The legacy healthcare system has fragmented, disconnected systems that make it difficult for patients to access or providers to deliver seamless care. Our platform—ro.OS (the Ro Operating System)—is built to change that. Every piece of the Ro platform, whether a self-service feature for patients, a clinical tool for practitioners, or a data workflow for care teams, plays a role in delivering care that’s easy, effective, and scalable. With Ro, patients don’t just have access to appointments, treatments, or their medical record; they get a platform that serves as a partner throughout their individual health journeys.
Just like LEGO® blocks, the systems that power ro.OS are modular, replicable, interconnected, and designed to snap together to create something greater than the sum of their parts. At Ro, we intentionally keep this idea in mind as we design and build new features and tools for our platform.
In this series, we’re spotlighting one platform feature at a time. Today, we’ll focus specifically on how we’re bringing transparency to the insurance approval process.
Shedding light on the insurance black hole
Understanding a health insurance policy is often challenging, let alone getting treatment approved for coverage when a prior authorization (PA) is required. During the PA process, patients are often left in the dark, unable to get answers from their provider, pharmacy, or insurance company.
They’re left wondering: What’s the status of my treatment coverage? Am I approved? Can I get my prescription filled?
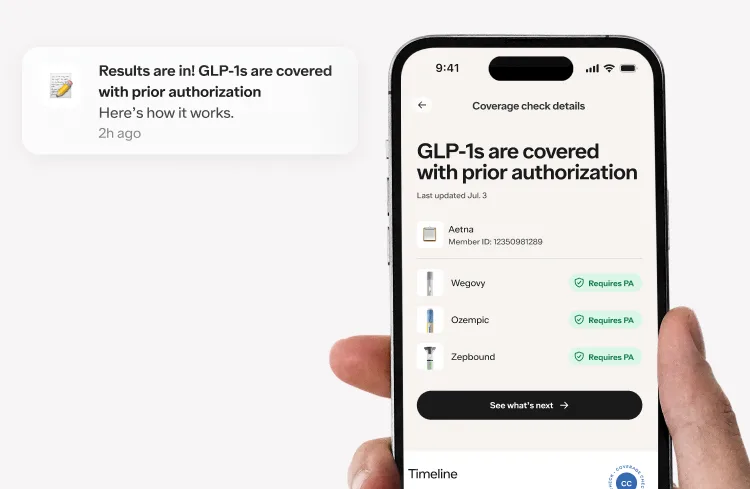
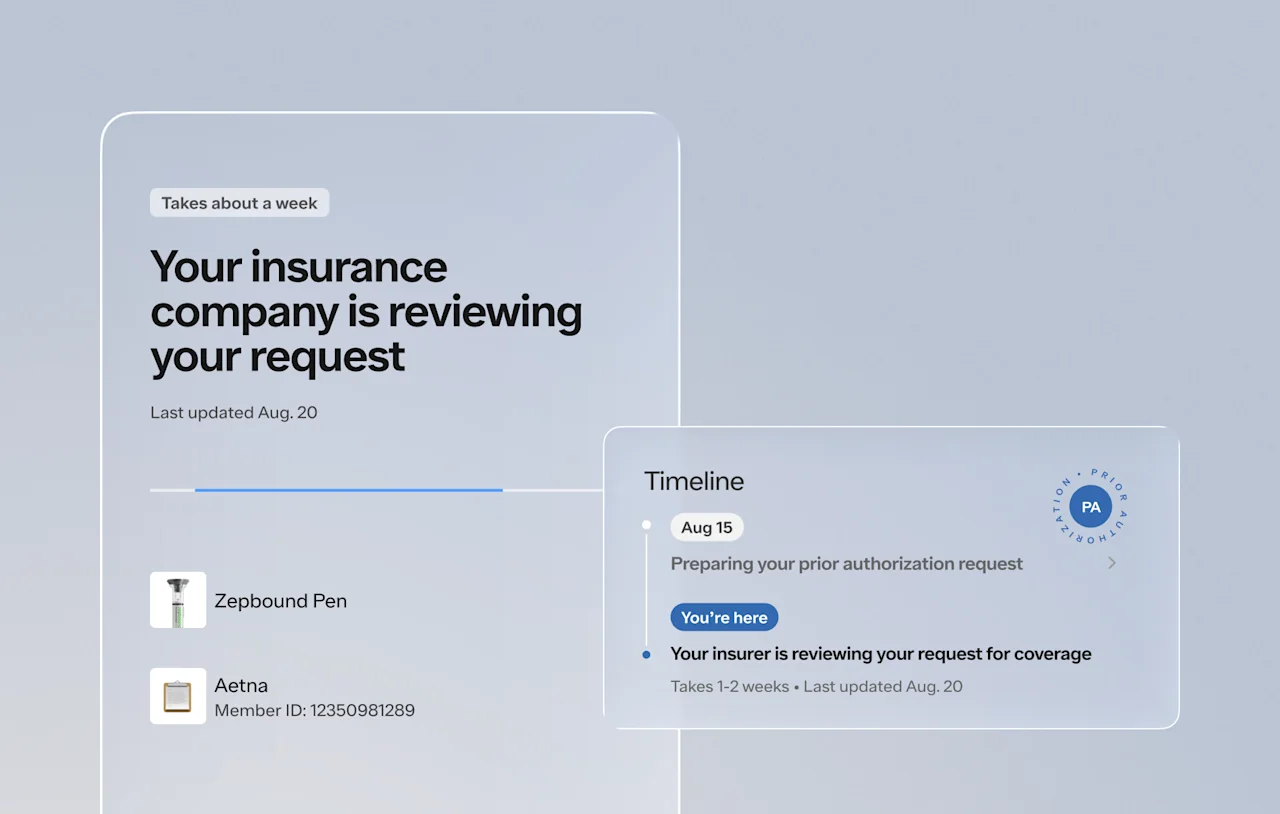
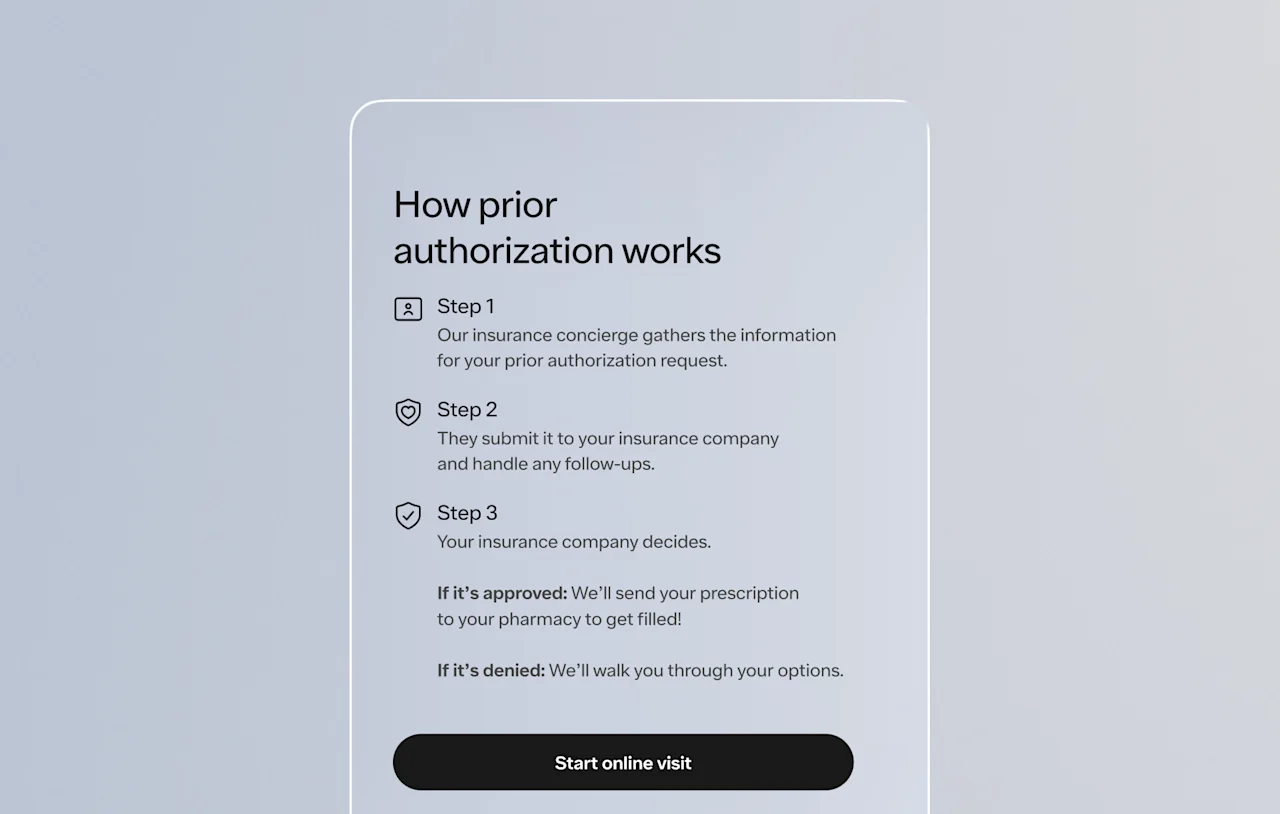
That’s why we set out to give patients transparency and clear guidance to help them understand each step of their insurance approval process. We launched the Prior Authorization Details Page, a dedicated, self-service page that helps patients understand where they are in the PA journey, what comes next, and how to take action if needed.
How it works
The Prior Authorization Details Page lives inside each patient's Ro account and is available as soon as a PA request kicks off. This page walks patients through their status, timeline, and options. We also surface when relevant information becomes available through push notifications and Ro’s Help Center to keep patients informed, wherever they are in the process—all without needing to message Ro’s care team.
“Across healthcare, the insurance journey is a black box from start to finish. When patients have a health goal in mind, and the hopes of getting coverage to help them afford the treatment to achieve that goal, they are incredibly excited to move as quickly as possible to get started. At Ro, we take on some of that burden for them, and want to keep them up-to-date and ensure they feel supported along the way.
The Prior Authorization Details Page is a game changer. It helps patients navigate this complex process with a tool at their fingertips, offering a detailed view of where their prior authorization request stands, what’s left to do, and when they should hear back. It also features educational resources on what each stage means and what to expect once they receive an insurance coverage decision.” — Emily Strait, Senior Manager, Strategy & Operations
Built with patients in mind
This experience was designed to reduce uncertainty and help patients feel confident in their care. We prioritized clarity, accessibility, and self-service. The results speak for themselves:
Fewer patient issues: Issue creation after PA notification dropped 24%
Reduced message volume: PA-related messages dropped nearly 17%
High engagement: Over 6.9K visits to the PA Details Page in just the first two weeks of launch
“Prior authorizations, and really anything insurance related, are confusing and not something patients deal with on a regular basis. There is a large info gap between patients and their insurance plan, and that can be daunting for patients. The Prior Authorization Details Page allows patients to better understand what is happening, what to expect and what some of the terms mean, like PA (prior authorization), QLO (qualifying life event), PBM (pharmacy benefit manager). So many acronyms.
It's one thing to be told ‘We're waiting on insurance’ it's another thing to be told ‘We submitted the PA on this date, we usually hear back in 1-2 weeks, and here is information you can use to understand what the decision will mean for your treatment.’ This kind of transparency and experience is reassuring to patients and shows them we are actively fighting for coverage, and in the event medications aren't covered by their insurance, what comes next.” — Becca Dan, RN, Special Teams
Powered by ro.OS
The seamless patient experience that the Prior Authorization Details Page offers is only possible through a platform like ro.OS. By integrating benefits checks, care team messaging, and a patient’s medical record into a convenient workflow, we’re turning what used to be a void of confusion into a patient-centric, guided experience.
“This detail page isn’t just a win for patients—it’s a foundational block that reflects how ro.OS lets us build tools that can serve multiple audiences. The same underlying data processing that powers our internal workflows, like task statuses, activity logs, and benefits verification updates, also drives what patients see. That means patients get updates about their care progress as soon as we do, powered by the exact same source of truth that our care teams use.
Because we’ve organized these blocks modularly in ro.OS, we can easily surface updates across experiences. If there’s a new development, a notification appears on the patient’s home screen. If action is needed, the patient is prompted with a task in their account. And clicking those items leads the patient directly to the relevant page—built from the same framework we’re using for pages dedicated to medication orders, prescriptions, lab results, and beyond.” — Steve Marks, Vice President of Product
What’s next
This is just one example of how we’re using technology to make care easier, more effective, and more scalable. Each feature we build on our platform strengthens Ro’s ability to deliver high-quality care to millions of patients.
The Prior Authorization Details Page is one of many detail pages that each guide patients through unique moments in their journey, whether it’s checking the status of their latest order, reviewing prescription information, or—as we covered here—understanding whether their treatment has been approved by their insurance plan. By bringing together the information patients need in one clear, easy-to-understand place, we’re giving them more control, more clarity, and more confidence at every step of their journey.
This is what building is all about at Ro: giving patients a better experience, one piece at a time.