Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Endometriosis is a common condition affecting about 10–15% of people with uteruses before menopause (Tsamantioti, 2021).
It can be tricky to diagnose. Some experience no symptoms, while others can have symptoms that significantly impair their ability to live their lives. It's also not uncommon for endometriosis to initially be misdiagnosed because the symptoms can resemble other illnesses (Tsamantioti, 2021).
If you’ve recently been diagnosed, it's essential to know what endometriosis symptoms you might experience. While there might not be a cure for endometriosis right now, there are effective treatment options for managing symptoms to help you live the life you want.
What is endometriosis?
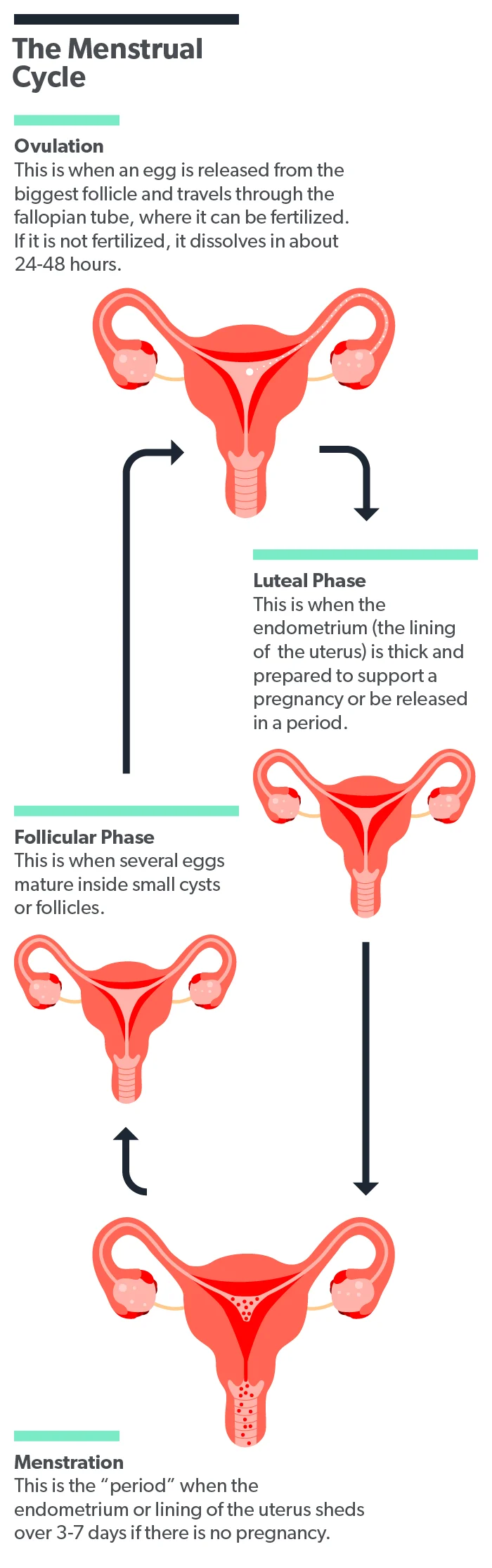
The inside lining of the uterus is called the endometrium. Every month, it grows thicker in response to the body’s hormones. It does this in preparation for receiving a fertilized egg to allow for pregnancy. If no pregnancy happens that month, the body sheds the endometrium. This is your monthly menstrual cycle.
Endometriosis is a condition where the endometrial cells that should only be inside the uterus instead grow outside of the uterus. Endometriosis can occur anywhere throughout the body. The most common location is just outside the uterus in the ovaries and fallopian tubes, but endometriosis can also affect the (Tsamantioti, 2021):
Large and small intestines
Other pelvic organs
Lining of the heart or lungs
Central nervous system
The endometrial tissue outside the uterus still responds to your body’s hormones the same way that the endometrium does. That means it grows each month with your menstrual cycle and then breaks down. Unlike the lining of your uterus, though, the tissues outside the uterus have no way to exit the body. This trapped endometrial tissue is what causes any symptoms that you experience (Dydyk, 2021).
The exact cause of endometriosis isn’t known, but there are many theories. Still, none of these theories can explain all of the symptoms that people with endometriosis experience (Tsamantioti, 2021).
The symptoms of endometriosis
Unlike other types of illness, the amount of symptoms you have doesn’t always directly relate to the amount of endometriosis you have. You can experience significant symptoms even if you only have minimal disease. Others may have considerable excess tissue growth but have minimal to no signs. Their endometriosis might only be found after surgery for another reason (Tsamantioti, 2021).
Pelvic pain
Between 50% and 70% of women with chronic pelvic pain will also be diagnosed with endometriosis. The pain associated with endometriosis is usually described as chronic pain in the pelvic area that gets worse over time. The pain is generally cyclic, meaning it comes and goes in a cycle. This cycle corresponds to the endometrial tissues growing and shedding with monthly hormone changes in the body (Tsamantioti, 2021; Dydyk, 2021).
People with endometriosis commonly report experiencing painful periods and severe menstrual cramps (Tsamantioti, 2021).
Infertility
Endometriosis has also been linked with infertility or trouble getting pregnant. Researchers aren’t exactly sure why, but 30–50% of women with endometriosis will have at least some difficulty getting pregnant (Macer, 2012).
One theory about endometriosis-related infertility is that the body’s attempts to clear away the endometrial tissue outside the uterus lead to inflammation. This inflammation leads to pain, scarring of the tissues, and bands of scar tissue that cause internal organs to stick together (adhesions). This inflammation and scar tissue can lead to women having trouble getting pregnant (Bulun, 2019).
GI symptoms
People who have endometriosis that has spread to the large bowel, the small bowel, or the rectum can experience various gastrointestinal symptoms. These can include (Tsamantioti, 2021):
Diarrhea
Constipation
Abdominal pain or cramping
Bloating
Rectal bleeding
These symptoms can sometimes lead to misdiagnosis since they resemble other conditions like inflammatory bowel disease or irritable bowel syndrome (Tsamantioti, 2021).
Other symptoms
Other common symptoms of endometriosis can include pain with sexual intercourse, pain with urination, and pain with bowel movements (Tsamantioti, 2021).
Some people who have endometriosis can experience a condition called hyperalgesia. This happens when the brain interprets any stimulus, such as a light touch, to the affected area as severe pain. It’s a form of neuropathic pain caused by nerve damage from the endometriosis cells (Tsamantioti, 2021).
Are there different stages of endometriosis?
The degree of your endometriosis can be measured in stages—surgery is the only way to know for sure what stage you have. The type of surgery is called “laparoscopic,” where a surgeon looks into your abdomen or pelvis with a camera inserted through small incisions. Your surgeon can see any signs of endometriosis and take tissue biopsy samples if needed (Hoyle, 2021).
The American Society for Reproductive Medicine categorizes endometriosis into four stages. These stages are (Hoyle, 2021):
Stage I (minimal): Small, solitary lesions without significant adhesions
Stage II (mild): Superficial lesions less than 5 cm, without significant adhesions
Stage III (moderate): Multiple deep lesions, small endometriomas (cyst-like lesions) on one or both of the ovaries, and thin adhesions
Stage IV (severe): Multiple deep lesions, large endometriomas on one or both ovaries, with thick adhesions
Most people are found to have stage I or II endometriosis, although it’s important to know that the stage doesn’t necessarily match the degree of symptoms you might have. Some people with low stages might have severe symptoms, while some with high stages might still have mild to moderate symptoms (Hoyle, 2021).
How do you treat endometriosis?
There is currently no cure for endometriosis. Instead, various medications and surgical treatments can relieve the symptoms, improve quality of life, and increase the chances of fertility (Tsamantioti, 2021).
Medications
First-line medications for endometriosis include non-steroidal anti-inflammatory drugs such as ibuprofen for pain and hormonal contraceptives to reduce ovulation and estrogen levels. Hormonal contraceptives (birth control) can include the birth control pill or an intrauterine device (IUD) containing levonorgestrel (Tsamantioti, 2021; Brown, 2014).
If these medications don’t work well enough for you, your provider might consider a class of drugs called gonadotropin-releasing hormone (GnRH) agonists. These medications cause a reduction in a few different hormones in the body and slow the growth of endometriosis tissues (Brown, 2014).
Surgery
Surgery to remove your endometriosis lesions is another treatment option. Due to the risks and complications with any surgical procedure, surgery is usually reserved for cases where medications haven’t worked. The advantage of surgery is that removing the endometriosis and scar tissue can relieve your pain and increase your fertility simultaneously (Tsamantioti, 2021).
In women with endometriosis undergoing fertility treatments, laparoscopy to remove endometriosis tissue has been found to improve spontaneous pregnancy rates in the months following surgery (Brown, 2014).
Assisted reproduction
Women with endometriosis experience lower fertility rates than those without the condition. While many women with mild to moderate endometriosis can still get pregnant without any medical interventions, women with more severe disease have lower pregnancy rates and might require assisted reproductive technologies (Macer, 2012).
In-vitro fertilization (IVF) is reported to be the most successful option for women with all stages of endometriosis. Your reproductive medicine specialists might also recommend using medications or surgery before undergoing IVF to improve your odds of a successful pregnancy (Macer, 2012, Brown, 2014).
Endometriosis can lead to a wide variety of symptoms that can significantly impact your life, from general comfort to planning your family. If you have or believe you may have endometriosis, there are treatment options that can help. By working closely with your healthcare provider, you can find the right approach to help you live the life you want to live.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Brown, J., & Farquhar, C. (2014). Endometriosis: an overview of Cochrane Reviews. The Cochrane Database Of Systematic Reviews, 2014 (3), CD009590. doi: 10.1002/14651858.CD009590.pub2. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6984415/
Bulun, S. E., Yilmaz, B. D., Sison, C., Miyazaki, K., Bernardi, L., Liu, S., et al. (2019). Endometriosis. Endocrine Reviews, 40 (4), 1048–1079. doi: 10.1210/er.2018-00242. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6693056/
Dydyk AM, Gupta N. (2021). Chronic pelvic pain. [Updated 2021 Jul 12]. In: StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554585/
Hoyle AT, Puckett Y. (2021). Endometrioma. [Updated 2021 Jun 15]. In: StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559230/
Macer, M. L., & Taylor, H. S. (2012). Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstetrics And Gynecology Clinics Of North America, 39 (4), 535–549. doi: 10.1016/j.ogc.2012.10.002. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538128/
Tsamantioti ES, Mahdy H. (2021). Endometriosis. [Updated 2021 Feb 25]. In: StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK567777/











