Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
As people in the US continue to have kids later in life, more will use assisted reproductive technology (ART) — including egg freezing, embryo freezing, intrauterine insemination (IUI), and in vitro fertilization (IVF).
Although these technologies have led to the birth of over 7 million babies worldwide (science is amazing!), they aren't an "insurance policy." We've said it before and we can't say it enough — using IVF or any other fertility treatment doesn't guarantee pregnancy, regardless of your age, health, or anything else.
Still, both the general public and physicians who are *not* women's health or infertility specialists sometimes overestimate the success of IVF, which means that people may be making decisions about these medical treatments without the most up-to-date and accurate information.
In this post, we'll break down each of the steps of the IVF pipeline that are required to go from retrieving mature eggs to a pregnancy, explain why one egg does not guarantee one pregnancy, and outline some steps you can take to increase your chances of success with IVF.
Key takeaways
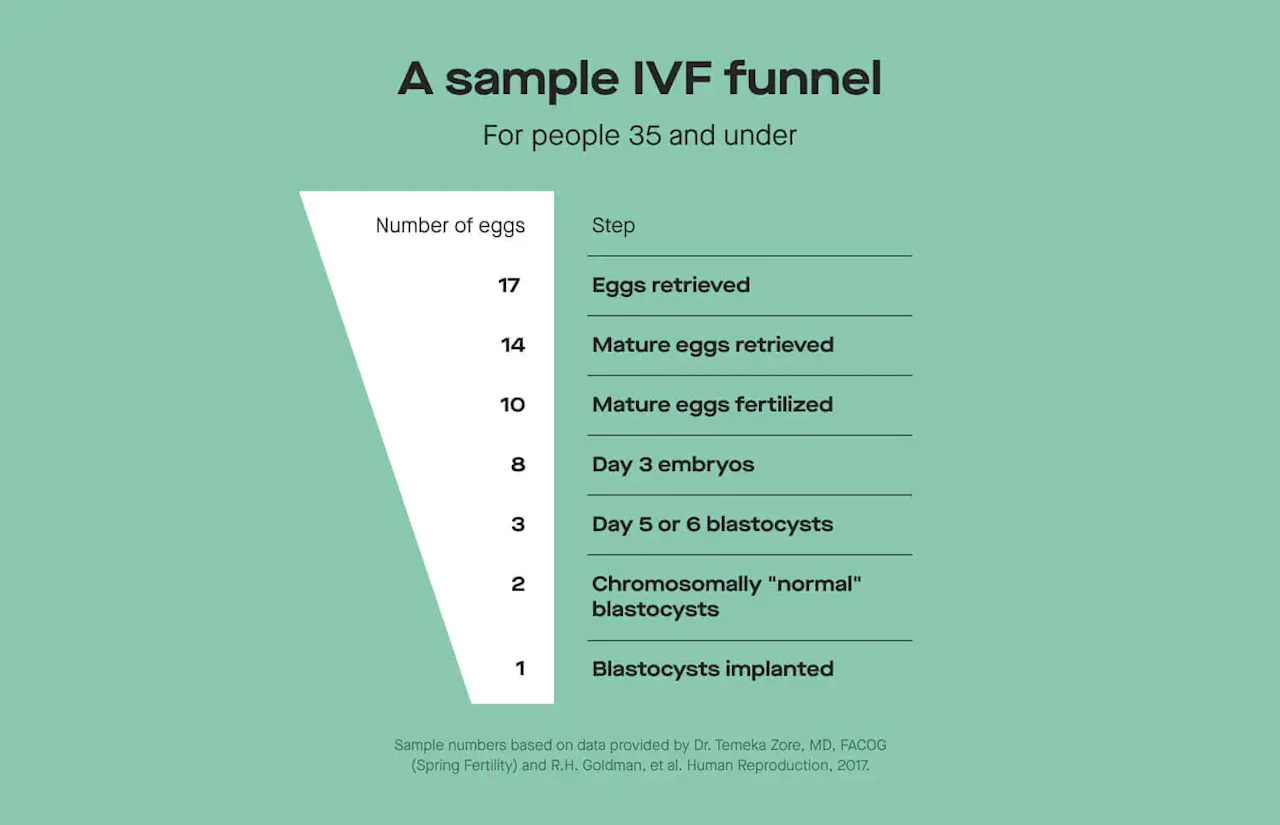
Each step of the IVF process is associated with some decreases in the number of eggs or embryos that make it to the next step, which is why each egg retrieved does not eventually equal one pregnancy. We call this the IVF funnel.
Ultimately, the chances that one egg retrieval cycle will eventually result in a live birth (based on data from the Society of Assisted Reproductive Technology, or SART) are 55.6% for people under 35; 40.8% for people 35-37; 26.8% for people 38-40; 12.6% for people 41-42; and 3.9% for people 43 and over.
Whatever your age, lifestyle, or level of health, there's no guarantee that IVF will result in pregnancy — but age does affect both the number of eggs and genetic quality of eggs a person with ovaries has.
While we can't control things like age, there are things people can do that may boost their odds of success in IVF, like researching clinic success rates, keeping tabs on physical and mental health, and understanding any underlying conditions.
The bottom line(s): Educate yourself on the data, but know that every person is unique. Have a conversation with your doctor if you're considering any of these procedures. Do what's right for you and your body.
Step 1: Egg retrieval
The IVF journey will always begin with egg retrieval, whether it be from you (if you're a person with ovaries) or an egg donor. We wrote an extended guide on how egg retrieval works and what you can expect at different stages, but here’s a quick summary of the main steps:
You take hormonal medication to encourage follicle development. Rather than the typical one or two follicles developing during the first half of the menstrual cycle, many may develop. The amount of medication used for ovarian stimulation is decided on by a combination of ovarian reserve and age. To get an estimation of ovarian reserve and to help figure out medication dosing (to reduce the chances of things like ovarian hyperstimulation syndrome, or OHSS), reproductive endocrinology and infertility specialists (aka REIs, the fertility specialists) will often measure anti-Mullerian hormone (AMH), a hormone that's made in the ovarian follicles.
The growth of these follicles is monitored via transvaginal ultrasound and blood work. This information is used to determine when follicles reach maturity and when the best day for an egg retrieval procedure will be.
Before ovarian stimulation, one of the last hormonal medications given is called the "trigger shot," which "triggers" the final stages of maturation for the developing follicles.
The doctor retrieves the eggs before they are released for ovulation. For the egg retrieval procedure, doctors use a transvaginal ultrasound and a needle to get the developed eggs. (P.S. You’ll likely have sedation and/or pain meds to help you through this.)
People who undergo an egg retrieval have a couple of options for next steps at this point. They could freeze their eggs to be used in the future, or proceed to what we're calling step 2 here: egg fertilization. Those who decided to freeze their eggs right after retrieval will eventually go to this next step, after their eggs are thawed once they're ready to be used.
Step 2: Egg fertilization
At this step, fresh or thawed eggs are ready to meet their partner in crime: sperm that carries the second set of chromosomes for the embryo. There are two main ways this can be done, each with its own pros and cons:
"Conventional" insemination: A single egg along with thousands of sperm are placed in a petri dish in the lab. The embryologist will then do a "fertilization check" the following day to determine how many eggs were fertilized.
Intracytoplasmic sperm injection (ICSI): Rather than waiting for a single sperm to fertilize the egg, ICSI involves an embryologist choosing a single, motile, normal-appearing sperm and injecting it into the egg, forcing that fertilization to occur.
Conventional insemination is the cheaper option, though it's not the best option for all cases. For example, when "male factor" infertility is suspected to be at play, ICSI might be recommended because it circumvents possible issues introduced by low sperm count or motility. Other times when ICSI may be recommended include in couples with unexplained infertility, those whose eggs were previously frozen, or those electing to genetically test their embryos (more on that below!).
Step 3: Embryo development
Next, embryos go through development for five or six days post-fertilization to make it to the blastocyst stage — which means the embryo is ready for transfer, freezing, or genetic testing followed by freezing. At this point in embryo development, the 100ish-cell blastocyst has developed two distinct cell types: one which will form the baby (called the inner-cell mass) and one which will form tissues and structures necessary for pregnancy, like the placenta (called the trophectoderm).
Eggs retrieved from people over 40 are more likely to result in embryos with genetic abnormalities that don't make it to the blastocyst stage, and this is often part of what scientists and doctors are referring to when they talk about egg quality. This is why using donor eggs can be a great option for some people. Though egg quantity (aka ovarian reserve) can be estimated via ultrasound or AMH, currently, egg quality cannot be estimated — the best predictor of egg quality we have right now is a person's age.
However, one tool can help us better understand the health and disease profile of a blastocyst before it gets transferred to the uterus: preimplantation genetic testing (PGT). While PGT isn't used in the majority of IVF cycles, its use continues to increase in the US — with some recent data suggesting PGT is used in 27% of all IVF cycles in the US.
There are several different types of PGT, and the type used depends on the specific question you are hoping to answer:
PGT-M ("M" is for monogenic): Curious whether the blastocyst has two variants associated with a genetic disease, if both you and your reproductive partner are carriers? PGT-M is your go-to.
PGT-A ("A" is for aneuploidy): To double-check the number of chromosomes is "normal," then you would use PGT-A.
According to Dr. Temeka Zore, MD, FACOG, a fellowship-trained reproductive endocrinologist and Modern Fertility medical advisor, PGT is typically paid out of pocket — though some insurance providers may cover genetic testing of embryos. In the rare event that coverage is offered, it may only be an option if both reproductive partners are carriers of a monogenic autosomal recessive disorder (like cystic fibrosis). The average out-of-pocket cost of PGT is $3,000-$5,000, depending on the testing platform you're using and the number of embryos being tested.
Step 4: Transfer and implantation
At this step, the blastocyst (or multiple blastocysts, depending on what you and your doctor decide) is transferred to the uterus with the hope that it'll implant in the endometrium. Soon after this implantation, blood levels of human chorionic gonadotropin (hCG) start increasing, which is the hormone detected in pregnancy tests.
How successful is IVF overall?
Because there are so many steps and decision points between egg retrieval and a live birth, it's tricky to point to a single number to best communicate your chances of success. However, we can get a sense of success rates at each step in the IVF funnel — and for the entire procedure to eventually end in a live birth.
How many eggs will be retrieved?
Though your doctor might retrieve a certain number of eggs, only some of those eggs are mature enough to be used. Both the total number of eggs retrieved and percent of those eggs that are mature depend on age to varying extents.
According to one study:
People who were 35 years old or younger had about 14 mature eggs retrieved in one cycle on average.
40-year-olds had about eight mature eggs retrieved on average.
Overall, the average total number of eggs and total number of mature eggs retrieved for people decreased significantly as age increased.
(By the way, more eggs isn't always necessarily better — the probability of eventually having a live birth plateaus at about 15 eggs.)
Small (but important!) caveat here: Just like with many other aspects of health, there's variation between people when it comes to the number of eggs you have as you age. While some may experience steep declines in egg quantity, that decline may be much more gradual for others.
How many eggs will be fertilized?
Regardless of whether "conventional" insemination (a single egg with many sperm in a petri dish) or ICSI (an embryologist injects a single sperm into the egg) is chosen, Dr. Zore says we can expect that about 75% of the mature eggs will get fertilized and make it to the initial embryo stage.
Of the mature eggs that are successfully fertilized, about 80% of them will make it to the day 3 embryo stage. The number of day 3 embryos that then make it to the final step before transfer, the day 5 or 6 blastocyst stage, can vary significantly based on the clinic, age of the egg and sperm, and possible causes of infertility. (This is why doing your research on clinics is so important — more on that below!) That said, Dr. Zore puts the percentage of mature retrieved eggs that get fertilized, make it to the day 3 embryo stage, and ultimately to the day 5 or 6 blastocyst stage at around 30%-50%, depending on age and other infertility factors.
How likely is it that a blastocyst will implant?
Not all blastocysts that are transferred to the uterus will actually implant. Blastocysts that are genetically normal ("euploid" in medical-speak) are more likely to implant and result in a live birth. Age plays a role in how many blastocysts will be euploid and thus more likely to implant and result in a live birth: Dr. Zore tells us about 75% of blastocysts will be genetically normal for 28-year-olds, 50% for 38-year-olds, and 25% for 42-year-olds.
But while the percentage of blastocysts that are genetically normal decreases as age goes up, implantation rates and live birth rates of genetically normal blastocysts don't change with age, according to Dr. Zore and data from Spring Fertility (as well as other studies). Each "normal" blastocyst has about a 55%-65% chance of implanting and resulting in a live birth per Dr. Zore. Like many other metrics in the IVF funnel, these percentages vary across clinics, so it's good practice to ask your doctor about their clinic success rates.
National data on IVF success rates
The Society for Assisted Reproductive Technology (SART) publishes comprehensive yearly reports that aggregate IVF data from all US clinics that provide information on outcomes. SART calculates success rates based on your chances of a live birth if you were to do one egg retrieval and publishes both cumulative success rates and initial success rates:
Cumulative success rates represent how likely someone is to eventually have a live birth from a single egg retrieval cycle (wherein doctors will retrieve as many eggs as they safely can) and one or more embryo transfers. Many people who do IVF may need to do more than one transfer in the event that they are not pregnant after the first one — and some may ultimately do more transfers with banked embryos for subsequent pregnancies.
Initial success rates represent how likely it is for one egg retrieval and the first, initial embryo transfer to result in a live birth.
Let's start with some of the highlights on cumulative success rates from SART's latest report, based on data from 2018:
For those under 35, the chances that one egg retrieval cycle will
For people ages 35-37, this falls to 40.8%.
For people ages 38-40, the rate is 26.8%.
For people ages 41-42, it’s 12.6%.
For people ages 43 and over, it’s 3.9%.
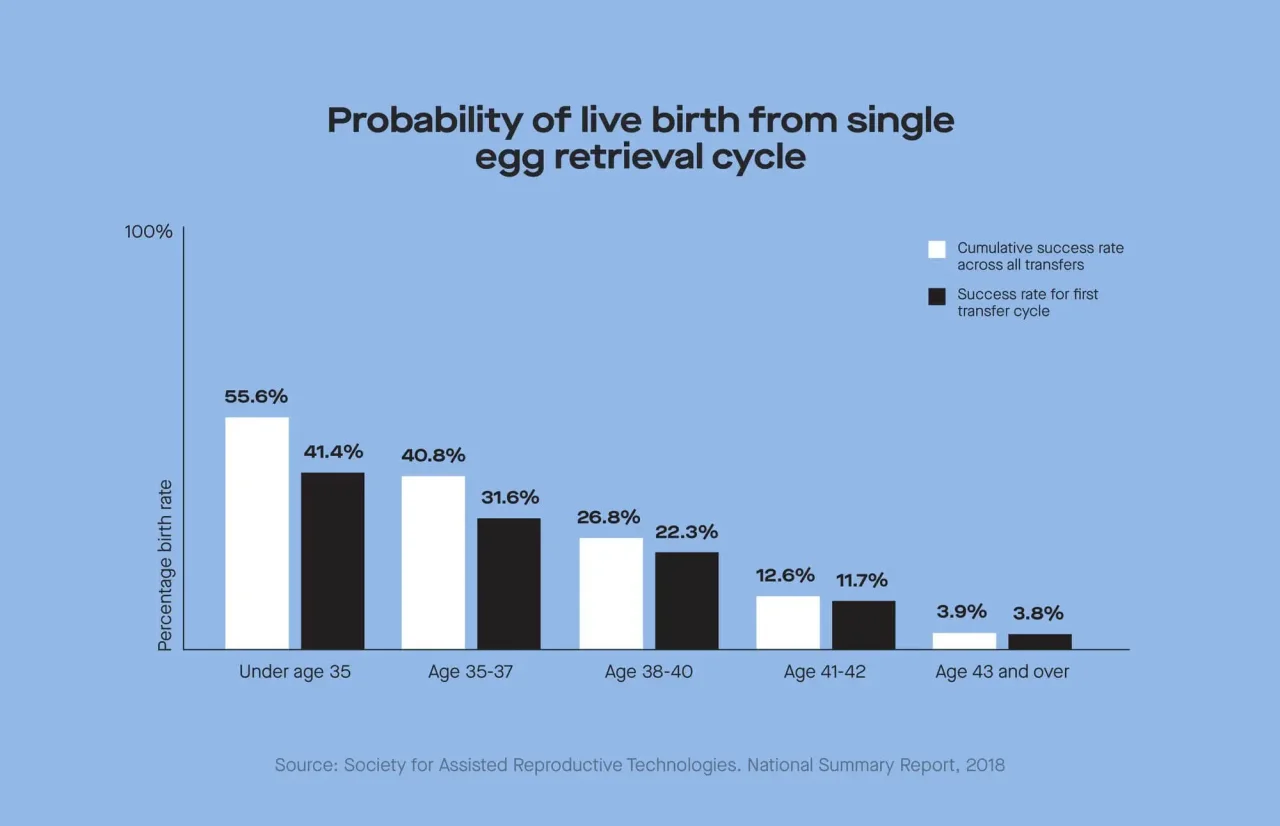
Now for initial success rates (the live birth rate per one egg retrieval and one embryo transfer is often lower because it's only accounting for that one initial transfer):
For people under 35, the chances that the first transfer cycle leads to a live birth is 41.4%.
For people ages 35-37, this falls to 31.6%.
For people ages 38-40, the rate is 22.3%.
For people ages 41-42, it's 11.7%.
For people ages 43 and over, it’s 3.8%.
Note: These numbers don't take into account preimplantation genetic testing.
It’s impossible to know your chances, but data can help you estimate them
Because there are so many factors that influence success rates, it's impossible to tell any individual person exactly what their chances of having a live birth through IVF will be. However, there are some prediction tools built using real-world data that may help you get a ballpark of what your success rates may be:
SART has a prediction tool based on data from 500,000 fresh embryo transfer cycles. This tool uses information on any fertility-related diagnoses you and your reproductive partner may have, number of previous pregnancies, and age.
Spring Fertility has an egg freezing calculator based on two published studies that allows you to input your age and number of mature, frozen eggs to get an estimate of your probability of one live birth versus two or more live births from those eggs. This tool may be helpful if you're deciding on whether you'll do one round of egg freezing or whether you may need additional cycles.
If you're a fertility nerd like we are, you'll probably spend a good bit of time playing with these tools and seeing how different factors can affect predicted chances of success (RIP afternoon productivity). Keep in mind that because these tools are based on different data sources, from different populations, and from different clinics, your predicted success rates from the two may differ.
Can you increase your chances of IVF being successful?
Just like the case of success rates when it comes to conception outside the context of IVF, there isn't any magical supplement, behavior, or trick to guarantee someone's IVF journey will end in a live birth. That being said, there are actionable steps you can take to tilt the odds in your favor:
If you're going to freeze eggs or embryos, sooner is better than later. Because both egg quality and quantity decrease with age, it's better to undergo an egg retrieval sooner rather than later.
Do your research on clinic success rates. Though the actual procedures done by fertility clinics don't vary extraordinarily widely, there are differences in success rates across clinics. Individual clinics should be able to provide you with information on their success rates. The CDC also collects and publishes clinic-level data, as does SART, which you can use to make an informed choice about where to go.
Promote your physical and mental health. Behaviors that negatively affect general physical health, such as smoking, have been shown to reduce the likelihood of IVF success. On the flip side, interventions to decrease mental stress like acupuncture may improve IVF success rates.
Understand underlying conditions. Certain conditions may decrease IVF success rates in different ways. A diagnosis of diminished ovarian reserve (DOR) means someone is likely to yield a lower number of eggs after an egg retrieval procedure than someone with a "normal" ovarian reserve, meaning it may take them more than one cycle to achieve the desired number of embryos. "Male factor" infertility (infertility caused by issues with sperm production or quality) decreases the likelihood that conventional fertilization will be successful, meaning an option like ICSI could be more successful. Understanding these sorts of underlying conditions, as well as if there's anything that can be done to minimize their effects on your chances of a live birth, can help you make more well-informed decisions throughout the process.
Is there a relationship between AMH and IVF?
Your AMH levels come into play when thinking about egg retrieval. This is because AMH levels are a strong predictor of how many eggs can be extracted as well as your response to stimulation during IVF. Whether your levels are high or low, they can give you more info to help you make decisions about whether egg retrieval is something you want to do (there's always the option of donor eggs), and if yes, when.
Birth doula and writer English Taylor used her AMH levels to think about proactively freezing her eggs. As she explains, "By freezing my eggs now (with higher AMH levels), I could be saving my future self some major dough." Why's that? Because our levels decline as we age, more egg retrieval rounds may be needed later in life to get viable eggs.
But for those with high AMH levels and/or PCOS, egg retrieval could come with some risks. Higher levels of AMH increase your chances of ovarian hyperstimulation syndrome (OHSS) after taking hormones for egg retrieval. These days, the risk for OHSS now is lower than before because we know of the potential risk factors, like PCOS, and AMH levels are now used to individualize retrieval-prep hormone protocols.
Whether or not AMH is related to the chance of an embryo transfer resulting in a pregnancy is still up for debate. Some studies suggest AMH predicts IVF success in older, but not in younger, people undergoing IVF. Others find that among people with low AMH undergoing IVF, there's no relationship between AMH and pregnancy. So, the jury is still out on whether AMH is related to IVF success rates, beyond its influence on the number of eggs retrieved.
Psst: Keeping tabs on your AMH levels over time may give you some insight into what that age-related decline in egg quantity looks like for you specifically.
Bottom line: You do you, with the right information in hand
There is no one-size-fits-all recommendation for whether IVF is a good way to help you achieve your reproductive goals. What we can tell you is this:
The quantity and quality of eggs you have decreases as you age, making your late 20s and 30s the best times to retrieve your eggs to maximize the number you'll likely get and the likelihood they will be genetically "normal."
Success rates of IVF go down with age too, but at no age does using any combination of fertility treatment options guarantee a pregnancy or live birth.
Here's one recommendation we can confidently get behind: Get familiar with the numbers. Whether they’re the numbers on success rates at different clinics, on your estimated chances of egg freezing success, or on what your ovarian reserve may look like, you deserve to have as much information as possible when making important reproductive decisions. So get out there and get that knowledge!
This article was medically reviewed by Dr. Temeka Zore, MD, FACOG, a fellowship-trained reproductive endocrinologist and infertility specialist and board-certified OB-GYN at Spring Fertility in San Francisco.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.










