Okay, real talk - do you ever pee when you, uh, weren't planning on it? Are you wondering why everyone you know is obsessed with kegels? We sat down with Pelvic physical therapist Rachel Gelman to talk about her equally interesting and important line of work, the myths and stigmas around urinary incontinence (the involuntary loss of urine), why the words “common” and “normal” shouldn’t be used interchangeably, and, of course, the elusive kegel. (She also explained why I pee a little when I attempt a pull-up at the gym.)
MF: Thanks for sitting down with us, Rachel. Tell us about yourself.
Rachel Gelman: I specialize in treating pelvic floor dysfunction in men and women at the Pelvic Health and Rehabilitation Center in San Francisco. As a pelvic floor physical therapist, I treat patients with a myriad of symptoms. I’m passionate about educating the community about pelvic health and, in my free time, I write and consult for various sex positive businesses, including Lioness, Unbound, Tabu, and Lelo.
MF: “Pelvic floor physical therapist”—what a fascinating title. Can you tell us more about what that means?
Rachel Gelman: Pelvic floor physical therapy focuses on the pelvic floor muscles. These muscles support the bowel, bladder and bladder muscles, and prostate or uterus. If the pelvic floor muscles become dysfunctional, it can lead to bowel, bladder or sexual dysfunction or pain. My patients report symptoms like urinary urgency and frequency, urinary incontinence, pain with sex, constipation, or penile and vaginal pain. This is by no means a comprehensive list.
What makes pelvic floor physical therapy so specialized is that the pelvic floor muscles can only be examined and treated internally. This means we treat these muscles via the vagina or the rectum. We also look at all the structures that attach to or relate to the pelvis, just as a “regular” physical therapist would do. This may include assessing the muscles and soft tissue in the abdomen, back, hip, or buttocks.
MF: Let’s talk more about urinary incontinence. What is it and what are the symptoms?
Rachel Gelman: Urinary incontinence is the involuntary loss of urine. So, a person urinating when they don’t want to. There are two common types of urinary incontinence. Stress urinary incontinence is when someone reports that they leak urine with certain activities—think coughing, laughing, sneezing, or jumping due to increased abdominal pressure. Urge incontinence is having a sudden urge to urinate. This is caused when the bladder muscle begins to contract and signals a need to urinate, even when the bladder is not full.
MF: I definitely pee a little when I try to do pull-ups at the gym. Does incontinence occur more frequently in certain folks? It's sometimes portrayed as something just elderly or postpartum women struggle with.
Rachel Gelman: Anyone can experience urinary incontinence—men, women, children. Literally, anyone. There can be many things that can cause or contribute to their symptoms, so it’s not just something that happens to the elderly or postpartum people.
MF: What are the most common causes of urinary incontinence? Are there any risk factors?
Rachel Gelman: Pelvic floor dysfunction is a common cause. Pelvic floor muscles support the pelvic organs, including the bladder. If they are not functioning correctly, either not contracting or relaxing when they should be, it can lead to urinary incontinence.
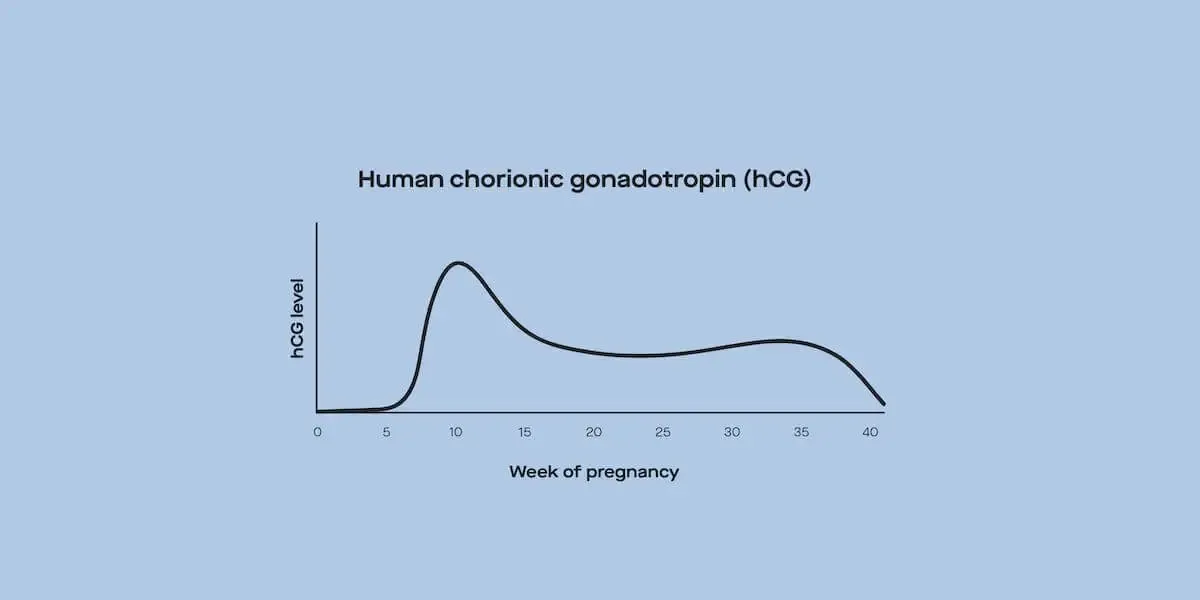
Certain life events and lifestyle changes can make someone more prone to leaking, such as pregnancy, childbirth, and menopause. Childbirth can result in pelvic floor dysfunction, for example. After delivery, the vulvar tissue and the periurethral tissue—the tissue surrounding the urethra—are also impacted by hormones. A woman’s estrogen levels are very low after childbirth. As a result, that vulvar tissue can be more dry, which may result in things like vaginal dryness, pain with sex, and incontinence. The same is true for those that have gone through menopause—estrogen levels decrease over time. When that vulvar and periurethral tissue is lacking estrogen, it doesn’t function as well. This may result in symptoms like incontinence.
Having a high BMI can also be a risk factor, as increased weight will lead to more pressure on the bladder and pelvic floor muscles. Research shows that diabetes, smoking, and hysterectomy are other risk factors.
MF: As a pelvic physical therapist, how do you work with patients to improve urinary incontinence?
Rachel Gelman: It depends on the person's symptoms and what is found during the physical exam. They may include manual therapy or training to learn how to properly contract and relax the pelvic floor. A patient may be given exercises to do at home to maintain and manage what is done in an appointment.
MF: So, all we hear these days are "kegels, kegels, kegels"—they’re pretty much in every headline. What's your perspective on kegels as they relate to urinary incontinence?
Rachel Gelman: For some reason, people seem to think kegel exercises are the cure to any problem relating to the genitals, and that’s not the case. Anyone who is experiencing signs of pelvic floor dysfunction, such as urinary incontinence, should consult a pelvic floor specialist before starting to do kegels.
If someone comes in with incontinence and upon a physical exam they have a very tight pelvic floor, kegels would not be appropriate. If a muscle is already at its end range of motion, having someone contract it further will only add fuel to the fire. Imagine if you have a cramp in your calf muscle and someone told you to do a bunch of heel raises. That may not feel great and may make the spasm worse. Hence, kegels are not always the answer.
All kegels are not created equal. The pelvic floor muscles have both fast and slow-twitch muscle fibers. So, sometimes a person needs to work on endurance versus strength. Often, a patient may need to learn how to properly relax their pelvic floor in addition to contracting it. Doing a 50 pound bicep curl is great, but you need to be able to put the weight down afterwards and let the muscle relax. Same with pelvic floor exercises.
Research shows that most people are unable to do a proper kegel with verbal instruction alone, and that most people do them incorrectly. Seeing a pelvic floor specialist can help.
MF: There can be stigma and feelings of isolation surrounding urinary incontinence—one might think that it's shameful or uncommon. What are your thoughts on this, and how can we create more acceptance and understanding?
Rachel Gelman: The more we stop thinking of incontinence as a problem that can’t be addressed, the better. I see ads for pads and diapers that make it sound like once someone starts leaking, that’s it. There’s no way to make it stop. Or you often hear people say, “Oh, leaking is just what happens when you get old,” or, “Of course you have incontinence, you had a baby, that’s what happens!” We need to let people know that leaking urine does not need to be their new normal. Hearing, “Oh, you are leaking, there are things you can do for that,” leads to follow-up questions and actual discussion. I often tell patients what they are experiencing is common, but doesn’t have to be normal. I think we often use common and normal interchangeably. That’s a problem.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.