Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
If you’ve tested your hormones with us and received your Modern Fertility results, you’ve probably noticed that there is a reference range for each hormone you test on your report.
You might be wondering, “what’s a reference range?” or “what does it mean that I am inside or outside of the reference range?” If you are pondering these things, you’ve come to the right place. This post will be a deep-dive into answering the following:
What is a reference range?
How are reference ranges calculated?
How do doctors use reference ranges?
What are Modern Fertility’s reference ranges?
How should you use and interpret the reference ranges in your report?
If you are looking for a tl;dr version, here are the key takeaways from this post:
Reference ranges are the range of values for a physiological measurement (in this case, hormone levels) for the middle 95% of the healthy population.
They comprise an upper and lower limit, and values outside those limits might indicate a health issue.
Doctors compare your results to the specific reference ranges of the lab where you were tested to make clinical decisions regarding treatment.
Reference ranges can be lab and test-specific, so you cannot necessarily mix and match ranges from different places.
What is a reference range?
A reference range is a set of values that includes upper and lower limits of a lab test based on a group of healthy people. However, not all healthy people are exactly the same, so you wouldn’t expect them to have exactly the same hormone levels. A reference range (sometimes called a reference interval) represents the hormone levels of the middle 95% of the healthy population.
How are reference ranges created?
You might be thinking, “Ok, that’s great, but how do you determine the hormone levels of the middle 95% of the healthy population?” So pleased you asked! The Clinical and Laboratory Standards Institute (CLSI for short) sets the best-practice guidelines for lab testing and recommends that at minimum, you sample 120 healthy people.
It is very important that you select a large enough group of people to capture the normal variability of the measure you’re trying to reference. That is because the healthy range of hormone levels depends on a number of factors, such as sex, age, height, weight, body mass index (BMI), ethnicity, even the time of day and the season in which you collect your sample. Since people vary, “normal levels” vary and clinicians use ranges instead of exact numbers. For example, if you are 5 feet tall and 100 pounds, it would make more sense to be in the lower end of the range for a hormone like testosterone. If you are 6 feet tall and 175 pounds, you may be at the higher end of the range.
What does it mean that I fall in the high or low end of a reference range
It’s important to consider several factors when thinking about where you land in a reference range––especially that being “higher” or “lower” in the range isn’t necessarily better or worse. As mentioned above, there are lots of reason that could explain where you fall within a range. Also, if you fall outside of the healthy reference range, it might not be of immediate concern. You might be one of the healthy people (5%) that is statistically outside the calculated reference range (remember, it only represents the middle 95% of healthy people). Or, it could be that the 120 people that were tested to determine the range did not include anyone like you. After all, 120 people is still a very small subset of the population. However, it is still not a bad idea to chat about next steps with your doctor if you fall outside the reference range, especially if your values are far outside the normal range.
Exclusion Criteria
To illustrate how a range is created, let’s pretend we are creating a range for the hormone prolactin. When creating a reference range, you don’t want to include just anyone in your study. It is crucial to exclude people who have conditions that may put their hormone levels outside the “normal” reference range. When you create a reference range for prolactin, you need to sample at least 120 people, making sure to exclude women who are pregnant or breastfeeding––known conditions that raise one’s prolactin levels. You would also want to exclude anyone taking medication that might change their prolactin levels, or anyone who has prolactin-secreting tumors.
Categorizing reference ranges
Not only are reference ranges condition-specific, but they can also be age- or sex-specific. Back to our prolactin example: men and women have different prolactin levels, so prolactin reference intervals are broken up by sex: one for women and one for men. Another common reason for creating multiple reference ranges is to split them up according to age. Prolactin is lower in older women who are postmenopausal, so two ranges are created for women: pre and postmenopausal. Age can also be broken up into groups of children vs. adults, by specific age, or by 5 year age intervals.
Reference ranges can also be condition-specific. You can make a separate reference range of pregnant women, for instance, by testing at least 120 pregnant women. Other factors, such as fasting, can affect your prolactin levels, so you can also create a fasting and non-fasting reference interval. The ways in which you decide to create your reference ranges all depend on clinically relevant categories for the measure for which you are creating the interval.
Sample Type
Reference ranges will also change depending on the type of biological sample you are testing. You can measure testosterone in serum and saliva, for example, but the concentrations of testosterone are different in those bodily fluids. That means that reference ranges are also sample-specific.
Specific ranges for tests and labs
Great, you’ve sampled at least 120 people who are healthy and thus represent your normal population. Now what? Now you chose where and how to test those samples. The most common way to measure prolactin in blood is through an immunoassay, so that makes the choice simple. For other hormones, such as testosterone, you might have multiple measurement options (e.g. immunoassay or mass spectrometry).
Now that you have chosen how to measure your prolactin samples, you will need to choose which brand of immunoassay to use. There are several on the market. For example, at Modern Fertility we measure prolactin using the Siemens Centaur XP immunoassay system for the in-lab test and for the at-home test we measure prolactin on a machine called the Beckman Coulter DxI800 immunoassay system. Because these are slightly different tests that were developed in slightly different ways, they will not give exactly the same results. And indeed, both of these immunoassays have their own reference ranges for prolactin.
Here is a picture of a fancy immunoassay machine!

Photo: Advia
One way to ensure that labs are up to snuff, and that the differences in measurement are not because of lab error, is to check if labs are CLIA and CAP certified. CLIA stands for Clinical Laboratory Improvement Amendments and is a program run by the U.S. federal government. CAP stands for College of American Pathologists and is an independent organization of board-certified pathologists. To be CLIA certified and CAP accredited a lab must meet very stringent regulatory requirements, ensure compliance with comprehensive standards, prove the accuracy of their results, and be inspected every two years. Only 16,158 labs in the entire U.S are CLIA certified and 8,027 are CAP accredited. Both of the labs that Modern Fertility uses are CLIA and CAP accredited.
Statistically determining the range
Once you have measured your 120 samples, you will then create the 95% reference interval based on your results. This interval is going to exclude the bottom 2.5% and the top 97.5% of people that you tested. Your reference range is then the values that fall between the lower 2.5% of the population and the upper 97.5% of the population.
The distribution looks like this:
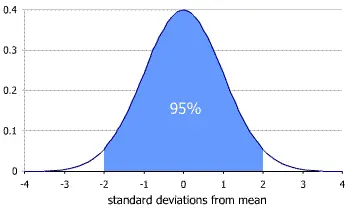
Photo: Tristanb, Wikipedia
How do doctors use reference ranges?
Clinical decision limits vs. reference rangesUnlike reference ranges, clinical decision limits (CDLs) are threshold values above or below which a doctor might recommend an intervention or treatment. A classic example that illustrates the difference between reference intervals and clinical decision limits is found in cholesterol. If you go through the steps above to define a reference range for cholesterol in the US, even if you try to exclude people with cardiovascular disease, you are still going to have people in your “normal” range with high enough cholesterol that a doctor would recommend treatment. For context, the 97.5% reference range for cholesterol concentration is 280- 300 mg/dL. However, the National Cholesterol Education Program defines borderline high cholesterol as those values that fall between the 50th and 75th percentile, or 200 mg/dL to 240 mg/dL and high cholesterol any value above 240 mg/dL. This range is based on clinical outcome studies that show that these values correlate to moderate and high risks for the development of cardiovascular disease.
In this sense, having a cholesterol value that is “normal” (i.e. within the 95% reference range) does not mean that you are in the clear from a health perspective. Every test, including hormone tests, will have a reference range as well as ranges where a doctor may or may not decide to do something, such as ordering more tests or deciding on a treatment plan.
Modern Fertility's reference ranges
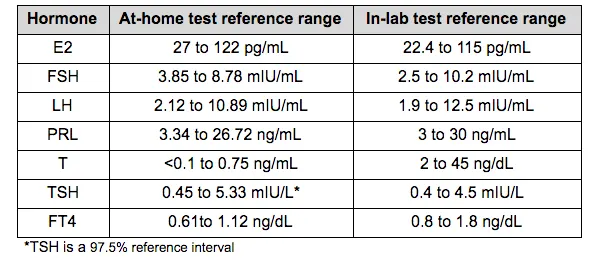
Whew! That was a lot of talk about creating reference ranges. Now, let’s dig into what our reference ranges actually are.
Below, you can see the two different reference ranges that Modern Fertility currently uses for our two different types of test. You can also see these ranges if you download the PDF of your results in your dashboard. You will notice that the ranges for the at-home test and the in-lab test are very similar, with slight differences (for example, testosterone is presented in different units at the two labs). This is because the two different tests use different different labs and equipment, as described above.
As you’ve already learned, it is important that certain reference ranges be age-specific. AMH is a great example of this. AMH decreases with age, so a “normal” level for a 40-year-old would not be considered “normal” for a 20-year-old. Below are the two different Modern Fertility reference ranges for AMH in women, broken out by age. (Note: as of August 2018 the in-lab reference range changed for some people because the lab was phasing in testing on the same assay as the at-home test. Check your results PDF accessible in your dashboard to confirm your reference range.)
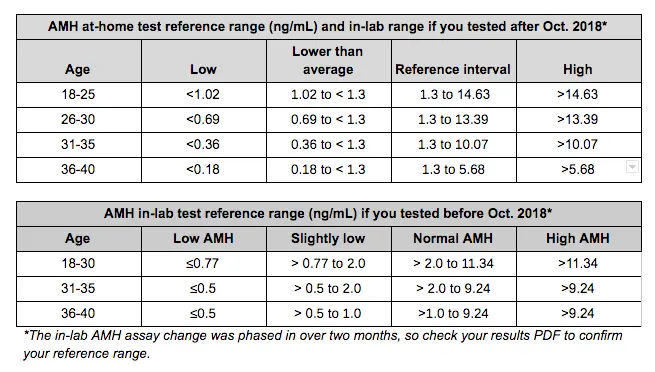
We have also incorporated similar nuance to clinical decision limits in our ranges for AMH. You’ll notice that there’s a “lower than average” and a “slightly low” category for the at-home and in-lab tests, respectively. These “slightly low” ranges are actually within the 95% reference range, but are low enough that they might have implications for fertility. The cut-off of 1.3 ng/mL of AMH is from on the European Society of Human Reproduction and Embryology (ESHRE) updated Bologna criteria, which established a range of AMH cut-offs for poor ovarian response based on a survey of peer-reviewed scientific studies.
For example, if you are 28 years old, did the at-home test and your AMH level is between 0.69 and 1.3 ng/mL, you are in the 95% reference range which is reassuring. However, your AMH is low enough that, for example, you might collect a fewer number of eggs in IVF or egg freezing. This is much like the cholesterol example above, where you might still be in the reference range, but your levels are high enough to be important for your health.
Using reference ranges
Once you have your hormone results in hand, it might be tempting to google what those levels mean. However, don’t forget that if you find a website that discusses a “normal” result for a certain hormone, that result is “normal” according to the lab that tested that sample. If you did not test with the same lab, it could be misleading to compare your results to the results presented on the website.
Additionally, if you bring your results to your next doctor’s appointment, and she is not familiar with Modern Fertility, you will probably want to make sure she sees the reference range so that she has context to interpret your results. This also holds true for re-testing. If you retest through your doctor’s office or at a different lab, you won’t necessarily get the same results, even if two labs use the same assay and equipment. This could be because of variability in any number of factors: who is running the tests, the temperature of the lab, the calibration of the machines, etc. That’s not to say that if you get different results, one result is “correct” while the other is “incorrect.” They are both valid and clinically relevant, but different because they are lab- and assay-specific. This is why you need a reference range!
What if my result changes?
It’s not uncommon for results to change from one test to another, even if you test at the same lab. This is called “within individual variation.” Hormones are a great example of this. They fluctuate...a lot. For example, testosterone is higher in the morning than the evening. And you probably don’t need to be reminded that certain hormones fluctuate over the menstrual cycle. It wouldn’t be a cycle without these changes! This is why we require that you test on day 3 of your period (depending on your birth control). Because of this fluctuation, some hormones, like FSH, have specific reference ranges that correlate to different times in the menstrual cycle. And going on and off birth control will also change your hormone levels.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.









