Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
There are many good reasons to take a prenatal while you're trying to conceive. They’re formulated with the specific needs of a pregnancy and developing baby in mind, meaning they contain ingredients that support things like the baby’s brain and spinal cord development, and blood cells getting enough oxygen so everything can run smoothly.* One thing prenatals don’t do, contrary to what some might think, is actually change your chances of conceiving (as far as we know).
We dug through the literature in search of scientific evidence supporting a link between prenatals and chances of conception. To date, there have been no published, large-scale studies linking the use of prenatal vitamins or specific micronutrients with pregnancy rates or time to pregnancy — meaning there's no evidence that taking prenatals impacts your chances of conception.
Here, we’ll give you a quick breakdown of where the science stands on what prenatals can and can’t do (spoiler: they can help promote a healthy pregnancy, but they can’t change your chances of getting pregnant*), and point to some actionable steps you can take to increase your own chances of conception.
Micronutrients and reproduction: What do we (and don't we) have clinical evidence for?
We do know that the micronutrients in prenatal vitamins can support a healthy pregnancy*
Micronutrients play important roles for a whole range of physiological processes, including reproductive function — and there’s no shortage of lab studies on how micronutrients may affect processes that are crucial to conception. One prenatal micronutrient in particular, folate, is backed by decades of lab research as well as real-world effectiveness.
Multiple randomized controlled trials (the "gold standard" in the research world) have demonstrated the efficacy of supplementation of folate's synthetic form, folic acid, for supporting fetal neural tube development.* In fact, in the mid-1980s, researchers started running a study on folic acid supplementation around the time of conception, spanning 33 centers and seven countries. Their goal was to study 2,000 people, but they ended up stopping the study early because folic acid supplementation had such a large positive effect they thought it was only right to give it to all participants. That's when it was first discovered just how crucial folate is for fetal neurodevelopment.*
These findings spurred the creation of mandatory food-fortification campaigns. Folic acid began getting added to things like grains, whole grains, cereal, and flour in the US in 1996, and a decade later, the World Health Organization and United Nations published guidelines to help countries determine their folic acid fortification strategies. After folic acid enrichment of grains was mandated in the US, the prevalence of infants born with neural tube defects decreased by 36%.
Despite these fortification programs, many people in the US still do not get the recommended amount of folic acid. That's why the American College of Obstetricians and Gynecologists (ACOG), the leading body of OB-GYNs, recommends 600 micrograms (mcg) of folate per day during pregnancy — with at least 400 mcg DFE (dietary folate equivalent) coming from supplemental folate — starting at least one month preconception through at least the first 12 weeks of pregnancy. It's for the reasons stated above that virtually all prenatal vitamins you find will contain some form of folate (e.g., methylfolate, folic acid). Recent research also suggests that the B vitamin choline is equally essential in neurodevelopment, as well as for many other critical functions.*
Other micronutrient recommendations are based more so on our general understanding of fetal development and pregnancy. Along with folate and choline, ACOG recommends the following nutrients before and during pregnancy:
Omega-3 fatty acids (DHAs) help with fetal brain and retina development.*
Iron is the building block of hemoglobin — a blood protein that transports oxygen.*
Vitamin A supports good vision, healthy skin, and a functioning immune system.*
Vitamin B6 boosts protein metabolism for both you and your pregnancy.*
Vitamin B12 plays a role in central nervous system function.*
Vitamin C makes it easier for your body to absorb iron.*
Vitamin D3 increases absorption of calcium from food.*
Iodine is important for thyroid hormones and thyroid health.*
Calcium strengthens fetal teeth and bones.
Research also shows that taking prenatal vitamins with B6 may decrease morning sickness in pregnancy.*
We don't know if those same micronutrients can have an impact on conception
Despite all we know about how micronutrients may affect reproductive function on a cellular level, there’s a surprising gap of research on how micronutrients may affect chances of conception in humans in the real world — and, to our knowledge, there haven’t been any clinical trials run by prenatal manufacturers on whether prenatals are associated with higher pregnancy rates or shorter time to pregnancy. In terms of pregnancy loss? Studies found no association between prenatal vitamins and lowered miscarriage rates.
There have been some studies looking at whether taking multivitamins or specific micronutrients may impact chances of conception, but we’re still far from being able to say that any specific vitamin formulation or individual micronutrient actually boosts chances of conception. Until large-scale randomized controlled trials systematically compare pregnancy rates or time to conception in people who do and do not use micronutrient supplements, the jury’s out on whether they have an effect.
The majority of dietary supplements that are specifically marketed as prenatals don’t make claims about their product’s ability to increase your chances of conception, but there are countless over-the-counter supplements marketed as “fertility supplements” that do claim to improve egg quality, treat infertility, “balance” reproductive levels, and promote ovulation, along with other lofty promises. While it would be great if there was scientific evidence to support these claims, it doesn't currently exist.
Scientists at the Center for Science in the Public Interest dug for evidence of effectiveness for 39 different women’s fertility supplements (you can see the full list here). A (very, very small) minority of companies referenced scientific studies, but not a single referenced study found positive effects on ovulation, time to pregnancy, or pregnancy outcomes in women.Our suggestion? Approach any supplements that make these sorts of claims with a critical eye.
What can improve your chances of conception?
Though taking a prenatal before and while you’re trying to get pregnant likely won’t impact your chances of conception, there are some steps you can take to increase those odds:
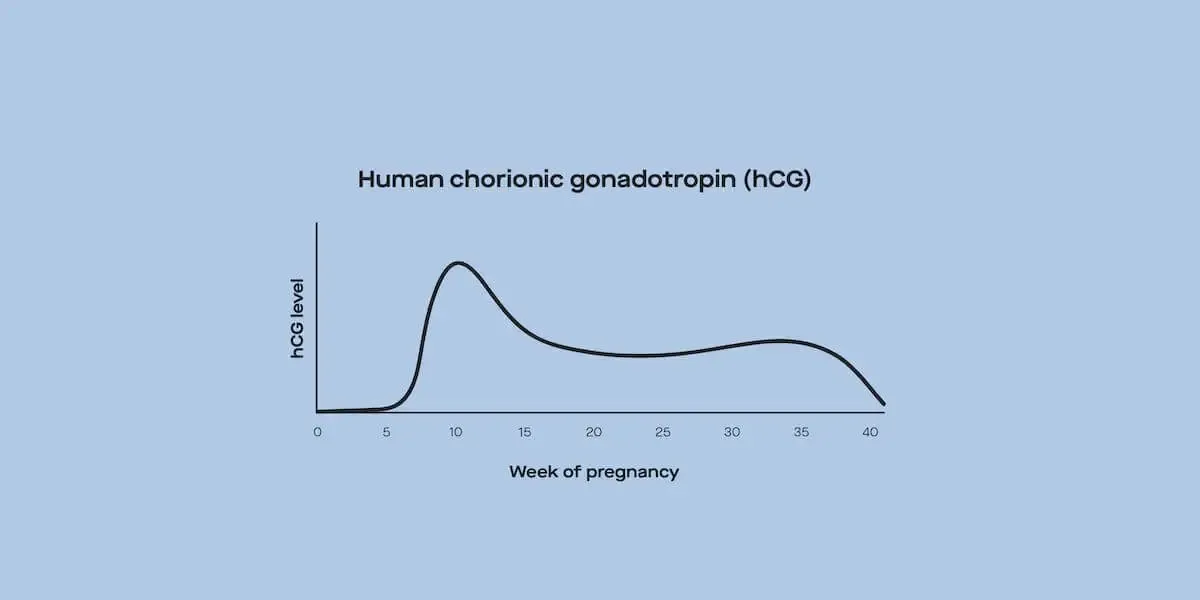
Tracking your cycle Conception is only possible during a narrow window of the cycle, with the likelihood being highest the day before ovulation itself. Because luteinizing hormone (LH) peaks before ovulation, tracking your LH can give you insight into when you may ovulate. If you’re looking for science-backed ways to track LH, we recommend using an ovulation test that measures LH.
Timing intercourse or insemination based on ovulationKnowing when your fertile window (the five days leading up to ovulation and the day of ovulation) is means you can pinpoint when intercourse and insemination are most likely to result in sperm and egg meeting.
Getting off birth control a few months early: Data show that birth control use has no long-term impact on fertility, but there are some methods associated with a slightly longer return to ovulation than others, like the implant and injectable. Because it may take a few months to get back to your pre-birth control cycles after stopping, it may be helpful to stop using birth control a little earlier than immediately before you want to start trying to conceive.
Knowing about underlying conditions: Some common conditions (that aren’t always commonly talked about!) like polycystic ovary syndrome (PCOS) and hyper/hypothyroidism are characterized by changes in reproductive hormones that in turn affect cycle regularity and ovulation. Fertility hormone testing is one way to screen for red flags for these conditions. If you have any of these conditions, it's important to talk to your healthcare provider before trying to conceive to increase the odds of getting pregnant.
Talking to your doctor about fertility-related medications Some people with the underlying conditions mentioned above, as well as some people with no detectable underlying conditions, may not ovulate regularly — which makes tracking and targeting conception trickier. There are some FDA-approved, science-backed prescription medications that induce ovulation (like Clomid and Femara), as well as some medications that weren’t invented specifically to induce ovulation (like metformin), but help regulate it all the same. Note: These medications do not increase the chances of conception in people who ovulate regularly, meaning they’re not for everyone.
Does it matter when you start to take prenatal vitamins?
ACOG’s recommendation is to start a prenatal at least one month preconception. This is because nutritional needs start changing in very early pregnancy, soon after conception — meaning it’s important to make sure you’re giving yourself enough time for nutrients to build up to sufficient levels before you can confirm whether you’re pregnant.
Here's an example: We know that the neural tube (which develops into the brain and spine) closes within the first few weeks of pregnancy (30 days post-conception to be exact). Because a good chunk of neural tube development happens before someone can even know whether or not they’re pregnant, it’s crucial that people who are trying to conceive have sufficient amounts of the nutrients that keep this process running smoothly (like folate and choline) before they can confirm they’re pregnant.*
Highlighting the importance of folate for fetal development, the Centers for Disease Control and Prevention (CDC) actually recommend that all people with ovaries of childbearing age, regardless of whether they’re currently trying to conceive or pregnant, make sure they’re consuming adequate amounts of folate, either through balanced eating or supplementation (or a combo of the two).* Their logic here is that because almost half of pregnancies in the US are unplanned, making sure that people who could potentially get pregnant are getting sufficient amounts of folate at all times.
The bottom line
Though prenatals won’t change your chances of actually getting pregnant, they can help you fill in the micronutrient gaps to support your health through pregnancy and healthy fetal development.* Pregnancy and lactation (whether or not you're breastfeeding/chestfeeding) are associated with a wide range of physiological changes that facilitate the growth and development of a baby, so it’s not a surprise that nutritional needs change during this time too. Prenatals are formulated with these changing nutritional needs in mind — making them important to have on hand before, during, and after pregnancy.
This article was reviewed by Dr. Jennifer Conti, MD, MS, MSc.
*This statement has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.