Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Your body is kind of like an info feedback loop for reproductive health, and one example of this is your cervical mucus — specifically its volume and consistency. Tracking changes in cervical mucus is one of the most effective ways to understand where you are in your menstrual cycle. Because cervical mucus creates an optimal environment for sperm in your vagina and helps the sperm travel to the egg, documenting changes in consistency and appearance each month can reveal when you have the highest or lowest chance of getting pregnant (or when cervical mucus makes it easier or harder for sperm to travel through the fallopian tube).
What is cervical mucus monitoring?
Monitoring your cervical mucus, also known as the cervical mucus method, is a fertility awareness method technique that can help you try to conceive. Aside from ovulation tests, cervical mucus monitoring is one of the most effective ways to predict ovulation so you can time sex around your fertile window.
Cervical mucus tracking can also help you to avoid pregnancy if you’ve been able to identify your “safe” days (when you are least fertile and able to get pregnant) and “unsafe” days (when you are most fertile and likely to get pregnant). Note that if you plan to use cervical mucus tracking to avoid pregnancy, it’s recommended that you’ve charted your mucus changes for at least one cycle and that you’ve sought guidance from your doctor.
Three different ways to monitor your cervical mucus
There are three different methods for recording your cervical mucus changes: the Billings Ovulation Method, the Creighton Method, and the 2-Day Method. Whether you’re trying to get pregnant or not, understanding your cycle better through one of these methods can help you note patterns and become more familiar with symptoms you experience at certain times of the month. Whichever method you choose, there are a few different ways to actually check for the changes:
Wiping your vaginal opening with toilet paper before you pee and inspecting what’s left on the toilet paper.
Noting mucus appearance, color, and texture on your underwear.
Inserting fingers into your vagina to see mucus color and feel its consistency. If you then put your fingers into a glass of water and the substance either stays on your fingers or sinks to the bottom of the glass, then it’s definitely cervical mucus — as opposed to vaginal fluids (made up of water and microorganisms) that help to keep the vagina clean.
Once you start examining your cervical mucus, what does each change mean? When can you expect to see watery cervical mucus versus creamy cervical mucus? What is fertile mucus, as opposed to infertile mucus? We’re breaking it all down for you right here.
How cervical mucus changes throughout your cycle
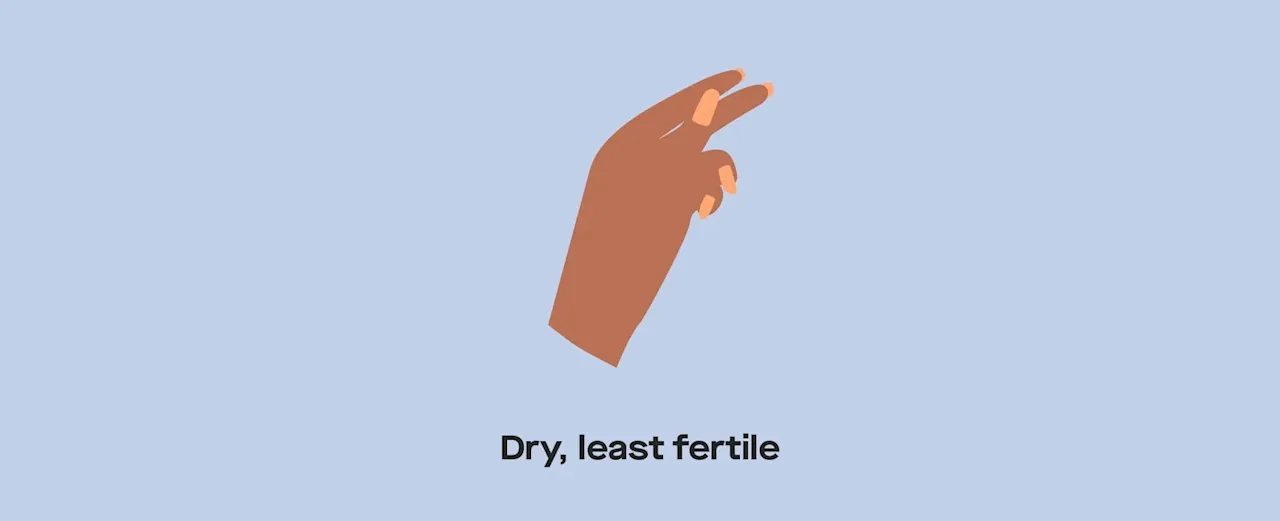
Dry, and the least fertile. This mucus is produced a few days before your period, during your period, and immediately after your period.
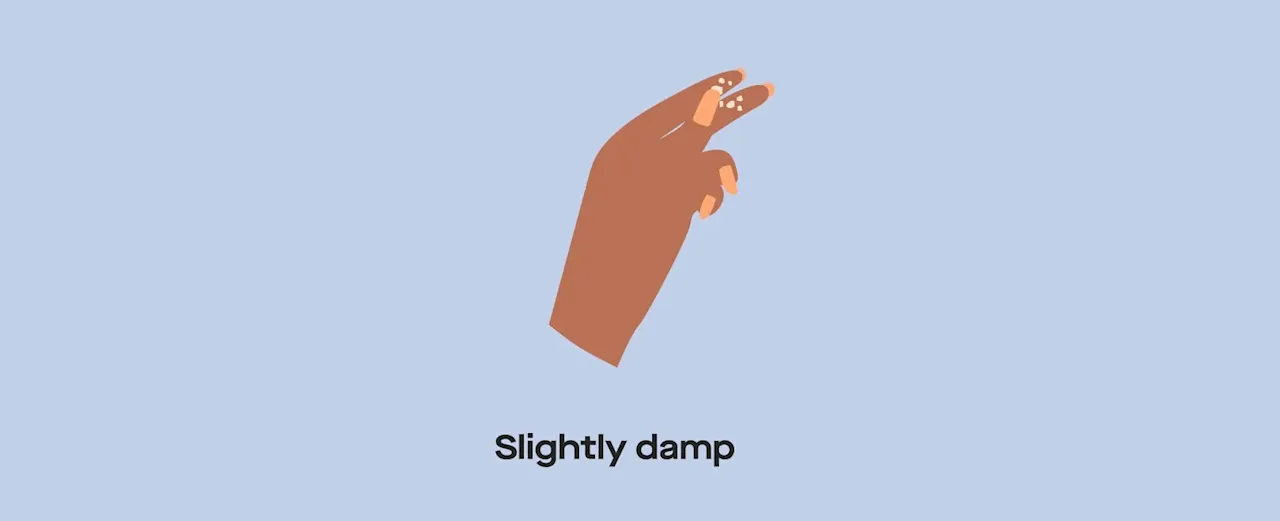
Slightly damp, low fertility. This type of mucus is produced during the first three to four days days following your period.
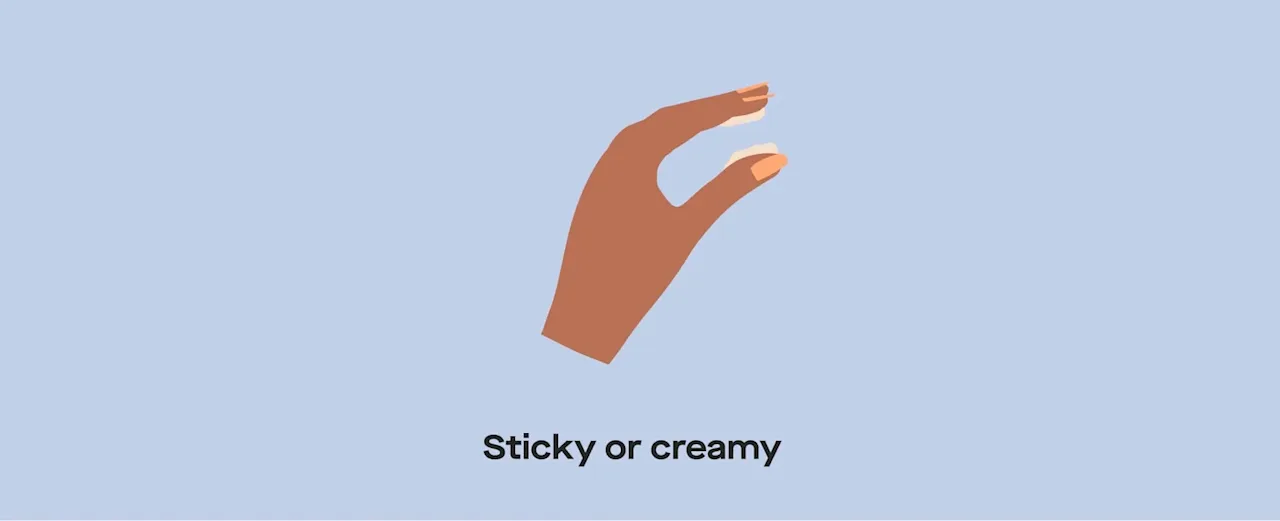
Thicker in consistency — could be sticky or even creamy. Signals intermediate fertility. This mucus is produced when one egg in one ovarian follicle fully matures (around day 10 if you have a 28-day cycle).
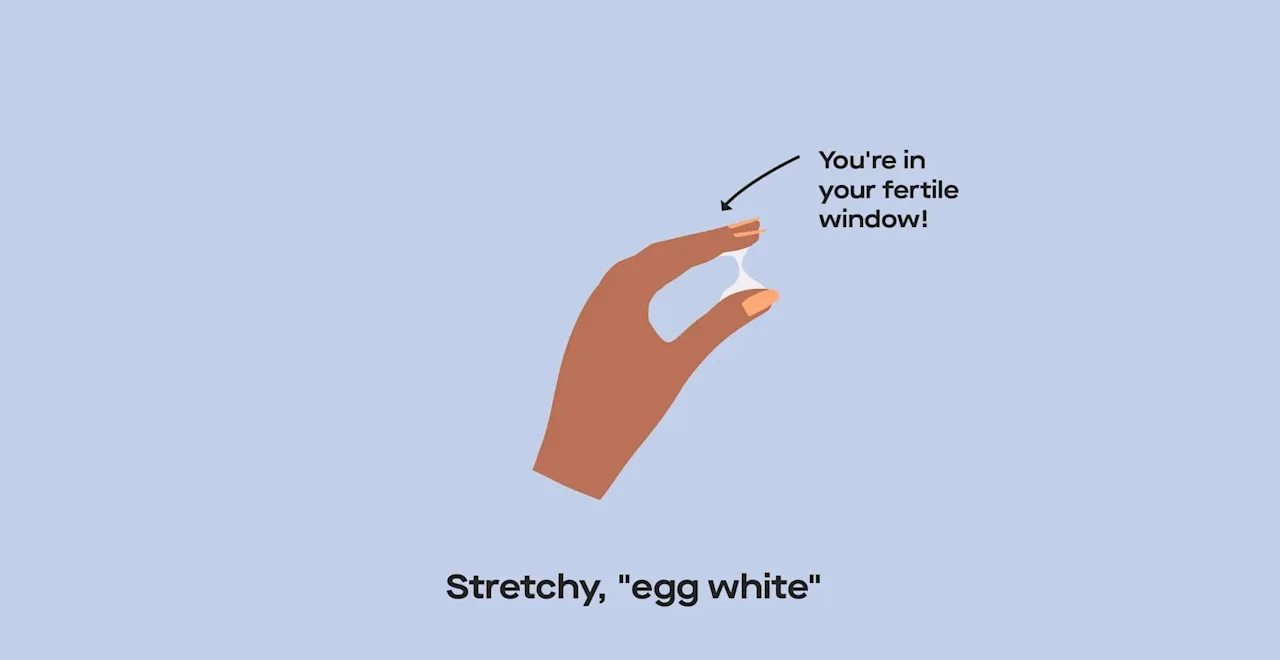
Stretchy and similar to an egg white in consistency. Indicates you’ve reached peak fertility. This mucus is produced during the days preceding your day of ovulation (day 14 if you have a 28-day cycle).
Cervical mucus before your period
Cervical mucus before your period
In the days leading up to your period, you likely won’t notice any cervical mucus, whether you’re checking for it or not. While you probably won’t observe anything on your underwear, you may notice a shiny residue on toilet paper when you wipe (this is called vaginal cell slough).
This type of cervical mucus has a dry consistency, but if you insert your fingers into your vagina, the mucus feels slightly damp to the touch before any moisture quickly evaporates. (Because the vagina is a mucus membrane, it’s never completely dry.) Once your period begins, any cervical mucus produced by your body is hidden by menstrual blood. Then, once your period stops, your body will continue producing this type of cervical mucus immediately after your period.
This type of mucus signifies your body’s least fertile time — the lack of mucus and moisture means sperm may not as easily travel through your vaginal tract.
Cervical mucus after your period
Cervical mucus after your period
During the first three to four days after your period, you still won’t see any mucus, but you’ll begin to feel a slightly damp sensation around your vaginal opening. This is more moist because of your body’s rising estrogen levels at this stage of your cycle. Still, your fertility is considered low at this stage.
Cervical mucus before ovulation
Cervical mucus between your period and ovulation
After your period and before ovulation, the dominant ovarian follicle (thanks to follicle-stimulating hormone, also known as FSH) matures a fully developed egg. If you have a 28-day cycle, this happens around day 10.
Around this same time, you may feel a wet, slippery substance around your vaginal opening. It might even feel like you just got your period. This substance looks thick and white or yellowish in color, and still feels sticky when you touch it. When you see this mucus, whether you’re tracking it via finger insertion or by what’s left on your underwear, it’s a sign that you’re entering your fertile window and have “intermediate fertility,” according to the University of North Carolina School of Medicine. Your underwear might also have a wet spot or a mark where that wet spot was absorbed into fabric.
Your most fertile cervical mucus
Cervical mucus at peak fertility
Just a few days before you ovulate, you may start to feel more wetness around your vaginal opening; you may even feel like water is flowing out of your vagina. Some — not all — people ovulate on day 14 of their cycle, and this kind of mucus shows up shortly before that day.
The substance feels damp when you touch it with your fingers and, notably, it won’t evaporate when you move your hands. It can also stretch for at least an inch between your fingers without breaking. This is the most fertile type of cervical mucus. It can look creamy, but its watery appearance is more frequently compared to raw egg whites and it may leave wet patches on your underwear that never fully dry.
This is the largest amount of cervical mucus that your body will ever produce during your cycle, and it signifies peak fertility. Studies have found that you’re most likely to conceive with this type of cervical mucus on a day before actual ovulation, and that you are two to three times more likely to conceive when stretchy “egg white” mucus is present, compared to the previous types of cervical mucus.
Cervical mucus after ovulation
After ovulation, your body starts producing less and less cervical mucus. The mucus that you do see after ovulation, whether on your underwear or on your fingers, may look cloudy and feel sticky. If you’re not pregnant at this stage of your cycle, then you will soon notice the return of drier cervical mucus — meaning you may see no mucus at all. But if you had sex with a partner who has sperm or underwent a fertility treatment, sperm fertilized your egg, and the egg implanted in your uterus, then you will start to see increased amounts of vaginal discharge because of rising estrogen and progesterone levels that accompany early pregnancy.
Is cervical mucus different for each person?
These are the most common stages of cervical mucus, but someone with a cervix won’t necessarily follow this exact timeline during their cycle. Some people may notice that their bodies produce more than one type of cervical mucus on a single day. Other people may notice their bodies never produce a certain type of mucus.
If you have a hormonal imbalance that can result in anovulation (lack of ovulation) — including polycystic ovary syndrome (PCOS), primary ovarian insufficiency (POI), and thyroid disorders — then you may produce lesser amounts of cervical mucus.
Outside factors that can also contribute to changes in cervical mucus include breastfeeding, douching (our team of medical advisors say don’t *ever* douche), recent use of hormonal birth control or Plan B, early menopause, cervix surgery, and STIs.
Tracking cervical mucus is a great, no-tech-required way to understand your body’s ovulation patterns. If you’re looking for deeper insight (and maybe a little less room for interpretation), an ovulation test can analyze your luteinizing hormone (LH) at low, high, and peak levels as you move toward your fertile window — helping you predict ovulation using your *actual* hormone levels.
This article was reviewed by Dr. Jennifer Conti, MD, MS, MSc. Dr. Conti is an OB-GYN and serves as an adjunct clinical assistant professor at Stanford University School of Medicine.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.










