Here's what we'll cover
Here's what we'll cover
If you experience painful periods, pelvic pain, infertility, or a whole host of other symptoms, you may have endometriosis. Endometriosis is a common, chronic condition in women’s health. Its effects can range from a mild disease that causes no symptoms to severe endometriosis that causes chronic pain and infertility.
Depending on the severity of your condition, you may get a diagnosis of stage I, II, III, or IV endometriosis. These stages help healthcare providers make the best recommendations for treatment.
Here’s a look at the various endometriosis stages, the differences between them, and how you can treat them.
What is endometriosis?
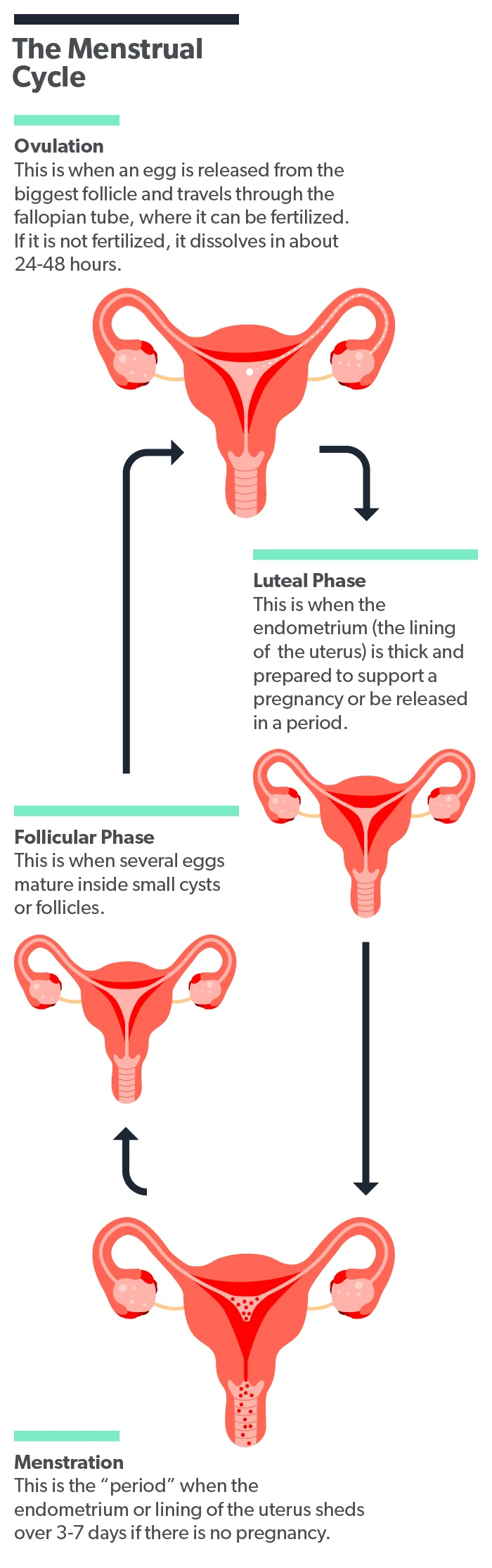
Every month, the inner lining of your uterus, called the endometrium, grows thicker in response to hormones made by your body—this is called the menstrual cycle. This cycle prepares your uterus in case a fertilized egg implants and you become pregnant. If there is no fertilized egg that month, your body will shed the endometrium as your menstrual period.
Endometriosis is a medical condition where the tissue that should only be inside of the uterus also grows elsewhere in your body. Endometriosis can occur anywhere in the body. The most common location is in the pelvic cavity in the fallopian tubes and on the ovaries. Other places in your body where endometrial tissue can appear include (Tsamantioti, 2021):
Large and small intestines
Bladder
Ureters
Urethra
Lining of the abdomen
Lining of the heart or lungs
Brain and spinal cord
Many theories exist, but researchers don’t know what causes this tissue to grow outside the uterus. They also don’t fully understand why this would cause the wide range of symptoms people with endometriosis experience (Tsamantioti, 2021).
The symptoms that you experience with endometriosis come from the fact that the endometrial tissue growing outside the uterus still responds to hormones the same way as the endometrium does. This means that each month the tissue grows and then breaks down. However, unlike the lining of your uterus, endometriosis tissue has no way to leave your body. This trapped collection of blood and broken-down tissue causes inflammation (Dydyk, 2021).
What are the stages of endometriosis?
The American Society for Reproductive Medicine (ASRM) categorizes endometriosis into four stages. These stages are minimal, mild, moderate, and severe (Hoyle, 2021).
Endometriosis stages are based on the severity, amount, location, depth, and size of the growths. Since symptoms can resemble so many other illnesses, it’s not uncommon for people with endometriosis to experience symptoms for 4–11 years before getting a diagnosis. This means that endometriosis is usually diagnosed in the more advanced stages (Tsamantioti, 2021).
The only way to accurately determine what stage of endometriosis you have is with laparoscopic surgery. This is when a surgeon makes small incisions into your abdomen or pelvis and inserts a camera. Your surgeon can see any signs of endometriosis and take biopsy samples if needed during the surgical procedure (Hoyle, 2021).
Stage I endometriosis: minimal
In stage I endometriosis, there are small, solitary lesions present. There are no significant adhesions present. Adhesions form when the scar tissue caused by the inflammation of endometriosis binds two organs together that usually aren't attached (Hoyle, 2021; Somigliana, 2012).
Stage II endometriosis: mild
Stage II endometriosis features superficial lesions (or implants) that are less than 5 cm in size. Superficial implants are those located only on the surface of the pelvic organs. There are no significant adhesions present with mild endometriosis (Hoyle, 2021).
Stage III endometriosis: moderate
In stage III endometriosis, there are multiple deep, implanted lesions. These deep implants are spots of endometriosis that have grown into the surface of the organs and can impact their function. Small endometriomas, or endometriosis cysts, are present. These lesions become filled with dark brown fluid and are sometimes referred to as "chocolate cysts." They are most commonly found on the ovaries (Hoyle, 2021).
Stage IV endometriosis: severe
In stage IV endometriosis, there are multiple deep, infiltrating endometriosis lesions. Large endometriomas are present on one or both ovaries. These ovarian endometriomas can lead to chronic pelvic pain and infertility and often require surgery for treatment. Thick adhesions may be present (Hoyle, 2021).
How is endometriosis diagnosed?
If your healthcare provider suspects you might have endometriosis, they will ask you detailed questions about your health history and perform a physical exam. You should tell your provider if you have any history of the following (Tsamantioti, 2021):
A family history of endometriosis
Pelvic pain
Ovarian cysts
Pelvic surgeries
Trouble getting pregnant
The only sure way to diagnose endometriosis is for a surgeon to use a camera to look inside your abdomen, also called laparoscopy. This surgery is an invasive procedure and might be too much for someone with only mild symptoms. Your healthcare provider will likely start with less intrusive methods like pelvic exams or special scans (Tsamantioti, 2021).
A pelvic exam can show tender points and masses of tissue that can be felt for some women. Others don’t have these present. You can still have endometriosis even if your provider doesn’t find anything with a physical exam (Tsamantioti, 2021).
Special scans such as magnetic resonance imaging (MRI) and transvaginal ultrasound can also be used to diagnose endometriosis. Ultrasound is very effective at helping providers find endometriosis tissues around the ovaries and in the pelvis and is easily performed as an outpatient (Tsamantioti, 2021).
What are the treatment options for endometriosis?
We don’t have a cure for endometriosis yet. Healthcare providers currently use various medical and surgical treatments to relieve your symptoms of endometriosis, improve your quality of life, and increase your chances of fertility (Tsamantioti, 2021).
Medications
The most commonly used medications for treating endometriosis include (Tsamantioti, 2021):
Non-steroidal anti-inflammatory drugs for pain
Hormonal contraceptives to reduce ovulation and estrogen levels
Hormonal contraceptives can include the combined estrogen-progesterone birth control pill (BCP) or an intrauterine device (IUD) containing levonorgestrel (Brown, 2014).
Gonadotropin-releasing hormone (GnRH) agonists can be considered if the other drugs don’t control your symptoms. This is a class of medications that suppresses multiple types of hormones in the body to slow down the growth of endometriosis tissues (Brown, 2014).
Surgery
Surgery is another option available to treat endometriosis. The advantage is that surgically removing endometriosis and scar tissue from your abdominal cavity can simultaneously relieve your pain and enhance fertility. However, all surgeries come with risks and complications, so it’s usually only considered when medications haven’t worked (Tsamantioti, 2021).
Assisted reproduction
If you have endometriosis, you might have a lower chance of getting pregnant than those without the disease. However, many women with mild to moderate endometriosis can still have a baby without any medical interventions. If you have more severe disease, you might need medical help to conceive. In-vitro fertilization (IVF) is a successful option for women with endometriosis (Tanbo, 2017).
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Brown, J., & Farquhar, C. (2014). Endometriosis: an overview of Cochrane Reviews. The Cochrane Database Of Systematic Reviews, 2014 (3), CD009590. doi: 10.1002/14651858.CD009590.pub2. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6984415/
Dydyk AM, Gupta N. (2021). Chronic pelvic pain. [Updated 2021 Jul 12]. In: StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554585/
Hoyle AT, Puckett Y. (2021). Endometrioma. [Updated 2021 Jun 15]. In: StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559230/
Somigliana, E., Vigano, P., Benaglia, L., Busnelli, A., Vercellini, P., & Fedele, L. (2012). Adhesion prevention in endometriosis: a neglected critical challenge. Journal of Minimally Invasive Gynecology, 19 (4), 415–421. doi: 10.1016/j.jmig.2012.03.004. Retrieved from https://pubmed.ncbi.nlm.nih.gov/22575862/
Tanbo, T., & Fedorcsak, P. (2017). Endometriosis-associated infertility: aspects of pathophysiological mechanisms and treatment options. Acta Obstetricia et Gynecologica Scandinavica , 96(6), 659–667. doi:10.1111/aogs.13082. Retrieved from https://pubmed.ncbi.nlm.nih.gov/27998009/ .
Tsamantioti ES, Mahdy H. (2021). Endometriosis. [Updated 2021 Feb 25]. In: StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK567777/












