Here's what we'll cover
Here's what we'll cover
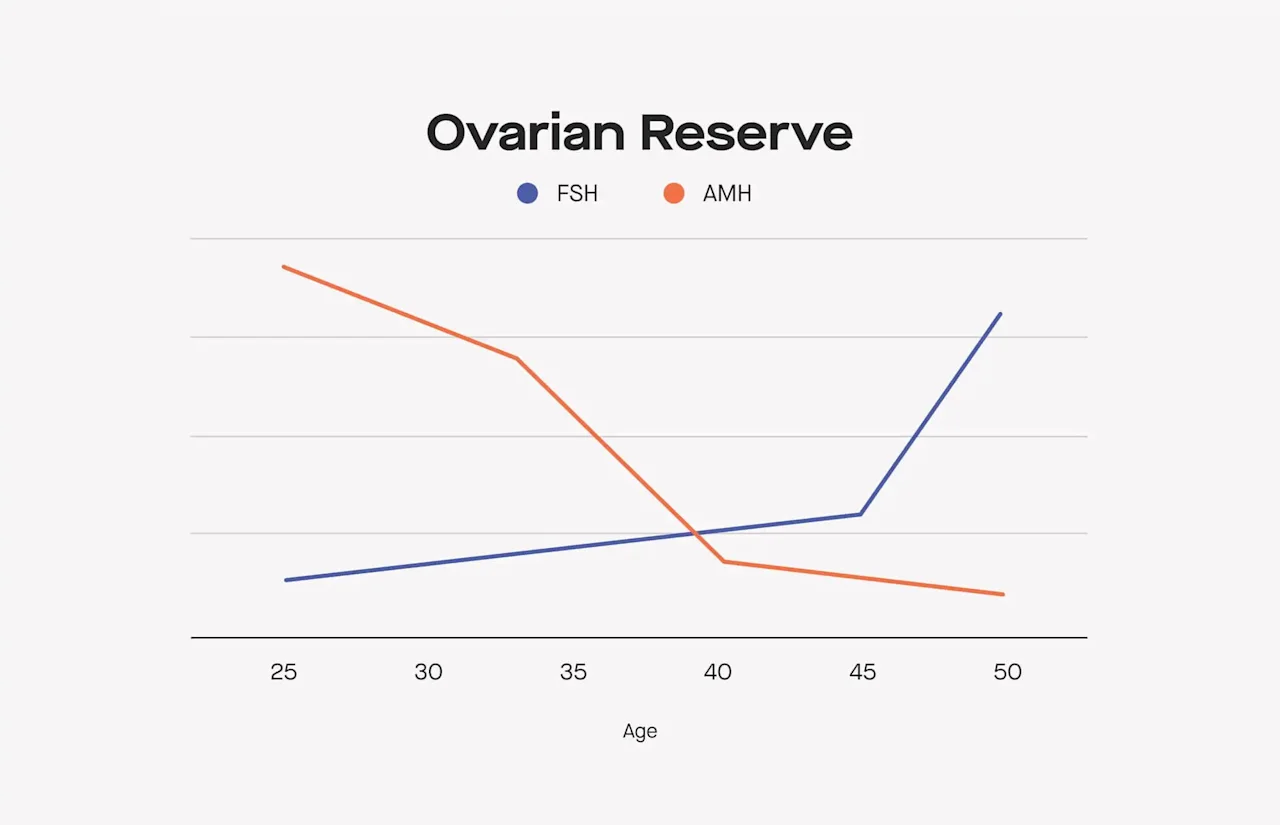
Over the last fifteen years, the science of testing hormones related to ovarian reserve (aka egg count) has made some pretty remarkable strides. Before anti-Mullerian hormone (AMH) was discovered to be a more reliable marker of ovarian reserve, fertility clinics relied primarily on follicle-stimulating hormone (FSH) for testing. So, if doctors place more emphasis on AMH these days, is FSH still worth testing? The answer is yes — FSH can provide important info too.
AMH and FSH *both* provide insight into your egg count, along with the estrogen estradiol (E2). Testing these hormones, FSH included, can help you understand your overall reproductive timeline so you can map out a plan for having kids.
In this post, we’ll explore the nuances of FSH and what it can tell you about fertility. Here are the most important takeaways:
Follicle-stimulating hormone's (FSH) primary responsibility is stimulating growth of the follicles that contain your eggs. In other words, FSH helps set the stage for ovulation to occur.
Your FSH level rises as you approach menopause. This is because as you get older and your egg count dwindles, your body has to work harder to prepare an egg for ovulation.
Your FSH level shouldn’t be interpreted in isolation. FSH is one data point that tells you about your ovarian reserve and should be interpreted with E2, but more weight should be put on your AMH level.
FSH does NOT tell you about your ability to get pregnant today, and it also can’t determine if you’ve reached menopause. But, coupled with AMH and E2, your FSH level can provide insight into your overall reproductive timeline.
High FSH is an indication, not a cause, of reduced egg count. There’s a common misconception that lowering a high FSH level will boost fertility, but there’s no way to increase your egg count as you age.
If you’re not on hormonal birth control (or you're on the (If you are on birth control other than the hormonal IUD or minipill and/or you don’t get a period, you can still take the test and measure your AMH, which is the most important hormone in the panel for understanding ovarian reserve.)
What is FSH and why does it matter?
Hormones are chemical messengers that travel through the body via the bloodstream, and tell organs and cells in your body what to do. Follicle-stimulating hormone (FSH) is produced in the pituitary gland of the brain and acts on the ovaries. Its primary responsibility is stimulating growth of ovarian follicles (which makes “follicle-stimulating hormone” a pretty apt name!) that house and develop your eggs. In other words, FSH helps set the stage for ovulation to occur.
Measuring this particular hormone is like listening in on the messages your brain is sending to your ovaries. From these messages, we can get more insight into how these systems are working — and how their functions are changing over time as we age and fertility declines.
A super important note: No matter what your FSH level is, it *won’t* tell you whether or not you can get pregnant right now. (Even if your egg count is really low, it still only takes one sperm and one egg!) But, coupled with other hormones that give you insight into your ovarian reserve — anti-Mullerian hormone (AMH) and estrogen (E2) — it can help you understand your timeline for having kids.
How can FSH change throughout your lifetime?
Levels of FSH rise as we approach menopause. Why? As we age, our egg count declines. This means that over time, we’ll have fewer follicles developing in our ovaries. When ovarian follicles grow, they give off estrogen (E2). Estrogen tells the brain that it’s okay to shut off production of FSH (in other words, E2 and FSH work in a “negative feedback loop”).
So, as you have fewer follicles, there’s less E2. This means the pituitary never receives the signal that it can stop producing FSH and your levels rise.
Let’s break that feedback loop down a bit more:
When you’re younger, it looks something like this: | As you get older, it looks more like this: |
|---|---|
• Your pituitary tells your ovaries to start growing follicles to prepare for ovulation. The pituitary sends FSH to stimulate the growth of the follicles. • • Your ovaries start growing follicles. • • As these follicles grow, they give off E2. This sends a message to the pituitary that there are plenty of follicles growing, and the pituitary stops producing FSH. | • Your pituitary tells your ovaries to start growing follicles to prepare for ovulation. The pituitary sends FSH to stimulate the growth of the follicles. • • The ovaries start growing follicles — but since your egg count is lower, fewer follicles grow each cycle. • • Since there are fewer follicles growing, they give off less E2. The pituitary doesn’t get the message that there are enough follicles, so it keeps producing FSH. |
So can a high FSH level confirm that you’ve reached menopause? FSH levels of >30 IU/L can indicate that someone is approaching the menopausal transition, but gynecologists rely more on symptoms and menstrual regularity in determining if someone is entering (or has reached) menopause. It’s also worth noting that elevated FSH levels can also point to primary ovarian insufficiency (POI), a rare condition where ovarian function ceases before age 40.
How does FSH change within each menstrual cycle?
Since FSH is a hormone that helps power ovulation, it fluctuates predictably over the course of your menstrual cycle as your body gets ready to ovulate:
At the beginning of your cycle, FSH levels are at their lowest.
As FSH levels rise, the follicles grow and eggs begin maturation in the ovary.
These follicles start to produce estrogen, which is a signal to the pituitary gland that it’s time to shut off production of FSH.
Since your FSH level can vary quite a bit throughout your cycle, fertility clinics test FSH on a particular cycle day (day 3) to capture your FSH level at its baseline.
What do low, "normal," and high FSH levels mean for ovarian reserve?
Before we dig into the specifics, here’s something that’s really important to remember: FSH levels are only one data point around your ovarian reserve and shouldn’t be interpreted in isolation. "FSH should always be considered in the context of E2. A high E2 can mask an otherwise high FSH," says Dr. Sharon Briggs, PhD, Modern Fertility's head of clinical product and research. "If you don't measure E2, you don't know if your FSH is being suppressed by E2. Either way, we put more weight on your AMH level when interpreting ovarian reserve."
Think of it this way: If your hormones were a band, AMH is the lead singer. FSH and E2 are on backup vocals. They’re all important for making the music happen, but AMH takes the spotlight.
What does it mean to have low or "normal" FSH levels?
Modern Fertility's reference range categorizes FSH levels under 3.85 mIU/mL on day 3 of your cycle as "Low," and levels between 3.85 and 8.78 as "Normal." If your FSH level is low (<3.85) or "normal" (3.85-8.78), that’s one indication (read: not a definitive answer) that you have the expected number of eggs and amount of follicles developing every month for your age — the latter of which are producing enough E2 to turn off the body’s production of FSH.
A low FSH, however, shouldn't be interpreted on its own. "If FSH is low and E2 is normal, it's unlikely to be a cause for concern — especially if you are getting regular cycles," explains Dr. Briggs. "But even in the case of irregular cycles, a single low FSH result is not likely to be clinically concerning. Low FSH becomes a problem if E2 is also low and someone is not getting any periods at all."
Low FSH levels can also occur in people who are underweight or have recently had substantial weight loss, or if there’s an issue with your pituitary gland that’s causing it to not produce enough hormones. It’s always a good idea to follow up with your healthcare provider if you have any concerns.
What does it mean to have high FSH?
Modern Fertility's reference range categorizes FSH levels between 8.78 mIU/mL and 15 on day 3 of your cycle as "Slightly High" and those above 15 as "High." If your FSH level is high (>15), that’s an indication (again, not a definitive answer) that you could be working with fewer eggs and have fewer follicles developing each month — meaning your pituitary isn’t getting the signal (in the form of E2) to stop FSH production.
It’s good to keep in mind that doctors distinguish between a temporarily high FSH level and a sustained high FSH level. FSH fluctuates more from cycle to cycle than AMH does — which is another reason to look first to AMH when interpreting your results. Depending on how high your FSH is, your doctor may order a retest to see if your level was temporarily elevated or if the high result persists over time. Since FSH can fluctuate from cycle to cycle, a single high result is less likely to be concerning as it may be in the normal range in a subsequent month.
Here's a quick breakdown of how to think about high FSH levels:
FSH + AMH: A high FSH in isolation is unlikely to be clinically concerning if your AMH level is "normal." If your high FSH level is coupled with a low AMH level, both signals point toward a potentially lower reserve of eggs for your age. It's worth it to discuss this combination of results with your healthcare provider.
FSH + E2: If FSH is high and E2 is very low, this can be a sign of menopause — especially if AMH is also very low.
What does your FSH level have to do with your fertility?
As we mentioned at the top of this article, earlier days of ovarian reserve testing commonly relied on FSH as the primary indicator of ovarian reserve and menopausal timing. About 15 years ago, AMH was discovered to be a more reliable marker of ovarian reserve. According to Dr. Briggs, "AMH has largely replaced day 3 FSH for two reasons: AMH is less variable throughout the cycle and can be measured any day, which is much more convenient for patients and doctors. Secondly, it is believed that AMH levels decrease prior to FSH levels increasing thus providing an earlier signal of ovarian reserve decline."
Can you lower your FSH level?
A common question we hear from customers is, “What can I do to lower my FSH level?” First, it’s important to remember that FSH levels can fluctuate from month to month. So a single high level in isolation is unlikely to be concerning — and may in fact be "normal" in another cycle.
There’s some evidence that acupuncture can decrease FSH, but the quality of the studies showing this effect is questionable. The role of diet and supplements has been researched a little, and there are varying amounts of research about the effectiveness of certain foods (here, here, and here) in lowering FSH.
But even if there was a clinically validated “silver bullet” for lowering your FSH level, doing so would kind of be like treating a symptom rather than the actual cause. In other words, a high FSH level is only a potential reflection of a lower egg count — not what's causing a lower egg count. Since we’re born with all the eggs we’ll ever have, there isn’t a way to increase egg count as we age.
If your FSH level is high and, when interpreted alongside your AMH and E2 results, points to low ovarian reserve, that’s important info to take to your doctor so you can discuss your options.
How can you measure your FSH level?
If you’re interested in getting a read on your FSH level, a great way to do that is by getting a blood test panel. FSH is included in the blood test panel for people who are not on hormonal birth control (or who are on the hormonal IUD or minipill) and get a regular period.
In this article, we talked a lot about how important it is to interpret your FSH alongside your AMH and E2 results. When you get your results back, you’ll get dedicated hormone reports that explain the roles of each of these hormones and your levels:
An FSH and E2 report that specifically addresses how to think about these two hormones in combination.
An Ovarian Reserve report that interprets your AMH, FSH, and E2 levels together so you can get the fullest picture of what your results indicate about the amount of eggs you have.
An Egg Freezing and IVF report that helps you understand what your levels indicate about success in these procedures.
A Menopause report that explains the clues that FSH and AMH provide for your overall reproductive timeline.
Since FSH can vary quite a bit throughout your menstrual cycle, testing on day 3 of your period is important for your results to be interpreted correctly.
The bottom line
Testing FSH, alongside AMH and E2, is a great way to get multiple data points that help you think through your timeline for having kids (and the flip side of this, how soon you’re likely to go through menopause) and potential success in IVF and egg freezing.
It’s true that AMH is a more reliable marker of ovarian reserve than FSH alone, so it’s important to look at your FSH result in context.
This article was reviewed by Dr. Sharon Briggs, PhD, Modern Fertility's head of clinical product and research.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.










