Here's what we'll cover
Here's what we'll cover
Unless you’re actively trying for kids, you might only think about your menstrual cycle when your period comes around. In some ways, that makes a lot of sense: Periods are the easiest part of the cycle to spot (see what we did there?) without any further investigation. Even the way we refer to the menstrual cycle puts periods front and center — menstruation is literally in the name. But there’s so much more going on that’s worth paying attention to, even if it’s not quite as obvious — especially the symptoms and experiences we may have during different phases of our menstrual cycles.
Understanding menstrual cycle phases and knowing where you are in your cycle can be helpful whether or not conception is on your mind. Here’s some of what tracking your cycle allows you to do:
Get a heads-up when your period’s coming (which makes it easier to plan ahead or stock up on products).
If you are trying to get pregnant, it can clue you in to the days when sex or insemination gives you the best chances.
It can give you important details to bring to your healthcare provider when managing your reproductive health and conditions like polycystic ovary syndrome (PCOS).
To that end, welcome to the Modern guide to the menstrual cycle. Below, you’ll find all the info you need to know what’s going on with your body during various menstrual cycle phases, from beginning to end — and additional context for when you might see changes.
Here's what we'll cover
Menstrual cycle phases, from beginning to end
First, let’s outline the order of the three menstrual cycle phases since you’ll be reading these terms a lot. Based on the "textbook" 28-day cycle:
Follicular phase: This phase lasts from day 1 of your period until approximately day 14 of your cycle (or until you ovulate).
Ovulation: This usually happens around day 14 and only for one day.
Luteal phase: This phase begins after ovulation and lasts for about 14 days.
The main purpose of these menstrual cycle phases is to get all your ducks in a row for a possible pregnancy — the “ducks” in this instance being the ovaries and uterus. The cycle kicks off with a menstrual period, and when the last phase ends, the first one begins again, and so on, and so on. That is, until menopause (when cycles come to a complete stop).
Do we all have the same cycle?
While many of us were taught in school that the “average” menstrual cycle length (from one period to the next) is 28 days, the American College of Obstetricians and Gynecologists (ACOG) and the US Office of Women’s Health say that it can last anywhere from 24-38 days. But there can actually be an even wider range:
One 98,000-person study found that 95% of their participants have cycles between 20 and 40.4 days in length.
However long your cycle is, one thing remains constant: Hormones (little chemical messengers) produced by the brain and reproductive system set off a chain of events that preps the body for pregnancy if an egg is fertilized by sperm.
Plus, a little trivia: Only a handful of mammals have cycles with menstruation (aka periods). Beyond primates, at least four bat species show signs of menstruation, and there is plenty of evidence proving the elephant shrew also menstruates. Now you know!
Now, keep reading as we walk you through each of the menstrual cycle phases.
1. The follicular phase: Period + prep
The follicular phase, aka the proliferative phase, begins on the first day of your period (more on this in the luteal phase section) and ends around day 14, based on the “textbook” 28-day cycle. One study found that the average number of days in the follicular phase is 15.8.
What’s happening in the body during the follicular phase:
The pituitary gland in the brain sends two hormones — follicle-stimulating hormone (FSH) and luteinizing hormone (LH) — through the bloodstream to the ovaries.
FSH and LH trigger about 15-20 eggs to mature. Each egg lives in its own tiny fluid-filled sac, called an ovarian follicle.
The ovaries start producing estrogen, which goes back up to the brain and stops FSH production in its tracks.
In ovulatory cycles, aka ones where ovulation occurs, one ovarian follicle steals the show and keeps maturing (and producing estrogen) — the immature follicles that aren’t developed enough for ovulation fade into the background and die off.
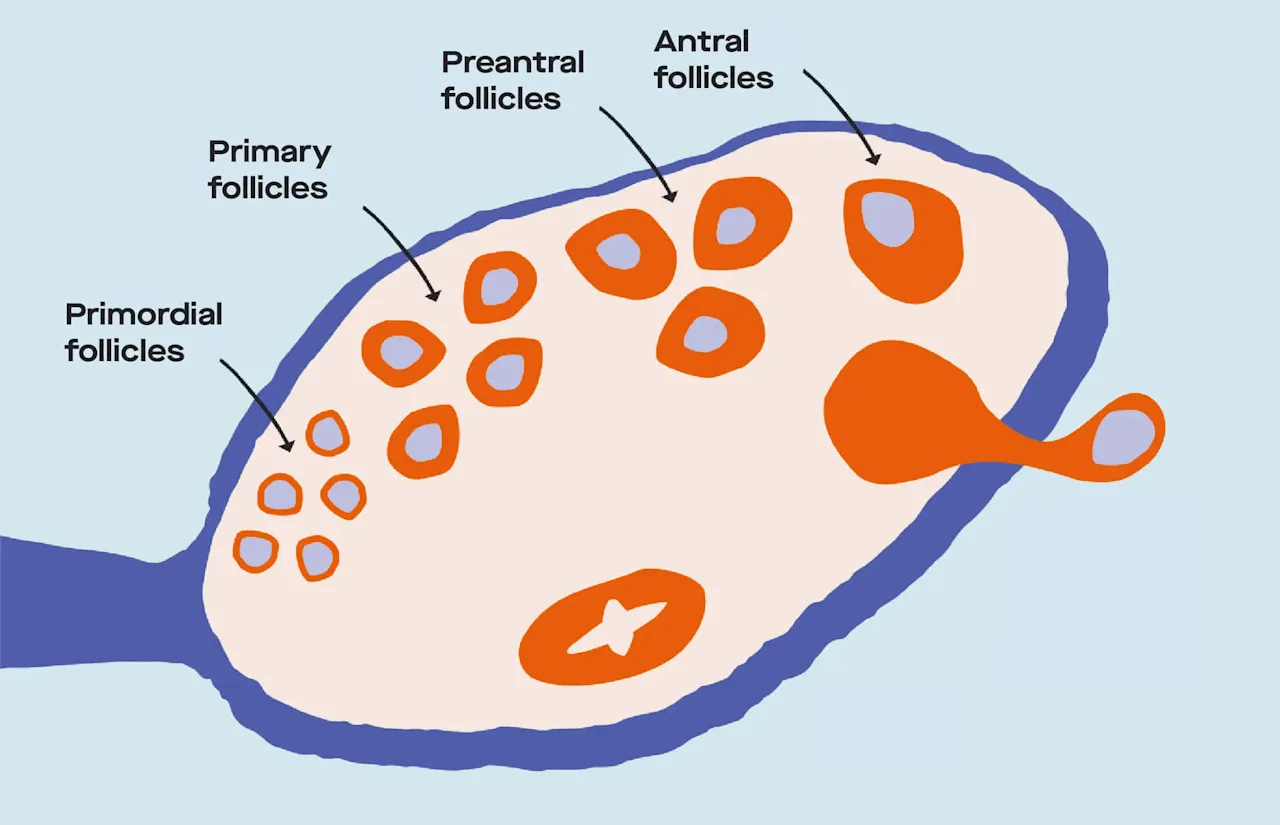
The stages of maturation (aka development) of the ovarian follicles in the ovary.
Meanwhile, the lining of the uterus (in medical-speak: the endometrium) is also keeping busy — this is what “proliferative” refers to (proliferation = rapidly producing cells or tissue). As levels of estrogen increase, the uterine lining thickens in preparation for implantation. At this time, cervical mucus, or the fluid produced by the cervix, picks up production and it becomes more cloudy and sticky.
Possible symptoms and experiences during this phase include:
Cramps, bloating, headaches, tender breasts, body aches, fatigue, mood swings, and skin breakouts during your period.
Increased sexual desire due to higher estrogen levels.
High estrogen during this phase was linked to feeling more in the mood, according to one 2013 study. (Essentially, your body is revving up the hormone engine to make fertilization more possible.)
How to manage symptoms:
You can treat painful cramps, headaches, and other body aches with over-the-counter medications like ibuprofen, as well as heating pads and exercise.
Meditation and good sleep hygiene can help you manage mood swings and irritability.
Hormonal birth control can help regulate symptoms like menstrual migraines , acne, cramps, heavy bleeding, and a severe form of PMS called premenstrual dysphoric disorder (PMDD).
2. Ovulation: The egg goes on its journey
About 14 days into the cycle (based on a 28-day cycle), we enter a new, one-day phase where the ovary releases an egg for possible fertilization: ovulation.
This is a time of *peak* fertility. The five days leading up to and the day of ovulation are considered your “fertile window,” meaning the days when your chances for conception are highest.
Why are the days before ovulation part of that window? The egg only has 12-24 hours for fertilization, but sperm can last up to five days (!) in the reproductive tract… so sex or insemination during that 6-day window can mean sperm is there waiting when the egg is released.
Tracking your ovulation to plan sex or insemination around your fertile window increases the likelihood that sperm and egg will meet up at *just* the right time for fertilization to be possible.
During ovulation, your cervical mucus is also at its fertile peak — it’s slippery, clear, and stretchy, and has a similar consistency to a raw egg white.
If sperm tries to meet up with the egg at this time, the mucus will help move sperm past the cervix and make conception more likely.
What’s happening in the ovaries during ovulation:
24-48 hours before ovulation, the rise in estrogen produced by the dominant follicle signals that it’s time to ramp up luteinizing hormone (LH) production in the brain.
The dominant follicle ruptures and releases a mature egg. (Ovulation!)
The little finger-like tendrils at the end of the fallopian tube (called fimbriae) grab the egg and send it on its way through the tube (a journey that lasts about 30 hours).
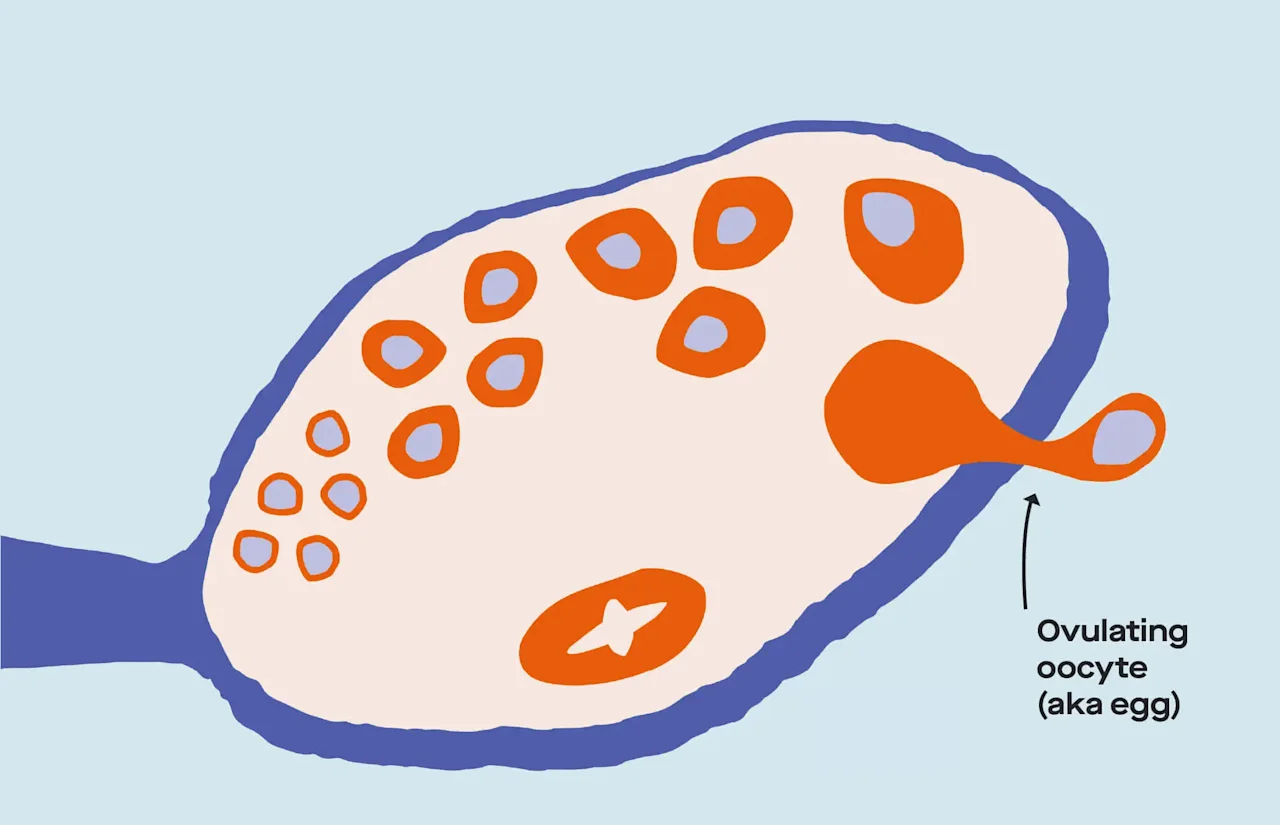
Ovulation! The dominant follicle ruptures and releases the most mature egg.
Possible symptoms and experiences during this phase include:
Ovulation pain, which is known as mittelschmerz — German for “middle pain” (because it happens around the middle of the cycle).
Each ovulatory cycle, the ovaries alternate which one releases an egg. About 1 in 5 people with ovaries experience abdominal pain on the side with the ovary that’s ovulating — this is known as mittelschmerz, which is German for “middle pain” (because it happens around the middle of the cycle).
There are two possible causes for this pain: The follicle growth might stretch the ovary’s surface and cause pain, or the ruptured follicle might irritate the abdominal stomach lining.
Breast tenderness
How to manage symptoms:
Mittelschmerz can be treated with over-the-counter pain relievers or hormonal birth control to stop ovulation altogether.
3. The luteal phase: It's go time
The last phase of the cycle is called the luteal phase (sometimes secretory). The word “luteal” refers to the development of the corpus luteum (Latin for “yellow body”) — a structure that forms in the ovary after ovulation to prep the body for pregnancy, regardless of whether or not fertilization occurs. According to one large study, the average length of this phase is around 13.7 days.
What’s happening in the body during the luteal phase:
The ruptured follicle transforms into the corpus luteum, which produces high amounts of both estrogen and progesterone to thicken the uterine lining and make it a receptive and nourishing home for a fertilized egg.
If sperm fertilizes the released egg in the fallopian tube, the fertilized egg heads toward the uterus and implants into its wall to support embryo development. (This takes place around 8-10 days after fertilization.)
In the event of pregnancy, the corpus luteum keeps on producing progesterone for 10 weeks and the implanted embryo begins producing human chorionic gonadotropin (hCG). (hCG is what pregnancy tests, like ours, use to detect early pregnancy.)If the egg isn’t fertilized after about 24 hours, the uterus sheds the egg and its excess lining in the form of your period (bleeding that lasts ~2-7 days), and the corpus luteum decays.
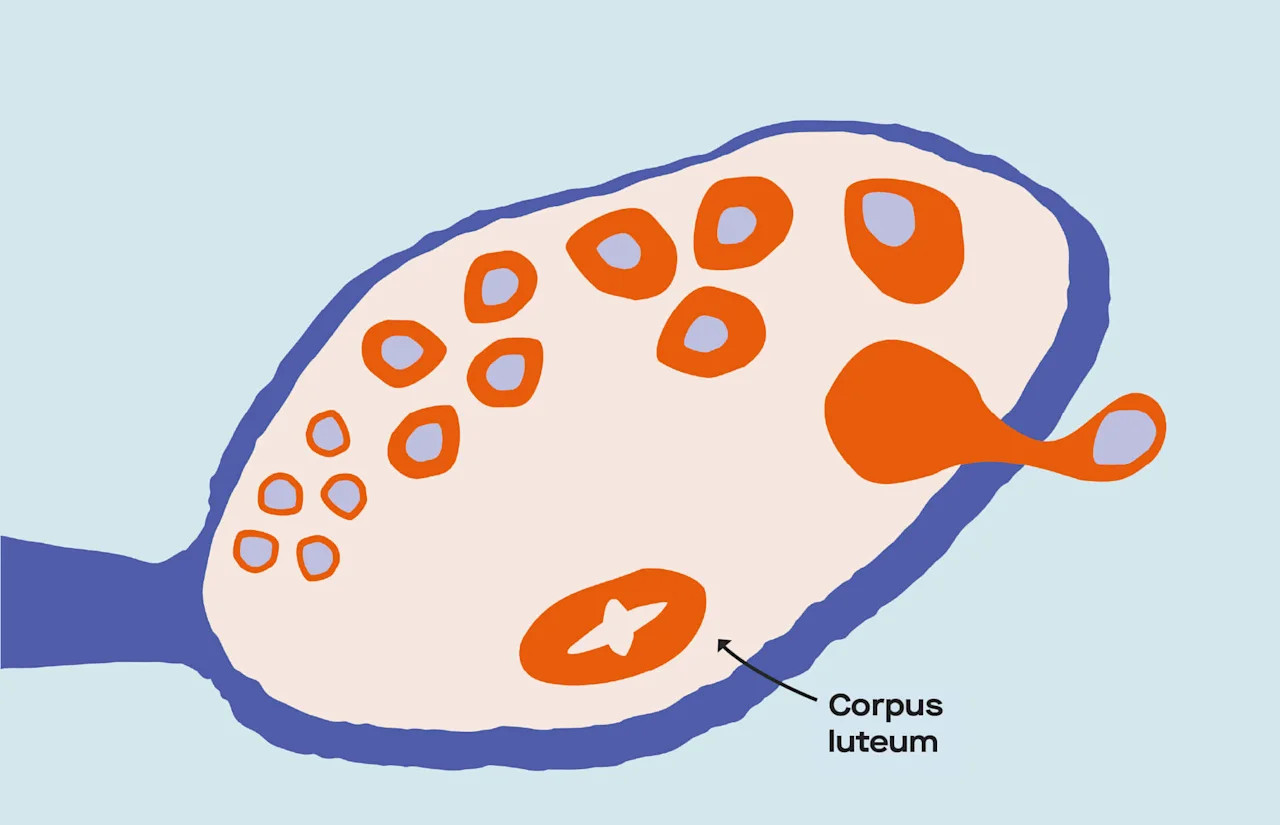
After ovulation, the ruptured follicle turns into the corpus luteum. (Since the menstrual cycle repeats, the different follicles will be in various stages in the ovary.)
Possible symptoms and experiences during this phase include:
Premenstrual syndrome, or PMS. In fact, most people with ovaries (90%) experience some premenstrual symptoms, like bloating, cramping, or mood changes, while others experience a broader range of symptoms — both physical and emotional.
PMS typically begins after ovulation and before the period starts.
The medical community isn’t sure exactly why some people experience PMS symptoms, but it’s likely a combo of factors — ovarian hormones being one of them. We know this in part because symptoms often improve if ovulation is suppressed by hormonal birth control.
PMS can be associated with physical symptoms (like swollen or tender breasts, stomach issues, aches) and emotional symptoms (like tiredness, sleep problems, anxiety, mood swings, lower sex drive).
Premenstrual Dysphoric Disorder, or PMDD. This is a more severe form of PMS that occurs in up to 2% of people with ovaries.
PMDD has similar physical side effects as PMS, but the emotional side effects can be debilitating.
You may feel sadness or hopelessness, anxiety or tension, extreme moodiness, and irritability or anger.
Just like PMS, the cause of PMDD isn't clear to the medical community. Since pre-existing depression and anxiety are common for people who experience PMDD and PMS, the theory is that hormonal changes may cause mood disorders to become even worse.
How to manage symptoms:
Regular exercise, balanced eating, eight hours of sleep a night, stress management, and not smoking can all help with PMS symptoms.
Over-the-counter pain relievers can also provide relief.
Prescription meds like hormonal birth control may relieve physical symptoms, while antidepressants (SSRIs) and anti-anxiety medications may relieve emotional symptoms, especially with PMDD.
The factors that impact the menstrual cycle
Okay! You’re all caught up on the menstrual cycle phases. But, since our bodies are all different, what factors influence the ebbs and flows of our unique cycles?
Like we mentioned at the top of this article, the exact length of the menstrual cycle varies from individual to individual. For most people with ovaries, the luteal phase lasts 14 days — but there’s typically more variety in the follicular phase leading up to ovulation, which often ranges from 10 to 16 days.
What’s way more important than how long or short your cycle is consistency from cycle to cycle. If your cycles are irregular, you may ovulate or get your period at different times than expected — or you may not ovulate or get your period at all some months.
Some irregularities are a natural part of aging, and some may be the result of taking hormonal birth control or having certain health conditions. (Read this article for more info on irregular cycles.)
Below, we’ll talk about some of the factors that influence your cycle the most.
Age and the cycle
Your reproductive window, or the years in which you’re able to conceive, starts at menarche (the first period) and ends at menopause (when the menstrual cycle comes to a complete stop).
In the US, the average age of menarche is 12.4, while the average age of menopause is 51.
Starting your period at a younger age may mean menopause comes at a younger age — and genetics play a role in timing of menarche, perimenopause (when the cycle begins to change leading up to menopause), and menopause.
When you first start getting periods, cycles are typically more irregular, but they become more regular as you get older.
Once you’re in perimenopause, typically in your mid-40s (but anytime from your late 30s on is fair game), cycles may become irregular again as you get closer to the onset of menopause. (That’s because the ovaries are slowing down production of estrogen and progesterone until they stop producing eggs altogether.)
Lifestyle factors and the cycle
Irregularity in your unique menstrual cycle can be caused by several different lifestyle factors:
Smoking: In one 1999 study, heavy smoking was linked to 4x the risk of shorter cycles, mostly because of an abbreviated follicular phase — and possible increased risk of anovulation (when ovulation doesn’t happen) and a shorter luteal phase.
Exercise level: Intense exercise or rigorous athletic training can interrupt the menstrual cycle as a result of low body fat, high stress, and high energy expenditure. (But it’s not just extreme athletes whose cycles are impacted by exercise.)
Stress: High stress levels can cause ovulation and menstruation to stop because of their effect on the hypothalamus — the part of your brain that regulates the hormones in charge of the menstrual cycle.
Weight: Low or high body weight, as well as rapid weight loss, can lead to absent periods.
Pregnancy or breastfeeding: A missed period is an early sign of pregnancy. Breastfeeding can also delay the return of your period after pregnancy.
Health conditions and the cycle
Certain health conditions can also result in disruptions or changes in the menstrual cycle:
Uterine fibroids: Non-cancerous growths on the inside or outside of the uterus or uterine wall. These can cause painful periods and/or heavy menstrual bleeding or periods that last longer than a week.
Endometriosis: A disorder where tissue similar to uterine lining grows outside of the uterus. This can cause pain before and during periods, and less frequently, heavier or irregular menstrual bleeding.
"Out-of-range" hormonal levels(like hyperprolactinemia, PCOS, and thyroid conditions): Too high or too low levels of prolactin, the hormone that stimulates milk production (hyperprolactinemia); testosterone, a sex hormone (polycystic ovary syndrome, or PCOS); and thyroid hormones (hypo- and hyperthyroidism) can impact everything from period flow to whether or not ovulation happens.
Primary ovarian insufficiency (POI) and menopause: Your period can become more irregular as you approach menopause, which, clinically speaking, means periods have stopped for 12 months or longer. The average age for menopause is 51, but for those with POI, it happens before age 40.
Pelvic inflammatory disease (PID): A bacterial infection often caused by untreated sexually transmitted infections (STIs) that spreads to the uterus and reproductive tract. PID can lead to irregular periods, vaginal discharge with an unpleasant smell, pain in the lower abdomen, and even infertility.
Birth control and the menstrual cycle
Reversible (i.e., nonsurgical) birth control methods were designed to place obstacles throughout the menstrual cycle, making conception nearly impossible.
Hormonal birth control: Synthetic progestins and estrogen typically block conception with two or more of the following moves: suppressing ovulation, thickening cervical mucus, and thinning uterine lining. (Take a deep dive into how hormonal BC impacts ovulation and the menstrual cycle.)
Copper IUD: This BC is non-hormonal and works by using copper ions to create a toxic environment for sperm, which then prevents egg implantation and pregnancy.
How does birth control affect menstrual bleeding?
Withdrawal bleeding: Many contraceptives aim to mimic the untouched menstrual cycle, so they include time off from the hormones to cause what’s known as “withdrawal bleeding” when a period would typically occur. The body reacts to the withdrawal of hormones by shedding the uterine lining. But this bleeding isn’t a “true” period because ovulation hasn’t occurred — and because the uterine lining is thinner with most types of birth control, the bleeding is often lighter than a usual period.
Skipping periods: You can stop periods entirely by skipping the placebo birth control pills if you’re taking oral contraceptives or skipping the 7-day break when using the vaginal ring. The most common side effect of menstrual suppression is breakthrough bleeding (unexpected bleeding), but that typically lessens over time.
How can you track your cycle?
Staying on top of where you are in menstrual cycle phases helps you figure out what’s coming next — making it easier to prepare for your period, time sex or insemination if you’re trying to conceive, or understand how health conditions or lifestyle factors might be impacting your reproductive health. So, how can you stay on top of your cycle? Keep reading:
Tracking apps: Typically, apps count the number of days between the last day you reported being on your period and the first day you report being on your next. Using that info, they can make a prediction of how long your cycle is and when your next period will come. Apps that track your LH levels take the predictions to the next level by grounding them in your *actual* hormone levels.
Ovulation tests: Ovulation tests use biological indicators of ovulation, usually LH levels, to help you figure out where you are in your cycle. Most ovulation tests give you a negative/positive result based on LH averages.
Cervical mucus tracking: Since your cervical mucus changes throughout your cycle, you can find clues for where you are in your cycle right in your underwear. At the beginning of your cycle, your menstrual blood will likely cover up the presence of any cervical mucus. As estrogen peaks right before ovulation, the mucus will be cloudier and stickier. Once you’re ovulating, mucus will be slipper, clear, and stretchy, and will resemble a raw egg white. After ovulation, once progesterone levels peak, you’ll stop seeing cervical mucus.
Basal body temperature method (BBT): Many people with ovaries track their basal body temperature, or BBT (the body’s temperature at rest), to look for signs of ovulation — though the changes are most clear after ovulation has already happened. ACOG) explains that “the body’s normal temperature increases slightly during ovulation (0.5–1°F) and remains high until the end of the menstrual cycle,” and your fertile window is “the 2–3 days before this increase in temperature.”
When should you talk to a doctor about your cycle?
Some variation in cycle length is totally normal — in fact, only about 20% of people will have cycles that are identical in length from one month to the next. But if you notice any of the following changes in your cycle, it's important to reach out to your healthcare provider to see what the underlying cause may be:
You experience sudden changes to how often you get your period
You bleed between periods (this is commonly referred to as spotting or intermenstrual bleeding)
Your period is heavier than average (i.e., you soak through your menstrual product every two hours or less throughout your cycle)
You bleed for more than a week
Your periods are extremely painful
You've gone 90 days, or the equivalent of three menstrual cycles, without getting a period (this is a condition known as amenorrhea)
Your doctor can help you take steps toward figuring out what’s causing your irregular periods and determine the appropriate treatment.
Closing the loop: The TL;DR
Throughout menstrual cycle phases, there are many hormone-led changes in the reproductive system that make conception and pregnancy possible. The cycle begins with your period and ends with your next one, before repeating the cycle all over again.
The first phase, called the follicular or proliferative phase (which is also when your period happens), focuses on maturing the ovarian follicles, getting the uterine lining ready, and making cervical mucus easier for sperm to swim through.
Ovulation comes next: This is when the dominant follicle releases an egg through the fallopian tube to meet up with sperm.
Finally, the luteal phase (or secretory phase) wraps things up by prepping the uterine lining for embryo implantation — or triggering your period if the egg isn’t fertilized.
Learning how your menstrual cycle works is vital for having a better understanding of your body, and we’re here to empower you with knowledge at each step (or phase!) of the journey.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.










