Here's what we'll cover
Here's what we'll cover
Subcutaneous injections, which are injections administered just under the skin, can be used to deliver a wide range of medications. They offer the added benefit of being a straightforward way for people who need frequent injections to get their medicine at home without visiting a healthcare provider.
These injections are common in people who have diabetes requiring insulin administration. Many fertility drugs and certain treatments for arthritis, multiple sclerosis, and cancer can also be administered subcutaneously (Woodley, 2022).
No matter how common this medication delivery method may be, injecting yourself (or someone else) may be intimidating. But with guidance from a healthcare professional, you can learn to give medications subcutaneously on your own.
Here’s a look at how subcutaneous injections work and what to expect.
What is a subcutaneous injection?
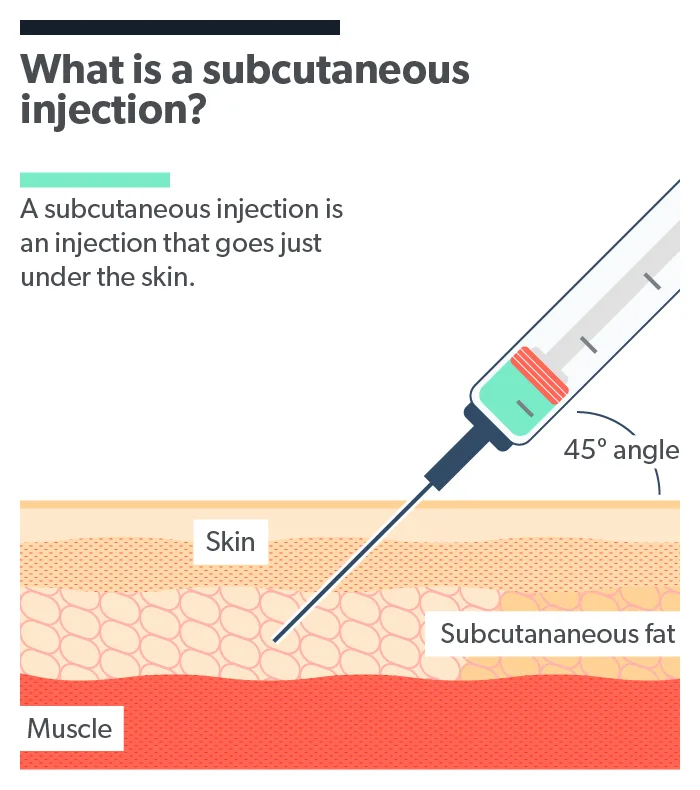
Subcutaneous means under the skin. A subcutaneous injection—also called a sub-Q or SQ injection—goes just under the skin and into that layer of fat above the muscle. These injections are typically less painful than intramuscular injections, which go into the muscle (requiring longer needles) (Usach, 2019).
In addition to being relatively painless, SQ injections are easy to do at home, and the small needle size means the risk of infections is low (Usach, 2019).
Compared to intramuscular or intravenous (into a vein) injections, subcutaneous injections deliver medications more slowly, which is important for certain medications. For instance, in the case of an insulin injection for diabetes, slower medication delivery means a more effective and even control of blood sugar.
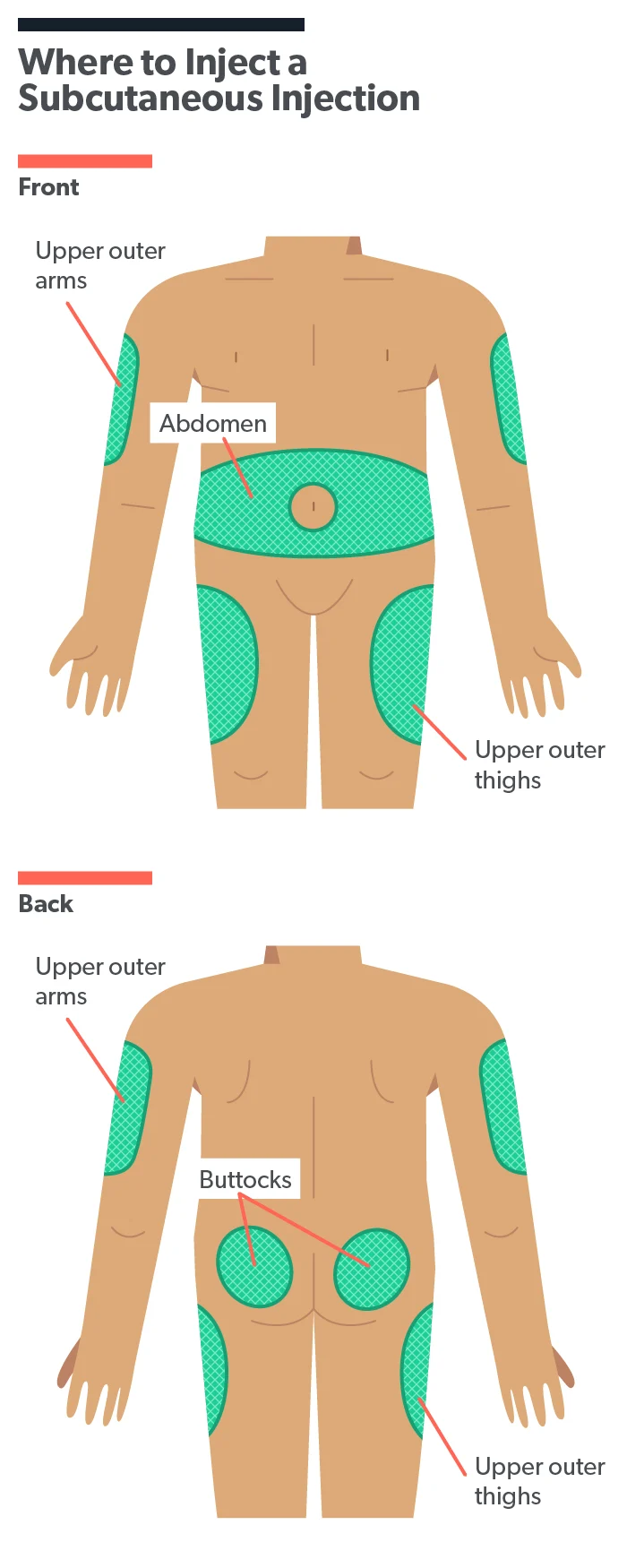
Subcutaneous injection sites
There are several common subcutaneous injection sites, all of which are places on the body with a layer of fatty tissue under the skin. These include the outer surface of the upper arm, the upper area of the front of the thigh, the abdomen (two inches from the belly button), and the buttocks (MedlinePlus, 2021). Where you inject your medication will depend on your healthcare provider’s instructions.
If you are giving yourself or another person daily or weekly injections, your healthcare provider may recommend switching up your injection site each time or positioning the needle at least one inch away from the last place you injected. Repeatedly using the same spot can cause a sort of scar-like tissue to form, which may make it more difficult for your body to absorb the medication injected there. It can also cause bruising (Kim, 2021).
What to know before the injection
Your healthcare provider will go over the specifics for your particular medication, including how to store the medication (in the refrigerator or at room temperature), the dosage, when to inject, and details about the injection device you’ll be using.
Likewise, if you’re helping someone else with their injections, follow their healthcare provider’s exact instructions. Some medications have very specific dosing requirements based on weight and other factors unique to each person.
There are different types of injection devices, so it’s important to know ahead of time what type you’ll be injecting. Some come prefilled with an exact dose for one-time use. Others contain multiple doses or need to be refilled. There are also pen-like injection devices that deliver medication with the click of a button (FDA, 2013).
Yet another type of injection device is called an autoinjector, best known with EpiPens, a quick-jab method of delivering epinephrine into the muscle for people having a severe allergic reaction (Campbell, 2016). Autoinjectors come in a variety of styles and are also used for subcutaneous injections of other medications (Tornero-Molina, 2021).
Many medications come in vials or containers that need to be transferred to a syringe. These typically use disposable needles and syringes.
Taking stock of supplies
Before any injection, it helps to have your supplies laid out on a clean, dry surface. Supplies typically include:
Medication and sterile disposable needles/syringes (or a prefilled injection device combining both)
Alcohol pad or cotton ball with rubbing alcohol (isopropyl or ethanol alcohol)
A puncture-proof container for safe needle disposal (as needed)
A band-aid
How to give a subcutaneous injection
The steps taken to give yourself or another person a subcutaneous injection are based on the device you are using. Always follow the instructions from your healthcare provider.
Here are some standard approaches:
Wash your hands thoroughly with soap and water.
Cleanse the injection site with a fresh alcohol wipe or cotton ball soaked in alcohol; wait 30 seconds for the site to dry before injecting.
Injection using a pen injector or autoinjector
If using a pen injector or another prefilled injection device, follow your provider’s instructions. Here’s some more information to help guide you (FDA, 2013):
If the device is prefilled with the exact dosage, your healthcare provider will instruct you to hold the pen to the skin’s surface and push the button on the top. For autoinjectors, the force of the injector hitting the skin activates the needle.
Multi-use injectors have a dosing dial to ensure the correct dose is given. It’s important to discuss dosing and how to set the dial with your healthcare provider.
Some pen injectors have snap-on disposable needles; others have built-in retractable needles.
After the injection, see directions about disposal or storage. Disposable needles will need to be put into a puncture-proof metal or hard plastic container, often called a “sharps container.”
Injection using a disposable needle/syringe
As with prefilled injection devices, consult with your healthcare provider about medication dosing and delivery.
The following are some basics instructions for using a needle and syringe (MedlinePlus, 2021; WHO, 2010):
Remove the needle cap.
Draw up the amount of medication needed (refer to instructions) using the syringe's plunger; this may mean turning the vial upside down.
Tap syringe to clear air bubbles. You may need to push the syringe plunger slightly to clear air from the syringe (air displaces the medication, potentially reducing dosage).
Pinch a 2-inch fold of skin, avoiding the muscle below (fat and skin only).
Hold the syringe with the index finger like a pencil or dart.
Insert the needle with the opening of the needle (called the bevel) facing up at a 45- to 90-degree angle to the pinched skin. A45-degree is usually better in areas where there isn’t much fat, but always follow your healthcare provider’s instructions).
Insert the needle so that it’s completely covered by skin.
Once it’s inserted, slowly push the plunger to inject the medication.
Do not rub or massage the area.
If there is bleeding, apply a bandage.
Place the used needle in a sharps container.
Tips and precautions
The very thin needles used nowadays have made subcutaneous injections less painful. Here are some other ways to reduce discomfort, if needed (Usach, 2019):
Ask your healthcare provider if you can apply a topical anesthetic, like benzocaine, before injection.
Make sure the needle is beveled side up, meaning you can see the oval-shaped hole if the injection is at an angle because it will help the needle slide in more easily.
If using a syringe, push the plunger down slowly rather than quickly. The slower entry of medication doesn’t fracture tissue as much and may lessen bruising (Kim, 2017).
It’s normal to have some pain or bruising for a day or two where you injected the medication, depending on the medication. Your healthcare provider can help you understand what to expect from your medication.
The chances of injecting the medication into a blood vessel in subcutaneous fat are low but possible (Sepah, 2017). If this happens, you may notice blood in the syringe. This is generally not a cause for concern, but it can change how quickly medication takes effect in some cases. Call your healthcare provider if you have any questions or have unexpected medication side effects.
Getting an infection from a subcutaneous injection is rare, but be sure to contact your healthcare provider if you experience fever, redness, warmth, or pain at the injection site in the days following an injection. These could be signs of an infection (Zhu, 2019).
Talk with your healthcare provider
Every medication comes with instructions that are often tailored to the individual. It’s important to consult with your healthcare provider about all medications, dosing, and how to give a subcutaneous self-injection if that’s required for treatment.
Your healthcare provider may have you inject your first doses in their office so you can get comfortable with it. That gives you a chance to get feedback and tips. It takes some getting used to but giving yourself or someone else a subcutaneous injection gets easier with practice.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Campbell, R., Bellolio, F., Motosue, M., et al. (2016). Autoinjectors preferred for intramuscular epinephrine in anaphylaxis and allergic reactions. Western Journal of Emergency Medicine , 17 (6), 775–782. doi:10.5811/westjem.2016.8.30505. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5102607/
FDA. (2013), Guidance for industry and FDA staff . (n.d.). Retrieved on Feb. 10, 2022 from https://www.fda.gov/media/76403/download
Kim, H., Park, H., & Lee, S. J. (2017). Effective method for drug injection into subcutaneous tissue. Nature News . Retrieved on Feb. 10, 2022 from https://www.nature.com/articles/s41598-017-10110-w
Kim, J. (2021). Medication routes of administration. StatPearls . Retrieved on Feb. 10, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK568677/
MedlinePlus. (2019). Subcutaneous (SQ) injections. U.S. National Library of Medicine . Retrieved on Feb. 10, 2022 from https://medlineplus.gov/ency/patientinstructions/000430.htm
Sepah, Y., Samad, L., Altaf, A., et al. (2017). Aspiration in injections: Should we continue or abandon the practice? F1000Research , 3 , 157. doi:10.12688/f1000research.1113.3. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5333604/
Tornero Molina, J., López Robledillo, J. C., & Casamira Ruiz, N. (2021). Potential benefits of the self-administration of subcutaneous methotrexate with autoinjector devices for patients: A Review. Drug, Healthcare and Patient Safety , 13 : 81–94. doi:10.2147/dhps.s290771. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8018568/
Usach, I., Martinez, R., Festini, T., & Peris, J. E. (2019). Subcutaneous injection of drugs: Literature review of factors influencing pain sensation at the injection site. Advances in Therapy , 36 (11), 2986–2996. doi:10.1007/s12325-019-01101-6. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6822791/
WHO. (2010). Best practices for injection. WHO Best Practices for Injections and Related Procedures Toolkit . Retrieved on Feb. 10, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK138495/
Woodley, W. D., Morel, D. R., Sutter, D. E., et al. (2021). Clinical evaluation of large volume subcutaneous injection tissue effects, pain, and acceptability in healthy adults. Clinical and Translational Science , 15 (1), 92–104. doi:10.1111/cts.13109. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8742644/
Yoshida, Y., Sumikawa, M., Sugimori, H., & Yano, R. (2021). Factors that affect symptoms of injection site infection among Japanese patients who self-inject insulin for diabetes. Healthcare , 9 (4), 402. doi:10.3390/healthcare9040402. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066722/
Zhu, Z. K., Weng, T. T., Wang, X. G., et al. (2019). [one case of severe subcutaneous soft tissue infection caused by nonstandard insulin injection]. Zhonghua shao shang za zhi = Zhonghua shaoshang zazhi = Chinese Journal of Burns , 35 (8), 619–621. doi:10.3760/cma.j.issn.1009-2587.2019.08.014. Retrieved on Feb. 10, 2022 from https://pubmed.ncbi.nlm.nih.gov/31474046/










