Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
When you think of an ingrown hair, you probably think of one that’s trapped and growing under the skin. This can happen with eyelashes but it’s rare. Instead, the term ingrown eyelash describes a lash that grows up and out through the skin in the wrong direction: towards the eye.
Ingrown eyelashes are more than a cosmetic issue. A misdirected lash can scratch your eye, and if it continues to touch your eyeball, it can lead to infection, scarring, and even vision loss (Patel, 2021).
Here’s a look at what causes an ingrown eyelash––and how to treat it.
What is an ingrown eyelash?
Ingrown eyelash, also called trichiasis, is a condition that affects (you guessed it) the eyelashes. Trichiasis occurs when you have at least one eyelash growing towards the eye instead of curving away from it.
When the angle of eyelash growth changes, it’s called primary trichiasis. If the entire eyelid turns inward forcing lashes into the eye, it’s called secondary trichiasis. When fewer than five eyelashes are affected it’s considered minor trichiasis. The condition can become serious if there are more than five lashes growing in this fashion (Patel, 2021).
What causes an ingrown eyelash?
Anyone can get ingrown eyelashes. It usually happens when the edge or eyelid margin changes in a way that alters hair growth.
A common cause of ingrown eyelashes is blepharitis—inflammation of the eyelid. Blepharitis can be caused by bacteria on the face, skin conditions (like dandruff or rosacea), blocked oil glands, allergies, and less frequently, eyelash mites (Eberhardt, 2021).
Another culprit are styes, which are red, painful bumps on the eyelid caused by infection. Any type of eyelid inflammation can change the skin around your eyes, potentially altering the way eyelashes grow (Bragg, 2021)
Other factors that can boost the risk of an ingrown eyelash include (Patel, 2021):
Eye infections (like shingles or trachoma)
Trauma or injury to the eyelid
Eyelid surgery
Autoimmune diseases that affect skin around the eyes
Aging (loose skin on the eyelids can change lash direction)
Skin conditions like eczema and psoriasis
Distichiasis, which is when you have two rows of lashes that can move others out of position
Ingrown eyelash symptoms
Sometimes ingrown eyelashes have no symptoms and go unnoticed. However, the majority of cases are noticeable and can be very painful. Common symptoms of ingrown eyelash are (Karademir, 2021):
Eye irritation or feeling like something is in your eye
Eye pain
Watery eyes
Redness and inflammation
Sensitivity to light
Blurry vision (if not treated early)
Ingrown eyelashes are more common on the lower lid than the upper one (Patel, 2021).
Treatments for ingrown eyelashes
Any time you feel pain in the eye, there could be what’s called a corneal abrasion, which is a scratch or scrape of the cornea. It’s a good idea to check with a healthcare provider who can refer you to an eye expert. They can then examine the cornea for scratches and identify the offending lashes.
Treatments are based on what is found. If there are scratches on the cornea, a soft contact bandage may be applied to protect the eye while it heals. How you ultimately remove ingrown eyelashes depends on how many you have and how persistent they are. Here are some common treatments for an ingrown eyelash.
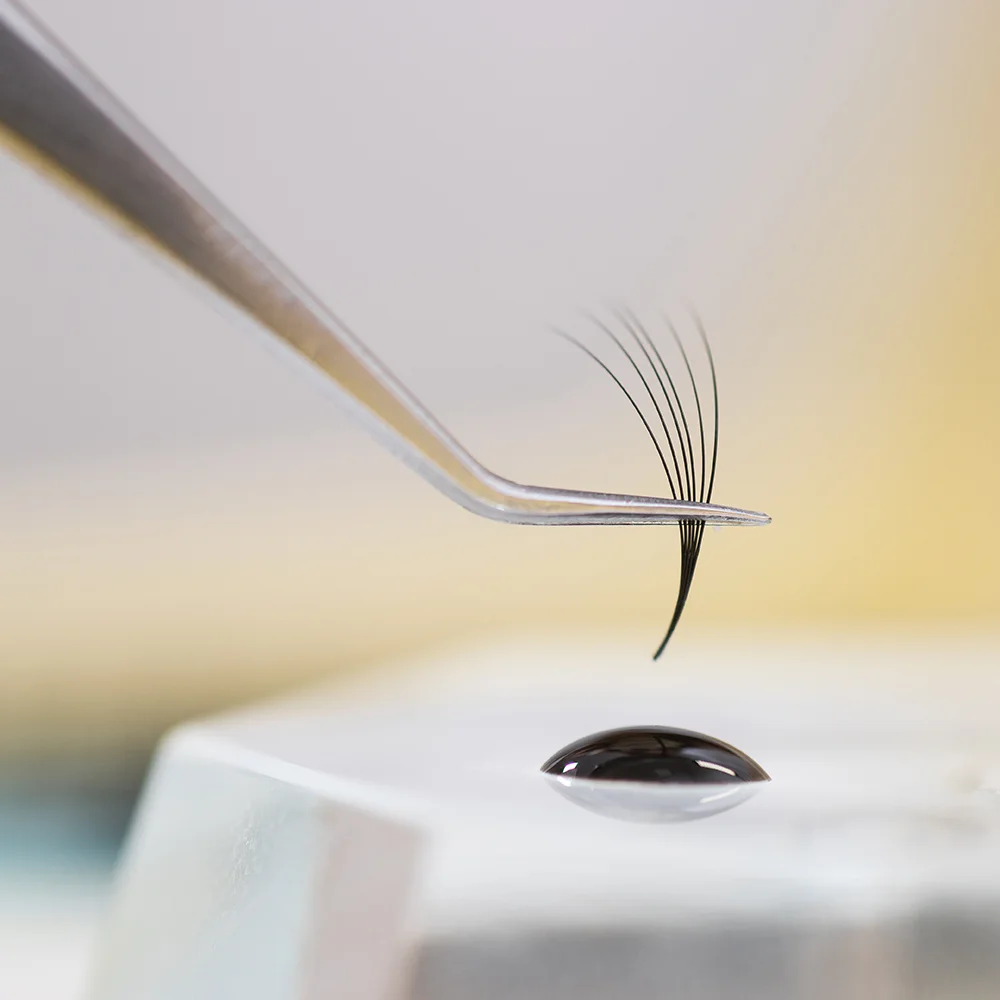
Epilation (tweezing)
Depending on how many ingrown lashes there are, you’ll likely be given anesthetic eye drops before the epilation procedure. The offending lashes are then removed with tweezers or forceps. Wait about 1–2 months (about how long it takes for eyelashes to grow back) before scheduling a follow-up appointment to see how the regrowth is going.
If they’re still growing in the wrong direction, your healthcare provider may advise continued tweezing or a more permanent solution (Patel, 2021).
Permanent eyelash removal
In worst-case scenarios, eyelashes can be permanently removed to stop them from growing back. The following procedures involve an office visit and anesthetic (Patel, 2021; Bezerra, 2021):
Electrolysis (a small electrical current destroys the hair)
Radiofrequency needle
Argon, ruby, or diode laser
Cryotherapy or cryosurgery (liquid nitrogen is used to damage the lash root)
Surgical methods of eyelash bulb removal
Repositioning eyelashes
There are also techniques that surgically reposition lashes rather than permanently remove them. Repositioning eyelashes has been shown to be successful (Karademir, 2021).
If you’re looking up trichiasis treatment online, you’ll a lot of information about trachoma trichiasis. This is a condition that affects more than eight million people in developing nations where trachoma—a serious eye infection—often leads to trichiasis and blindness.
In countries like this that have limited medical access, surgical techniques and at-home tweezing of eyelashes are common approaches to prevent infection and vision loss. Trachoma eye infections are not seen very often in the United States (Habtamu, 2015; Burton, 2015).
Preventing ingrown eyelashes
Some causes of ingrown eyelashes are not preventable, like the changes that come with aging or from necessary surgeries affecting the eye area. To prevent an ingrown eyelash, here are some practices that will reduce the chances of eye inflammation or infection (Bragg, 2021; Aumond, 2018):
Keep your fingers out of your eyes
Always wash your hands before touching your eye area
Remove make-up on lashes and around the eyes at night
If you wear contact lenses, keep them clean and remove if irritation starts
Use a warm compress or clean cloth to loosen debris around the eyes
Use tear-free shampoo (like baby shampoo) to remove and reduce bacteria around the eyelashes and ducts
If you end up with blepharitis or a stye, check with your healthcare provider about the best way to address the infection and reduce eyelid inflammation. Eyelid scrubs and debris removal are often combined with an antibiotic or an eye ointment, depending on the condition (Aumond, 2018).
If you have skin conditions like seborrheic dermatitis, a common cause of dandruff and psoriasis, that affect the eye area, there are treatments that can help. It’s best to take extra care removing skin build-up near the eyes, which can lead to ingrown eyelashes. Seeing a dermatologist and an ophthalmologist is a good approach when dealing with a skin condition close by the eyes (Wang, 2020; Rajguru, 2020).
Tea tree oil is one home remedy shown to have antifungal, antibacterial, and anti-inflammatory properties. It can be used to treat some conditions, such as eyelash mites, which can lead to blepharitis (Savla, 2019). However, it’s best to speak with your healthcare provider before trying over-the-counter tea tree oil, as it can come in many different concentrations and combinations with other oils that may potentially irritate the eye.
When to see a healthcare provider
Anytime you’re dealing with an eye condition it’s important to get medical advice––especially if pain or blurry vision is involved. If you suspect or know you have an ingrown eyelash, a board-certified ophthalmologist or optometrist can take a look to see if there are any scratches affecting the cornea.
Your healthcare provider may suggest ways to manage the condition at home with follow-up visits based on how eyelashes regrow. They may suggest a permanent hair removal approach if initial treatments don’t work. Overall, it’s best to have it checked first and follow their advice to protect your eye health.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Aumond, S. & Bitton, E. (2018). The eyelash follicle features and anomalies: A Review. Journal of Optometry , 11 (4), 211–222. doi:10.1016/j.optom.2018.05.003. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6147748/
Bezerra, Galvão R., Lílian Fernandes de Sousa Meneghim, R., Roberto Padovani, C., & Artioli Schellini, S. (2021). Diode green laser in the lid trichiasis treatment. Journal of Ophthalmic and Vision Research . doi:10.18502/jovr.v16i3.9428. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8358756/
Bragg, K. J. (2021). Hordeolum. [Updated Aug 9, 2021]. In: StatPearls [Internet]. Retrieved Feb. 4, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK441985/
Burton, M., Habtamu, E., Ho, D., & Gower, E. W. (2015). Interventions for trachoma trichiasis. Cochrane Database of Systematic Reviews , 12. doi:10.1002/14651858.cd004008.pub3. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4661324/
Eberhardt, M. (2021). Blepharitis. [Updated Jul 17, 2021]. In: StatPearls [Internet]. Retrieved Feb. 4, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK459305/
Habtamu, E., Rajak, S. N., Tadesse, Z., et al. (2015). Epilation for minor Trachomatous Trichiasis: Four-year results of a randomised controlled trial. PLOS Neglected Tropical Diseases , 9 (3). doi:10.1371/journal.pntd.0003558. Retrieved from https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0003558
Karademir, S. & Agaoglu, G. (2021). Treatment of trichiasis by releasing follicle roots of eyelashes: A new technique. Plastic and Reconstructive Surgery–Global Open , 9 (3). doi:10.1097/gox.0000000000003480. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8099408/
Kumar, D., Rajguru, J. P., Maya, D., Suri, P., Bhardwaj, S., & Patel, N. D. (2020). Update on psoriasis: A Review. Journal of Family Medicine and Primary Care , 9 (1), 20. doi:10.4103/jfmpc.jfmpc_689_19. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7014874/
Patel, B. C. (2021). Diseases of the eyelashes. [Updated Dec 22, 2021]. In: StatPearls [Internet]. Retrieved Feb. 4, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK537100/
Savla, K., Le, J. T., & Pucker, A. D. (2019). Tea tree oil for demodex blepharitis. Cochrane Database of Systematic Reviews . doi:10.1002/14651858.cd013333. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6556368/
Wang, L. & Deng, Y. (2020). Malassezia species may play potential roles in the pathogenesis of Meibomian gland dysfunction. Medical Hypotheses , 144, 110137. doi:10.1016/j.mehy.2020.110137. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33254481/