How Ro helped patients navigate a sudden CVS Caremark change with speed and scale
Ro fights to help patients access the treatment they need to achieve their health goals – not just when they’re getting started, but throughout every step in their journeys. Recently, that ongoing support was put to the test when thousands of patients faced a new hurdle to accessing their GLP-1 medication. Here’s how Ro stepped in to help.
In May, CVS Caremark, one of the nation's largest pharmacy benefit managers (PBMs), announced that they’d no longer cover Zepbound (tirzepatide) for weight loss. In short, the PBM reduced the treatment options available to its members, even those for whom it had previously authorized coverage.
For the thousands of patients in the Ro Body membership with Zepbound coverage through CVS Caremark, this wasn’t welcome news. Zepbound has been proven to be a highly effective treatment, and Ro’s data shows that the median Zepbound copay for those with coverage is only $76/month.
It’s clear why patients were frustrated to hear that a PBM was restricting their access, especially for those who have already:
Taken the brave step to start treatment;
Secured insurance coverage through Ro;
And began to make progress toward their health goals.
Ro knows that an unexpected change can bring stress to a patient’s journey and introduce questions about the cost of their treatment, efficacy of alternative options, or disruptions to their treatment journey. That’s why we made tackling these changes part of the Body membership, so patients always have someone in their corner, fighting on their behalf.
As soon as CVS Caremark made the announcement, our team leapt into action to make this policy update as seamless and easy as possible for patients who might be affected.
What we did:
1. Proactively educated patients about the CVS Caremark change
While this big policy change was prominently in the news, we didn’t want any patients to be surprised or left with questions when the change took effect on July 1. Three weeks in advance of the change, we communicated with patients to educate them about CVS Caremark’s update. In the communication, we assured them that, first, Ro had their back no matter what might change with their coverage and, second, that this wouldn’t affect everyone so not to worry until we checked if they were impacted.
2. Maximized access to prevent disruptions to patients’ treatment
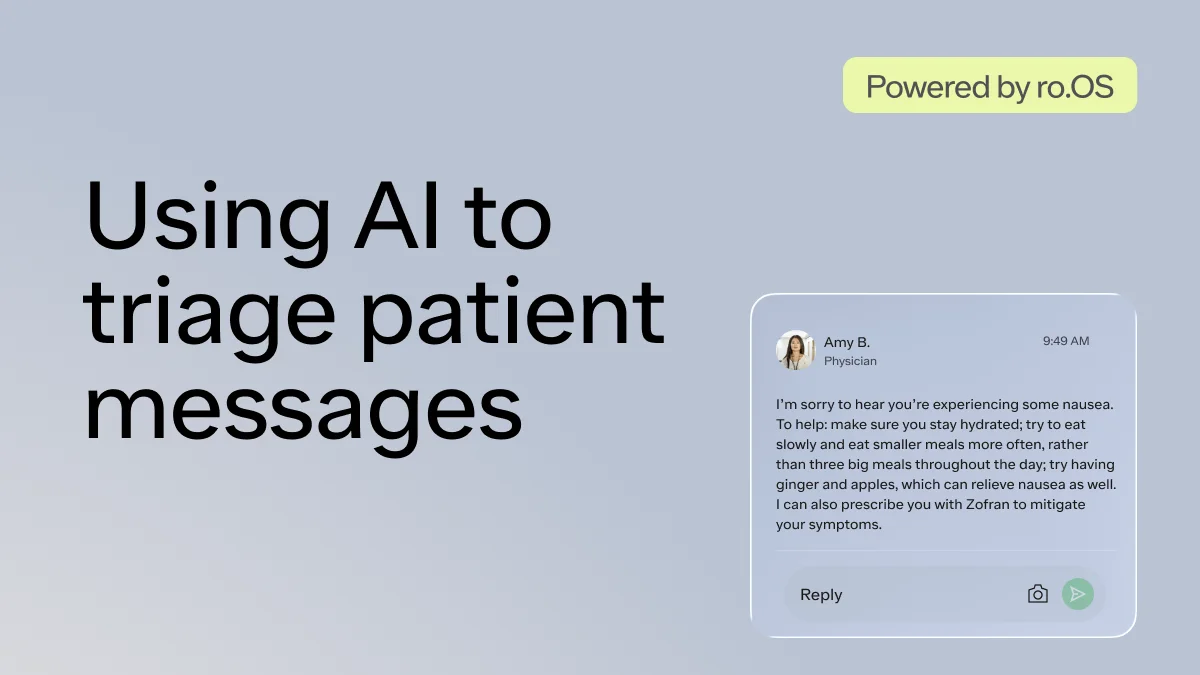
When a patient comes to Ro, they’re supported by a team spanning doctors and nurses, insurance experts, advocates who deliver support, and product and tech pros who build tools to make each patient’s journey seamless. Leveraging a suite of communications, task routing, insurance, and care management tools built on ro.OS (the Ro Operating System), this team got to work navigating the CVS Caremark hurdle.
Identifying all Caremark members with insurance coverage for Zepbound;
Re-checking each one of those patients’ coverage as soon as the policy went into effect;
Ensuring those who lost coverage were immediately prioritized in provider’s queues to review their treatment options and, when appropriate, prescribe an alternative;
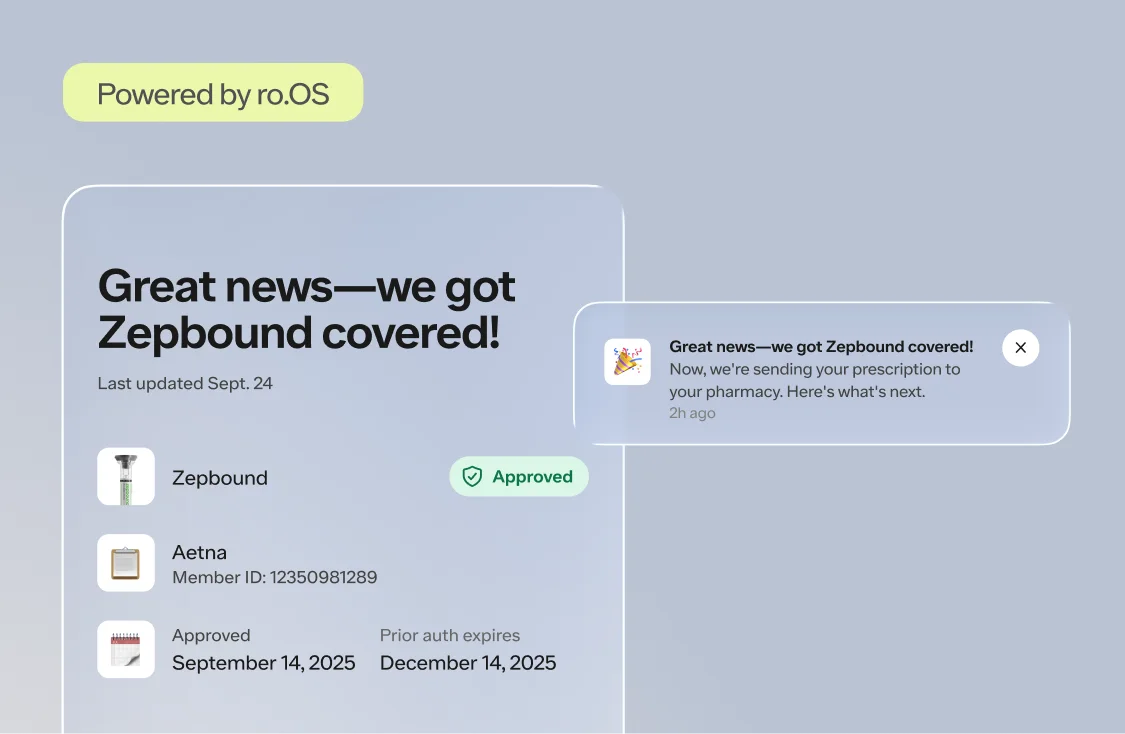
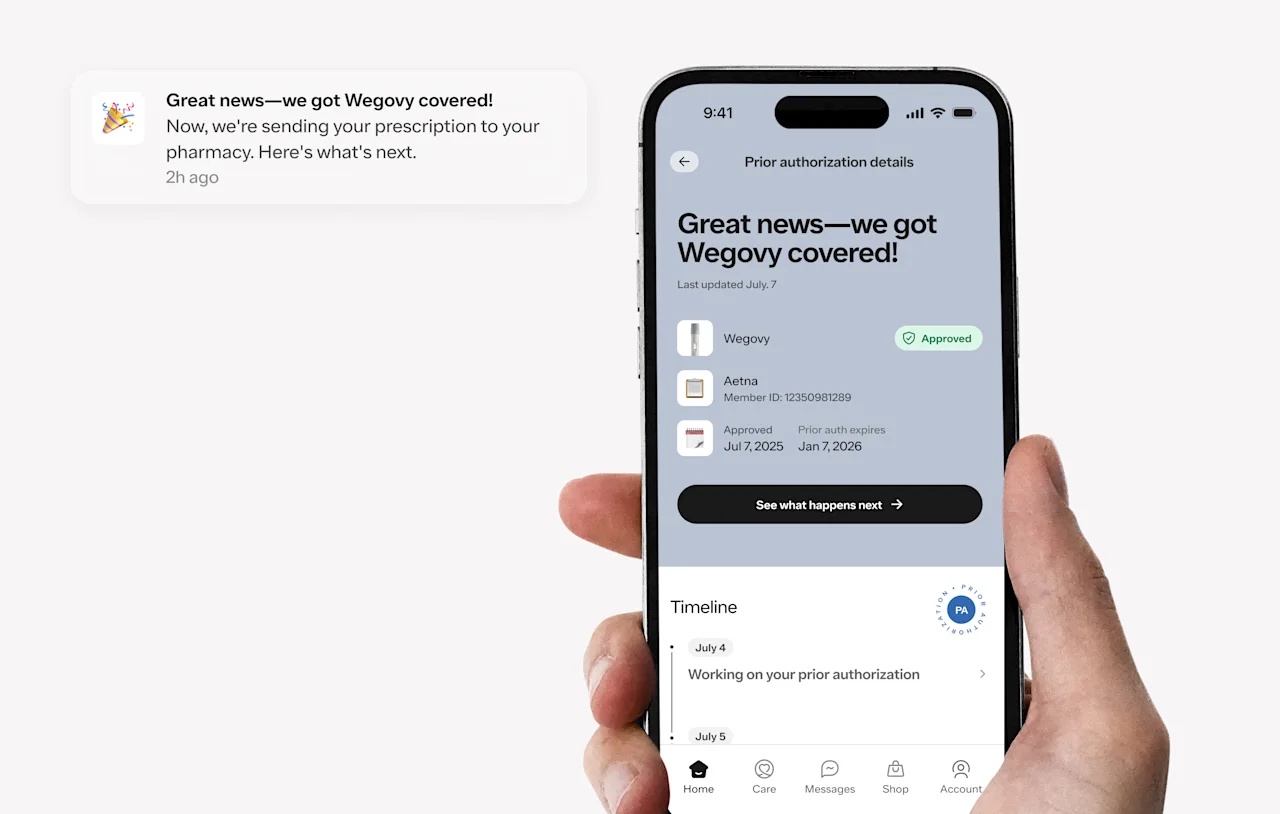
Notifying patients about any changes to their coverage and counseling them through their treatment options (i.e., switching them to an equivalent dose of Wegovy or Zepbound single-dose vials delivered through Ro’s integration with LillyDirect)
The results:
While we couldn’t undo CVS Caremark’s decision about Zepbound, Ro was committed to helping each patient continue on the best treatment journey available to them. With a platform and team built to handle challenges like this at scale, Ro:
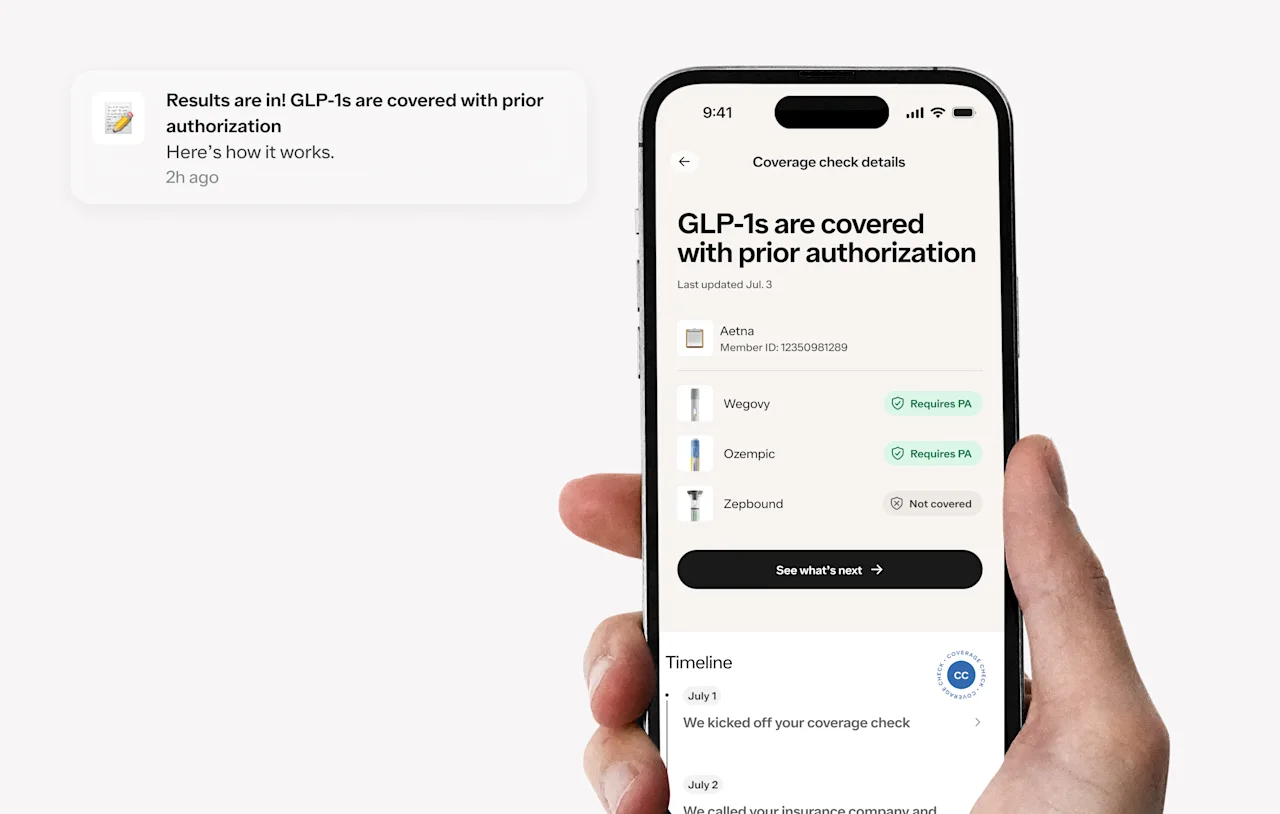
Completed more than 10,000 coverage checks in less than 72 hours;
Discovered that roughly 70% of patients maintained their Zepbound coverage, while only 30% lost it;
Confirmed Wegovy prior authorizations for those who lost Zepbound coverage, so they wouldn’t miss a prescription refill;
Made support available to patients who wanted to consider all of their treatment options as a result of the coverage change (i.e., file an appeal, switch to another medication, etc.)
Ro helps patients access effective treatment at the best possible price, whether their insurance offers coverage or not. For the 43% of patients with coverage of a GLP-1 for weight loss, navigating the insurance process is often worthwhile – since more than half of those pay $50/month or less.
The problem is, finding out what your insurance covers is anything but easy in the traditional system. Doctor’s offices or patients are forced to jump through hoops, make multiple phone calls, and link together piecemeal info just to get answers that might not be accurate. That’s why, Ro offers a free-to-anyone GLP-1 Insurance Coverage Checker that hundreds of thousands of people have used to understand their coverage.
It’s unfortunate that employers and health plans make changes that affect a patient’s treatment, especially once they’re well on their way in a successful journey. When these challenges are presented, Ro is dedicated to helping patients overcome any barrier – insurance, costs, or side effects – to make sure they can continue to progress toward their goals.