Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
The future of healthcare is one in which providers are not replaced but empowered by technology, unburdened from administrative paperwork, and liberated to practice medicine in concert with their patients where and when they need it most. Ro is striving to make this a reality every single day.
To make this vision a reality, it’s crucial that we offer what has been missing from health care for far too long — unrivaled transparency.
As Ro grows, I receive more and more questions trying to understand how physicians on Ro’s platform are able to offer high quality care at scale, how payment works, how we help uncover and potentially cure the serious underlying conditions, and how the provider platform works in general.
So, starting with this post and many more to come, we’re going to simply share. We will demystify telemedicine. We’re going to show you how the future of healthcare is coming sooner than you think. And, last but not least, we’re going to ask for your unvarnished feedback. We’re building this for you.
I’m going to share three real but anonymous cases on the Ro platform to show you:
How a physician can provide high quality care in as few as 2 minutes
How a physician can access more data points via telemedicine than in person
How telemedicine facilitates continuous, quality care after an initial diagnosis
Names will be changed to maintain privacy.
Average in-person visit
First, let’s level set. While there are many amazing things about the U.S. healthcare system, for the majority of Americans, it’s not working and we shouldn’t pretend that it is.
The facts (citations at the bottom):
An in-person doctor’s visit lasts ~13 minutes. Worse yet, NAMCS found these times are over-reported visit lengths by almost 4 minutes.
Average cost to see a PCP (Primary Care Physician) is $106, which would be 10% of someone’s monthly income on the poverty line.
Average wait to make an appointment is 29.3 days.
64% of primary care visits and 80% of specialist visits do not ask patients the purpose of their visit.
It’s estimated that physicians spend 40% of their clinical time on face-to-face visits, 40% on desktop medicine, and 20% on other activities when not logged into their EHRs.
86% of mistakes made in the healthcare industry are administrative.
So, here’s an in-person doctor visit in a nutshell: a patient waits 29 days to spend a few minutes with a physician, who often doesn’t ask why they are there and spends half the time looking at a computer screen. The visit costs the patient over $100, and if their heart or lungs are healthy, they are more likely to die from a typo than any other disease.
First case: Aaron - textbook case
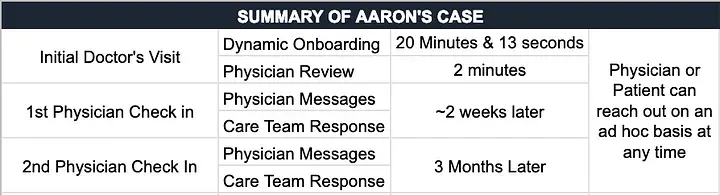
On Friday at 12:18 pm, Aaron started Ro’s dynamic patient onboarding seeking treatment for erectile dysfunction. He spent the next 20 minutes and 13 seconds providing a thorough overview of his health history and current symptoms.
Step 1: Aaron's online visit
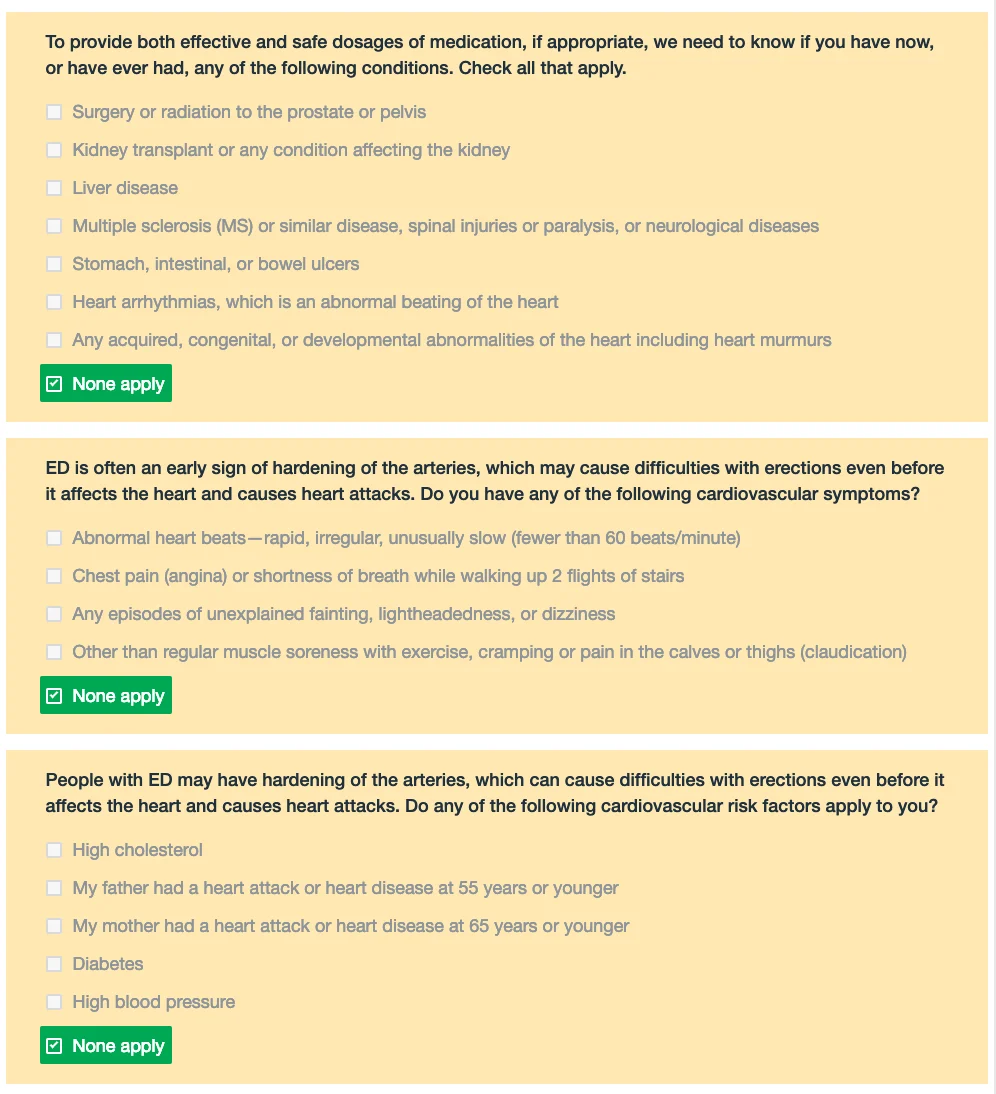
The most important concept to understand about Ro’s online visit is that it is dynamic, meaning that it changes depending on the individual patient entering information. As Aaron went through his visit, the system dynamically and intelligently collected and responded to information based on his unique medical history, biometric data, symptoms, medications, most recent physical, allergies and patient identification imaging, all of which was stored and forwarded to his physician for review.
For example, if Aaron had entered that he was a diabetic, the platform would have followed up with:
Are you on any medications for your diabetes?
What is your average daily blood sugar?
What was your last HA1C and how long ago was it?
Aaron isn’t a diabetic, so he wasn’t asked these questions. This is analogous to an in-person conversation with a provider or a medical assistant collecting information.

There are tens of thousands unique paths
During Aaron’s 20 minute visit, he addressed the following sections:
Demographic Information: 4 questions
Familiarity With Treatment: 1–3 questions
Current ED symptoms: 4–6 questions
Medical history: 15–42 questions
Current medications: 1–5 questions
Free form (i.e., open ended)
Identify verification: 2 image uploads
Location verification: 2 questions
Doctor Recommendation or Explicit Medication Preference: 4 questions
A few key points from Aaron’s case include:
Had no issues with his most recent physical (no physical abnormalities or cause for concern)
Had difficulty getting or maintaining erection and did not get an erection when waking up
Ruled out 49 other conditions, physical/mental symptoms, or family history indications that could have either created additional follow up questions or automatically made Aaron ineligible for treatment.
For a complete full list of conditions and lifestyle habits that we asked Aaron about, click here.
As Aaron answered questions, Ro’s software:
Eligibility: analyzed key information against evidence based protocols specific to erectile dysfunction
Drug Interactions: analyzed potential contraindications and risk factors based on medications, supplements, or allergies and flagged none
3rd Party Data: pinged a national third-party database to see if Aaron had any medications he forgot to mention while entering his medical history
As promised, let’s not gloss over anything. Let’s break down these three background processes. What’s actually happening?
Eligibility
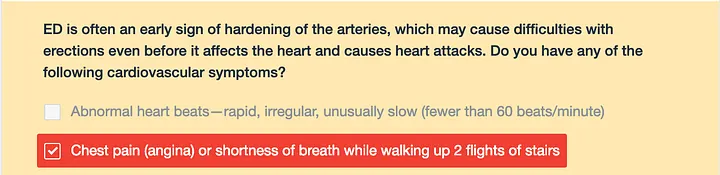
There are certain conditions, lifestyle choices, age ranges and other health information that would preclude a patient from being suitable for ED medication. Knowing treatment is medically restricted, we’ve built dynamic exit points directly into the online visit. To prevent fraud and abuse, not all exit points are the same and some wait until enough information has been collected to prevent duplicate online visits (i.e., someone coming in twice but answering questions differently).
Here is an example of what this looks like from a design perspective:
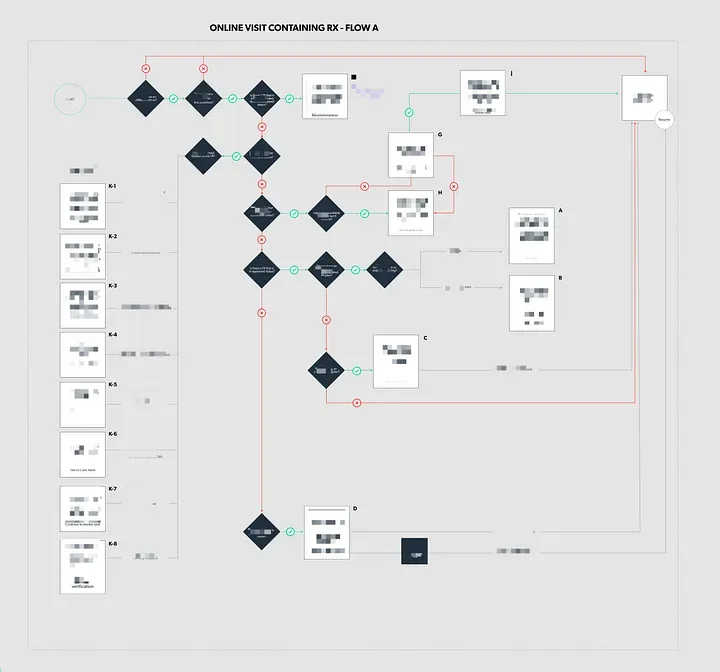
Drug Interactions:
A drug interaction is an effect produced by combination of two or more drugs together, which is different than the sum of the effects those drugs would each produce if used alone. When Aaron goes through the online visit, he provides the drug name, dose, and frequency of all medication he currently takes.
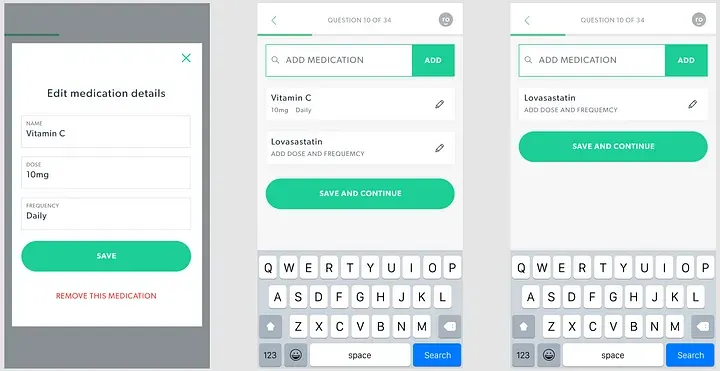
Ro’s software presents this information in an easily digestible, structured format to a physician that allows them to make informed decisions more easily.
3rd Party Data:
Close to 95% of pharmacies in the United States are part of a prescriptions clearing house called SureScripts. In order to be able to write a prescription to a pharmacy in the SureScript Network, an EMR has to be SureScript certified. The SureScript Network is valuable for patient safety because each prescription written through the network is shared among all providers and pharmacists. This prevents duplicate prescriptions as well as providing continuity of care across providers and pharmacies. For example, New York has passed a law requiring all prescriptions be electronic, which will dramatically reduce prescription fraud (i.e., someone using the same or a fake Rx to get multiple opioid prescriptions).
In the case of telemedicine, SureScript helps supplement the information a patient provides to his or her doctor by identifying the patient’s current and past electronic prescriptions in the SureScript Network. Meaning, if a patient, whether intentionally or unintentionally, leaves out an active or previous prescription while going through their initial online visit, Ro’s software automatically adds this prescription before presenting their information to their physician.
Cool, right?!
But this just captures a single moment. How does Ro’s software know what questions to ask? Aaron’s visit was the cumulation of analysis of millions of patient-physician interactions between patients and providers on the Ro platform.
In fact, it turned out that Aaron’s responses relating to his symptoms, medications, allergies, and risk factors were identical to tens of thousands of patients who used the Ro platform since Ro launched and to 1,745 patients in the last 35 days. This allows his physician to spend more time answering Aaron’s questions and his ongoing personalized treatment than on his initial diagnosis.
This is where telemedicine gets futuristic and will get your brain churning about all of the exciting ways we can improve patients’ lives with technology. Analyzing and leveraging uniquely large data sets is how Ro’s dynamic system gets smarter. It’s how Ro is able to ask the right questions at the right time and, hopefully, bring to light previously undetectable correlations in patient health and outcomes based on age, medications, biometric data, symptoms, family history, and location, and then present all that information efficiently to the patient’s physician.
Quick recap
Aaron spent 20 minutes and 13 seconds entering in his personal health information, ED symptoms, lifestyle habits, location, and verifying his identity.
During the 20 minutes, Ro analyzed all of his responses and matched them against knowledge from previous analysis of large data sets, collected the drug, dose, and frequency of current medication and supplement regimen, and pulled in any relevant active or passive prescription data from the largest prescription clearing house, which is the same one used by CVS, Walgreens, and Walmart.
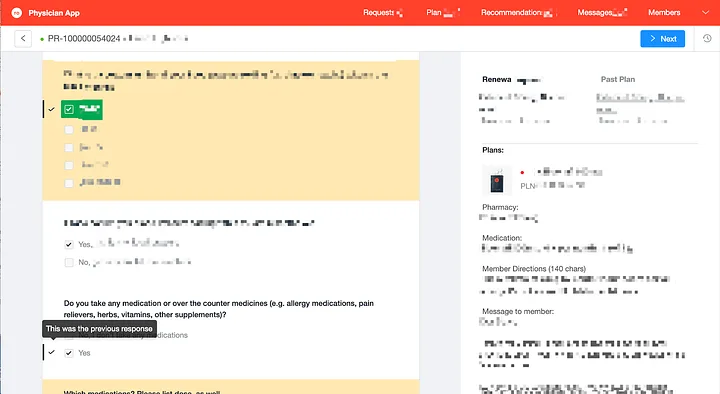
Step 2: Physician initial review
Aaron’s treatment request and information is then put into the physician queue, where only physicians licensed in Aaron’s state can pick up the consultation. Aaron’s doctor, let’s call him Dr. Phillips, pulls up Aaron’s submission.
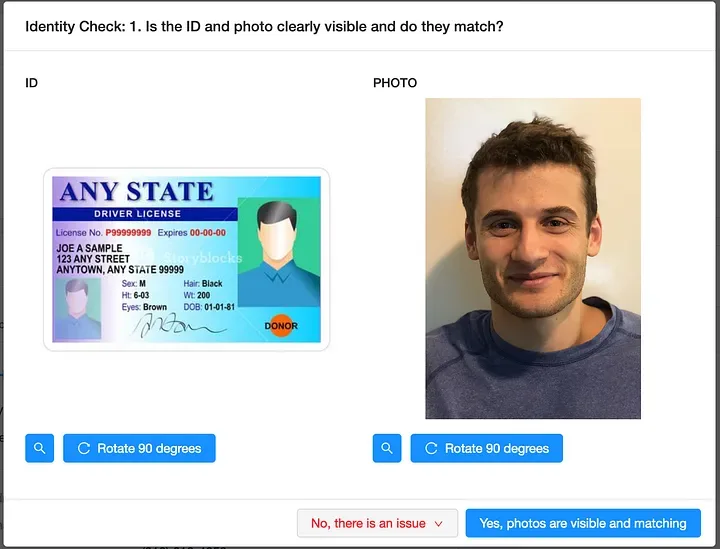
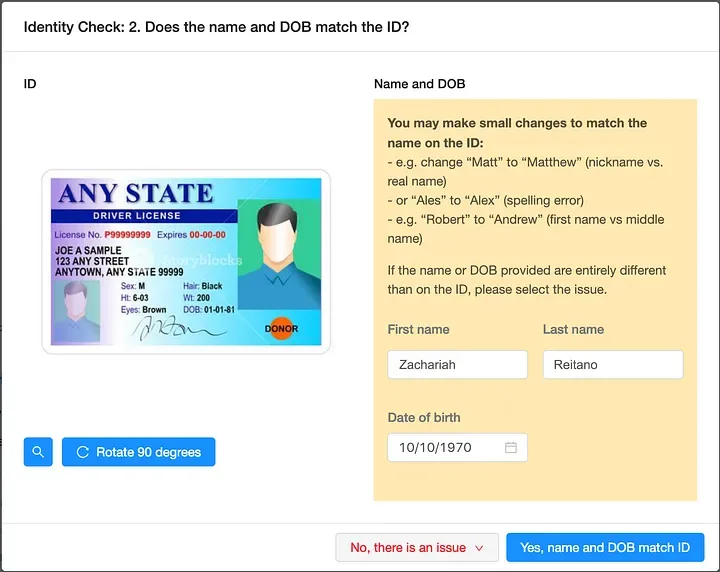
ID Check: Immediately, Aaron’s doctor is presented with Aaron’s ID and the image of his face, which have both been reviewed and analyzed by visual recognition software to prevent duplicates, blank images, and detect other anomalies.
A physician confirms that Aaron’s face matches his ID or tells the Ro system that Aaron needs to resubmit one (or both) of his photos and why. Here’s a mockup of what that looks like to the physician.
Treatment Review: all of Aaron’s medical responses are analyzed and presented, in their entirety, to the physician.
Here is the amazing part about telemedicine: By the time this information has arrived in front of the physician, the majority of people who started the online visit have been excluded from eligibility due to factors related to their health.
Approximately 14% of people who start their doctor visit are approved for treatment. Here is an example of how their information is presented to the physician upon review.
What if Aaron had answered differently? What would the EMR have displayed to his physician? What if Aaron had said he was having chest pain?
Ro’s software has made it incredibly easy for providers to do what providers do best, help each patient relating to what is unique about them — their questions, their concerns, their lifestyle habits, and their goals.
In Aaron’s case, the provider found that Aaron was a textbook case for ED treatment and that it was both safe and appropriate to write him a prescription. Here’s the message Dr. Phillips sent within Ro’s EMR system:
Hi Aaron,
Thanks for visiting Roman and taking the time to answer questions about your health.
My name is Dr. Bob Phillips. I’ve reviewed your health information and I think you likely have ED that can benefit from treatment.
I’ve sent a prescription for [ treatment selected by physician; obscured to maintain privacy ]
Prior to taking your medicine, please make sure to click on the Treatment Plan below. It will help you decide if the benefits of the treatment plan outweigh the risks, given the alternative options available to you, which include the option of not taking any treatment.
Link to treatment request (example here)
Also, please make sure to read the package insert that comes with your prescription. It will include a full list of potential side effects and warnings.
Please feel free to contact me if you have any questions by sending me a message.
Sincerely,
Dr. Bob Phillips
LINK TO PROFILE
Summary
After a total of 22 minutes, a patient was treated for ED via telemedicine.
But, when a physician treats patients through the Ro Platform, issuing a treatment decision is the beginning, not the end, of the patient-practitioner relationship.
From here, Ro provides:
Free blood test analysis.
We encourage all members to receive a blood test that could identify the underlying cause of their ED, and we work with Quest Labs to handle lab testing. Upon receipt of the lab results, a Ro physician will review the records and will schedule a free phone call or video chat with the patient to discuss the results and advise their patients regarding whether they should seek additional medical care.
Unlimited messaging, calls, or video chats at no additional cost to the patient
Regular Patient Check-ins
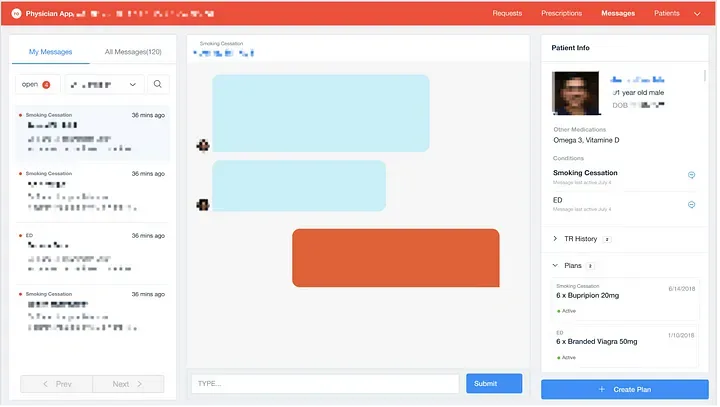
A smoking cessation program.
Smoking is the leading cause of preventable death worldwide and is often one of the main lifestyle causes of erectile dysfunction.
Ro is providing high quality, ongoing care by leveraging technology to reduce the barrier to more frequent, lighter touch interactions between patients and providers. This is key to unlocking affordable healthcare at scale.
While Aaron’s interaction took only 22 minutes, this level of safety and efficiency at scale is the result of tens of thousands of hours of hundreds of world leading medical experts, software engineers, and designers working day and night for two years at Ro. We want to build a world where the patient who needs 2 minutes now gets their issue resolved expeditiously, making it possible for a physician to spend 30 minutes with a patient who needs it (example below) and, in the future, maybe the patient who needed 2 minutes needs 30 minutes and vice versa.
Treatment plan overview
Dr. Phillips also provided Aaron with a treatment plan (example) that included:
overview of treatment
benefit of screening blood tests
important safety information
detailed breakdown of plan
biology of getting and maintaining an erection
difference in existing medications
common side effects
options if medication is ineffective
common alternative treatments
methods to improve overall health and reduce need for medication
ways to keep other healthcare providers in the loop and why it is important
contraindications and precautions; and
drug interactions from the Physician Desk Reference (PDR) and a link to the full PDR
Step 3: Dr. Philips follow up
2 weeks after the treatment arrived at Aaron’s home, Dr. Phillips proactively reached out to Aaron and sent the following message to check up on his treatment.
Hello Aaron,
I am checking in to see how things are going. I find it helpful to remind patients that the treatment plan we chose can take up to 8 tries to achieve the best results. However, if it hasn’t worked as you expected (even after only 4 or 5 uses), please reach out by sending a message through your MyRo account.
I can work with you. We can try a different dose, see if a different medication may be more effective, or just decide to give it more time. If you experience any side effects, please, let me know that too. We could try a lower dose, which may still be effective while reducing, or even eliminating, any side effects.
There is no fee for following up if there’s anything you’d like to discuss. We want nothing to stand between you and your healthcare goals. Being informed is the best way for us to work as a team in giving you the care you deserve.
If you have any questions related to shipments, billing, or your account, reach out to the Ro Care Team by emailing [email protected] or calling (888) 798–8686
Best,
Dr. Bob Phillips
Aaron responded that everything was good.
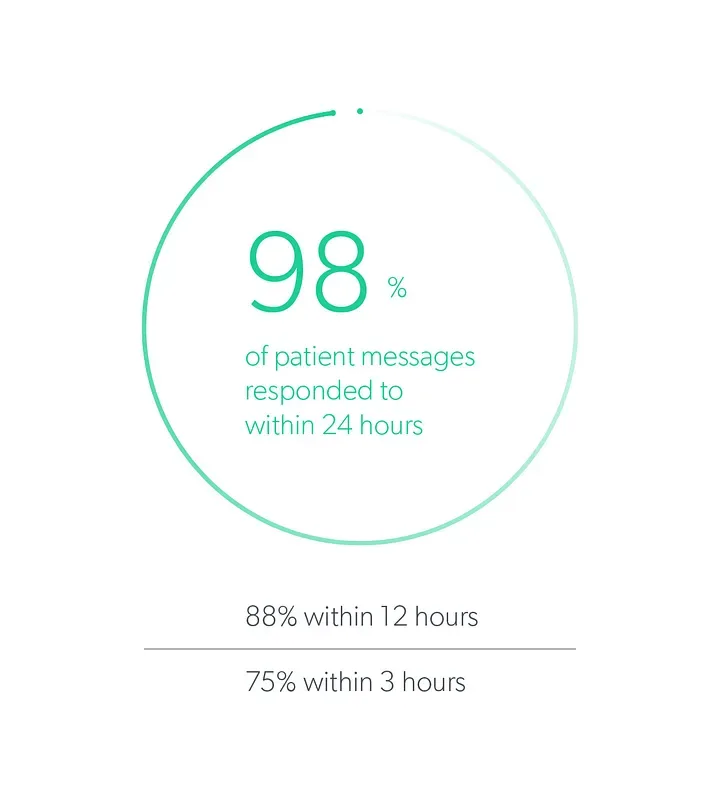
By leveraging technology, Aaron was able to receive high quality treatment from the comfort of his home, first by spending 20 minutes, then having a doctor spend 2 minutes, then having the doctor follow up two weeks later and creating a relationship that will last for years.
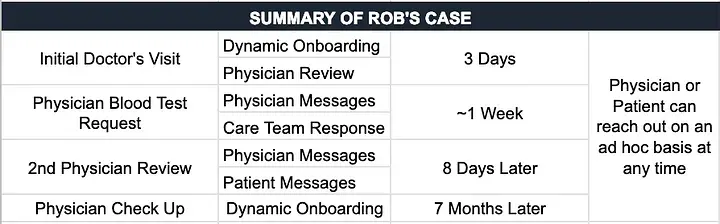
Second case: Rob - request for further medical record
Rob is in his late 40s and it took him 2 days to complete the online visit. He filled out 28% in his first session at 6:42 pm on Sunday and then completed the remaining 72% at 12:33 am on Tuesday (19 minutes in total).

Ro enables anyone to pick up where they left off if they can’t complete the initial onboarding in a single session. Before now, Rob could do this with TurboTax, but not healthcare.
At 7:33 am the next day, Rob’s physician, Dr. Abram, began reviewing his treatment request and something in Rob’s history caused his doctor to ask if he could share his most recent lab test.
RECAP: Rob was able to complete his initial onboarding after midnight and his doctor was able to review over her morning coffee.
Rob submitted his blood test a few days later to the Ro Care Team, who shared Rob’s full panel with his physician using a private and secure file storing service.
It took 11 days, 15+ messages, 2 Blood test summaries before Dr. Abram approved Rob for ED treatment.
Since then, Rob has had a dynamic follow up visit, which is required if a patient wants a medication refill or their prescription has expired. He completed his follow up visit at 4:32 pm and Dr. Abram reviewed the results at 4:46, 14 minutes later.
Since, Rob received a check-in through the Ro platform. It included condition and treatment specific questions like:
Whether or not his medication and dose have been effective
Whether or not he was experiencing any side effects
Whether he preferred to open a dialogue about changing his treatment
Whether he experienced the new onset of any of new symptoms in the past 12 months
The follow up visit is analyzed in the same exact way as the original dynamic onboarding.
Again, Ro’s platform empowered and augmented a provider.
In addition to garnering new information, follow up visit responses are cross referenced against previous responses (or additions made to Rob’s chart in the interim) to ensure that Dr. Abram can see Rob’s progress over time.
Traditionally, in medicine, Rob’s chart would be a series of distinct and loosely attached visits. But with Ro, his “chart” is a coherent, cumulative history of his interactions with his physician.
Today, when you have a doctor’s visit, it’s likely you wait a full year (or maybe more) until you have another doctor’s visit. This makes it difficult to identify trends: After two years you can see a line, but it would take three years to see a curve (i.e., three data points).
More data, more touch points, and more interactions between patients and physicians will lead to better care. This is where telemedicine and software can allow Ro, and other technology companies, to change the way people experience healthcare.
Third case: Michael - uncover, and, solve, underlying cause of ED
Michael came to Ro on 3/18/2018 at 8:12 pm seeking treatment for ED. He spent 13 minutes and 28 seconds entering his information.
At 8:26 pm, his physician, Dr. Rosen, put his treatment consultation on hold. While there were no specific contraindications to treatment, Dr. Rosen learned that Michael smokes cigarettes, so Dr. Rosen called Michael and spoke to him about the risks of smoking and its connection to ED.
45 minutes later, Dr. Rosen approved treatment for ED for Michael. In addition to his treatment plan, he provided him with resources to help him quit smoking. Here is Dr. Rosen’s follow up message after their phone call.
Dear Michael,
Thanks for visiting Roman and taking the time to answer questions about your health.
Thank you also for speaking with me on the phone about your condition.
My name is Dr. Rosen. I’ve reviewed your health information and I think you likely have ED that can benefit from treatment.
I’ve sent a prescription for [ patient treatment obscured for privacy ]. Treatment Plan Link
Also, please make sure to read the package insert that comes with your prescription. It will include a full list of potential side effects and warnings.
Prior to taking your medicine, please make sure to click on the Treatment Plan below. It will help you decide if the benefits of the treatment plan outweigh the risks, given the alternative options available to you, which include the option of not taking any treatment.
Cigarette smoking is a leading risk factor for erectile dysfunction. If you think you may be ready to tackle this difficult issue, the first step is deciding to quit. If you think you may be ready, how do you do it? I find these steps can be very helpful:
— Call the national toll free number 1–800-QUIT-NOW. The Help Line will let you talk to a specialist to help you get started and will create a quit plan that’s especially tailored to you.
— Make an appointment with a healthcare provider, or contact a smoking cessation clinic to discuss your options.
— Set a quit date
— Create a “quit plan” which includes your reasons for quitting, develop tips that will help you quit so they will be ready for you to use when you need them, set your quit date,
— Identify who can help you when you need support
— Adopt new skills and behaviors you’ll need to help you cope.
— Get more information from the American Cancer Society about making the decision to quit, setting a quit date and choosing a plan. Click on this link for more help! https://www.cancer.org/healthy/stay-away-from-tobacco/guide-quitting-smoking.htmlRemember, a quit plan is central to your success!
Also, be prepared for challenging moments and difficulties, including relapse.
Please feel free to contact me if you have any questions by sending me a message.
Dr. Rosen
Profile Link
8 months later, Michael signed up for Zero, Ro’s end-to-end service for addiction, starting with smoking cessation.
5 months later, Michael no longer needs ED medication or smoking cessation medication.
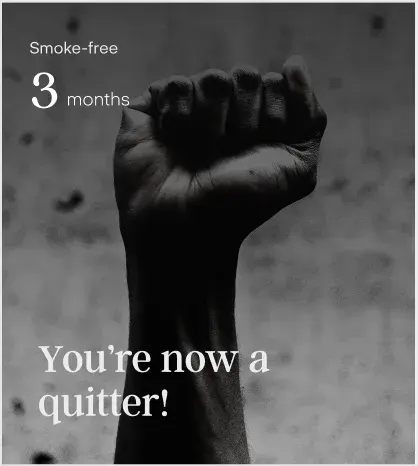
Almost one year since Michael’s first visit and he’s discovered (and fixed) the underlying cause of his ED, no longer needs ED medication, and stopped smoking before the age of 40. On average, smokers die 10 years sooner than non-smokers, but quitting before the age of 40 allows someone to gain 9 of those years back.
This is what the Ro team lives for. This why we believe in what we’re building.
It’s worth taking a moment and thinking about Aaron and the 30 million people who experience ED. Or the 50 million who experience herpes. Think about the people who avoid intimacy because they cannot hold their partner in an extended embrace. People who are scared about passing herpes on to their partner or even their child because they know that herpes can cause brain inflammation in children and lead to permanent brain damage. Those whose body is changing and sex, something that used to bring them and their partner great joy, is no longer an option. Think about how lost and scared they are.
I’ve been one of these patients and I’m sure many of you have too — whether it’s for a condition we treat or one we will in the future. You know how it feels to be lost, to be scared, and not know who to turn to.
We are who they turn to.
Every day, we help people who need a doctor. We help the 25 year old trying to quit smoking and the 40 year old trying to have a child. While Roman or Zero are not the end goal of Ro, it’s important to take a step back and recognize the incredible work our team is doing in the present.
On Ro’s platform, we have interactions that last 2 minutes, 2 days, 2 years, and hopefully a lifetime. What matters is how patients are treated over the course of their life as they experience health challenges.
Thanks for making it this far. It means a lot to us. In the next posts, I’ll cover:
Payment structure: how doctors are compensated and how we incentivize high quality care
ED can be a sign of a more serious underlying condition: how does Ro help get at the underlying cause?
What is Ro’s plan to expand beyond Roman (men’s health) and Zero (addiction) into women’s health?
References
Average duration of a doctor’s visit: 2016 Physician Compensation Report
Over estimation of duration of doctor’s visit: A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits.
Average wait time: A survey examining the time needed to schedule a new patient physician appointment in 15 major metropolitan areas
Average cost to visit primary care: health care cost institute
Did not ask purpose of visit: Journal of General Internal Medicine
Percentage of desktop medicine time: Medscape
Deaths from medical errors: Johns Hopkins & Journal of Patient Safety