Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Glucagon-like peptide-1 (GLP-1) receptor agonists have emerged as highly effective treatments for a variety of conditions including type 2 diabetes and obesity. In more recent clinical trials they have even been shown to reduce the risk of adverse outcomes in chronic kidney disease and the risk of major adverse cardiovascular events. Currently, researchers are studying the clinical utility of GLP-1s in mitigating neurological diseases such as Alzheimer’s, Parkinson’s and addiction.
In some areas, it’s clear that GLP-1s have clearly strong, positive effects on an individual’s health and well-being (i.e., diabetes, obesity), and in other areas, it’s not yet clear, but we may soon find the same (i.e., neurological diseases). However, the relationship between GLP-1s and mental health-related outcomes appears, by the available data, complex. In this article, we’ll look at one example of that relationship, the risk of depression and suicidal ideation, acknowledging this is just that – one example – and the relationships between GLP-1s and other aspects of mental health and well-being may differ greatly.
What we found: Currently the evidence does not show that GLP-1 medications increase the risk of depression or suicidality.
Overview
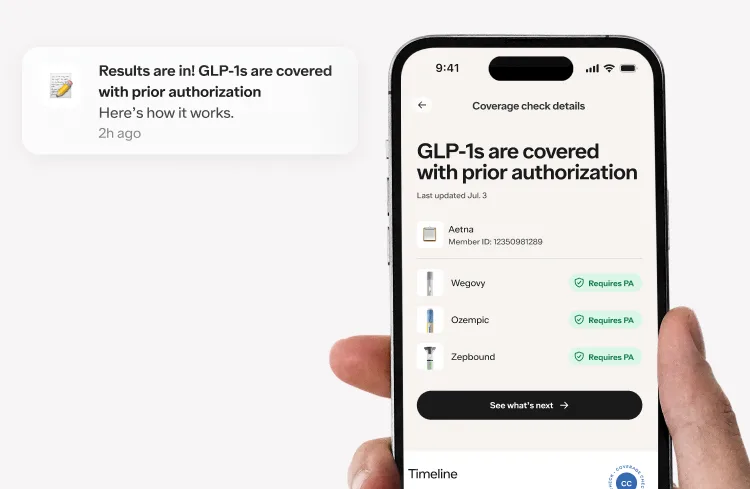
Since their approval, the labels for anti-obesity GLP-1s (Zepbound, Wegovy, and Saxenda) have included warnings about the potential risk for suicidal ideation and instruct healthcare providers to monitor patients and discontinue use if they experience suicidal thoughts or behaviors. These warnings are not a result of any direct causal link; instead they are a precaution stemming from findings in the Saxenda (liraglutide) trials where a small number of participants reported psychiatric symptoms (though these were not significantly different from the placebo group).
However, reports have raised concerns about the potential association between these medications and an increased risk of depression and suicidal ideation. These concerns have prompted regulatory bodies and researchers worldwide to investigate these associations and the possibility of a causal relationship, and continue to be a topic of interest into 2025. Findings from these investigations, and results from other studies, shed light on the relationship and what this means for patients.
Regulatory Investigations
In July 2023, the Icelandic Medicines Agency received reports about suicidal ideation in patients using GLP-1s, and the European Medicines Agency (EMA) initiated a review of a possible association between GLP-1 usage and suicidal ideation. Around the same time, the Food and Drug Administration (FDA) in the United States and the Medicines and Healthcare Product Regulatory Agency (MHRA) in the United Kingdom undertook similar evaluations. For all three of these investigations, the primary concern was whether or not GLP-1s were associated with increased levels of adverse psychiatric events, particularly with risk of suicide or self-harm.
Each of the regulatory bodies reviewed events reported via their respective adverse events reporting systems, formally known as spontaneous reporting systems (SRS). Manufacturers are required to report these events while providers and patients are also given the option (but are not required) to report adverse events.
The FDA’s adverse event reporting system, or FAERS database, is “designed to support the FDA’s post-marketing safety surveillance program for drug and therapeutic biologic products”. Following the release of a drug, the FAERS database collects adverse events reports from providers and patients that are witnessed in-market (i.e., in the real world practice of medicine rather than during a clinical trial or drug testing process). Most of these adverse events mirror those seen in trials, but on occasion, others only become evident upon widespread use. This is one of the primary reasons that real-world evidence is so important, as it can build upon the evidence generated during clinical trials with insights about safety and efficacy from a much larger, more diverse, and distributed patient population.
The FDA makes the data publicly available, enabling drug companies, clinicians and researchers to conduct their own analyses. Occasionally, analyses of that real-world data may show a signal of an unanticipated side effect. In the case of changes in mood and suicide risk, concerns raised from health authorities triggered formal investigations, while third-party researchers also analyzed the data from these databases for supporting evidence.
Investigatory Results: The results of the international investigations across three regulatory agencies were reassuring and aligned. The EMA, after analyzing approximately 150 reports, found no clear evidence of linking GLP-1 receptor agonists to increased risks of suicidal thought, or self-injurious behavior. The FDA and MHRA independently concurred with these findings. The FDA specifically stated that “our preliminary evaluation has not found evidence that use of these medicines causes suicidal thoughts or actions” while the MHRA noted that the “available evidence does not establish a causal relationship between GLP-1 receptor agonists and suicidal behavior, suicidal ideation, self-injury and depression.”
Taken together, these formal investigations did not reveal evidence of a causal relationship between the use of GLP-1s and suicidal thoughts, self-injurious behavior, or even depression.
The phrase “causal relationship” is important. Patients may have these feelings or behavior while taking a GLP-1, but none of the data that the regulatory bodies reviewed pointed to treatment with GLP-1 as the cause. Instead, patients might have been experiencing suicidal ideation prior to GLP-1 use, or experienced an unrelated external stressor while on the medication. There are many reasons an association can exist, but if the medication is not causing the adverse effect, then those associations are not a directly related safety concern.
Peer Reviewed Data and Research
At the same time that regulatory agencies were conducting their reviews, other researchers began publishing their findings. Reviews of multiple types of datasets (including, but not limited to, the same databases these agencies used) revealed similar findings. A review of comparisons of semaglutide (Wegovy, Ozempic) to non-GLP-1s in a large EHR database revealed a lower risk of incident and recurrent suicidal ideation among those treated with semaglutide compared to those treated with non-GLP-1 medications. That study showed that, for people with overweight or obesity taking a GLP-1, the risk of the incident (new occurrence) of suicidal ideation is almost 75% lower, and the risk of it happening again (recurrence) is over 50% lower. And, further, for patients with type 2 diabetes (T2DM) taking a GLP-1, the risks are reduced by about 60% and 50%, respectively.
In another evaluation of the FAERS data, McIntyre and colleagues observed disproportionate reporting of suicidal ideation and depression associated with liraglutide (Saxenda) and semaglutide compared to other glucose lowering agents. However, there was no increase in suicidal behavior, attempts, or completed suicide vs. any other GLP-1., Furthermore, while there was an increase in reports of suicidal ideation and depression in patients taking GLP-1 medications, there was no clear evidence that the GLP-1 medication was the cause. In a separate review of data available to the European Medical Agency, third-party researchers found no evidence that GLP-1 drugs like semaglutide led to suicidal thoughts or actions. Additionally, data from patients in Sweden and Denmark showed no statistically significant increase in the risk of suicide death among users of GLP-1 vs. another class of diabetes medications, SGLT2s. Finally, an analysis of some of the original trials for the use of semaglutide in weight management (STEP 1, 2, 3 and 5) found no significant increase in depressive symptoms or suicidal ideation/behavior. The analysis did identify a possible small reduction in depressive symptoms, but it was not a clinically significant difference.
While these findings were reassuring, there were other findings of note. A recent analysis of the World Health Organization’s pharmacovigilance database, VigiBase, found that there was an increased risk of suicidal ideation for patients taking semaglutide, liraglutide, and tirzepatide (Mounjaro, Zepbound) as compared with other medications for diabetes. Notably, though, there was a decreased chance of suicide attempts and completed suicides for patients taking liraglutide and semaglutide. These findings were similar to another analysis that showed disproportionately high reports of semaglutide associated suicidal ideation as compared with other medications for diabetes. The authors note that this risk was particularly evident among patients also using antidepressants. Additionally, evaluations of data from the TriNetX network, a global clinical data repository revealed a significantly increased risk of depression, anxiety, and suicidal behavior in those patients taking GLP-1 Receptor agonists as compared with other medications for diabetes., The most recent published research (January 2025), a large nationwide case-time-control study using data in France, found no evidence that GLP-1 use increased short-term risk of suicide or suicide attempt in patients with obesity or history of psychiatric disorders.3
What We Can Conclude
So what do all these findings tell us? First, the relationship between GLP-1 medications and depression and suicidality isn’t straightforward; reports on their association are conflicting. The word “association” here is very important. These studies and investigations are analyses of data that were not derived from randomized control trials, which are considered the gold standard for determining causal relationships. While it helps to leverage existing real-world data for cost-effective and time-efficient insights, this method can be challenged by potential biases, missing data, and lack of control over variables or study design. In particular, data in pharmacovigilance monitoring databases like FAERS rely on voluntary reporting which can be heavily influenced by media attention drawn to potential relationships. This can then create false signals where a medication appears to have a higher risk because of increased reporting, not actual incidence. That said, all of the studies have the same message: currently there is not enough evidence to prove that GLP-1 medications increase the risk of depression or suicidality.
Patients are prescribed GLP-1 medications to treat something about their health. For many it is obesity, and studies have demonstrated a significant association between obesity and psychiatric conditions. This association reflects a complex and multifactorial relationship between weight and mental health. For example, stigma and psychosocial stress associated with obesity may play a role, but there are likely many contributors. Therefore, we must be careful when we read these studies as there are many factors that may confound the link between medication and adverse effects like depression and suicidality.
We will continue to monitor and evaluate the potential relationship between GLP-1s and the risk for depression and suicidality. However, this is but one of the potential areas where GLP-1s may have links with mental health outcomes -- positively or negatively -- and we'll explore those other areas in future articles.
References
Perkovic, Vlado, et al. "Effects of semaglutide on chronic kidney disease in patients with type 2 diabetes." New England Journal of Medicine 391.2 (2024): 109-121. Lincoff, A. Michael, et al. "Semaglutide and cardiovascular outcomes in obesity without diabetes." New England Journal of Medicine 389.24 (2023): 2221-2232. Bezin, Julien, et al. "Suicide and suicide attempt in users of GLP-1 receptor agonists: a nationwide case-time-control study." eClinicalMedicine 80 (2025): 103029. European Medicines Agency. (2023, July 11). EMA statement on ongoing review of GLP-1 receptor agonists. https://www.ema.europa.eu/en/news/ema-statement-ongoing-review-glp-1-receptor-agonists U.S. Food and Drug Administration. (2023). FDA’s adverse event reporting system (FAERS). https://www.fda.gov/drugs/surveillance/fdas-adverse-event-reporting-system-faers Sakaeda T, Tamon A, Kadoyama K, Okuno Y. Data mining of the public version of the FDA Adverse Event Reporting System. Int J Med Sci. 2013 Apr 25;10(7):796-803. doi: 10.7150/ijms.6048. PMID: 23794943; PMCID: PMC3689877. Giunchi, V., Fusaroli, M., Hauben, M., Raschi, E., & Poluzzi, E. (2023). Challenges and opportunities in accessing and analysing FAERS data: A call towards a collaborative approach. Drug Safety, 46(9), 921–926. https://doi.org/10.1007/s40264-023-01345-w Becker, Zoey. "After Eight-Month Review, EMA Finds No Link Between GLP-1 Usage and Suicidal Thoughts." Fierce Pharma, April 12, 2024. https://www.fiercepharma.com/pharma/after-eight-month-review-ema-finds-no-link-between-glp-1-usage-and-suicidal-thoughts. https://www.fda.gov/drugs/drug-safety-and-availability/update-fdas-ongoing-evaluation-reports-suicidal-thoughts-or-actions-patients-taking-certain-type https://www.gov.uk/government/news/mhra-finds-evidence-does-not-support-a-link-between-glucagon-like-peptide-1-glp-1-receptor-agonists-and-suicidal-and-self-injurious-thoughts-and-act#:~:text=Following%20a%20thorough%20review%2C%20the,%2C%20self%2Dinjury%20and%20depression. Wang, William, et al. "Association of Semaglutide with Risk of Suicidal Ideation in a Real-World Cohort." Nature Medicine, vol. 30, no. 1, 2024, pp. 168–176, https://doi.org/10.1038/s41591-023-02672-2. McIntyre, Roger S., et al. "The Association Between Glucagon-like Peptide-1 Receptor Agonists (GLP-1 RAs) and Suicidality: Reports to the Food and Drug Administration Adverse Event Reporting System (FAERS)." Expert Opinion on Drug Safety, 13 Dec. 2023, https://doi.org/10.1080/14740338.2023.2295397. McIntyre, Roger S. "Glucagon-like Peptide-1 Receptor Agonists (GLP-1 RAs) and Suicidality: What Do We Know and Future Vistas." Expert Opinion on Drug Safety, vol. 23, no. 5, 2024, pp. 539-542, https://doi.org/10.1080/14740338.2024.2335215. Ruggiero, Rosanna, et al. "Glucagon-like Peptide-1 Receptor Agonists and Suicidal Ideation: Analysis of Real-World Data Collected in the European Pharmacovigilance Database." Pharmaceuticals, vol. 17, no. 147, 2024, pp. 1-11, https://doi.org/10.3390/ph17020147. Ueda, Peter, et al. "GLP-1 Receptor Agonist Use and Risk of Suicide Death." JAMA Internal Medicine, 3 Sept. 2024, https://doi.org/10.1001/jamainternmed.2024.4369. Wadden, Thomas A., et al. "Psychiatric Safety of Semaglutide for Weight Management in People Without Known Major Psychopathology: Post Hoc Analysis of the STEP 1, 2, 3, and 5 Trials." JAMA Internal Medicine, 3 Sept. 2024, https://doi.org/10.1001/jamainternmed.2024.4346. McIntyre, Roger S., et al. "Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and suicidality: A replication study using reports to the World Health Organization pharmacovigilance database (VigiBase®)." Journal of Affective Disorders, 2024. Schoretsanitis, Georgios, et al. "Disproportionality Analysis From World Health Organization Data on Semaglutide, Liraglutide, and Suicidality." JAMA Network Open 7.8 (2024): e2423385. Palchuk MB, London JW, Perez-Rey D, Drebert ZJ, Winer-Jones JP, Thompson CN, Esposito J, Claerhout B. A global federated real-world data and analytics platform for research. JAMIA Open. 2023 May 13;6(2):ooad035. doi: 10.1093/jamiaopen/ooad035. PMID: 37193038; PMCID: PMC10182857. Kornelius, Edy, et al. "The risk of depression, anxiety, and suicidal behavior in patients with obesity on glucagon like peptide-1 receptor agonist therapy." Scientific Reports 14.1 (2024): 24433. Leutner, Michael, et al. "Obesity as pleiotropic risk state for metabolic and mental health throughout life." Translational Psychiatry 13.1 (2023): 175.