Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
When it comes to family planning, understanding the factors that influence fertility is crucial. One of the most important markers for assessing a woman's reproductive potential is the anti-Müllerian hormone (AMH). This hormone serves as a key indicator of ovarian reserve, or the number of eggs remaining in the ovaries. As such, AMH levels are not just a reflection of a woman’s current fertility status but also a predictor of how long her reproductive window may remain open.
Given the significance of AMH in reproductive health, researchers have long wondered whether AMH levels could directly impact the chance of conceiving naturally. Although it has been hypothesized that serum AMH levels might serve as a predictive marker for conception, previous studies have had mixed results, largely due to limitations in study size. To shed light on this important question, Ro embarked on a comprehensive study involving 3,150 patients who had purchased a Modern Fertility hormone test and reported actively trying to conceive for more than three months.
Could AMH Levels Directly Affect the Chance of Conception?
Ro’s direct-to-patient platform allows us to scale care in a way that supports more patients in achieving their health goals. The expansive Modern Fertility patient population enabled us to explore the relationship between AMH levels and the time to pregnancy using the largest prospective cohort to date. A larger sample size allows for more robust and reliable data, with narrower margins of error. Our goal is that this research will equip patients and healthcare providers with the information needed to make informed decisions when planning for a family.
Here’s What We Found
Our research, published in the Journal of Fertility and Sterility, revealed a direct correlation between AMH levels and the likelihood of conception. You can read the full study here.
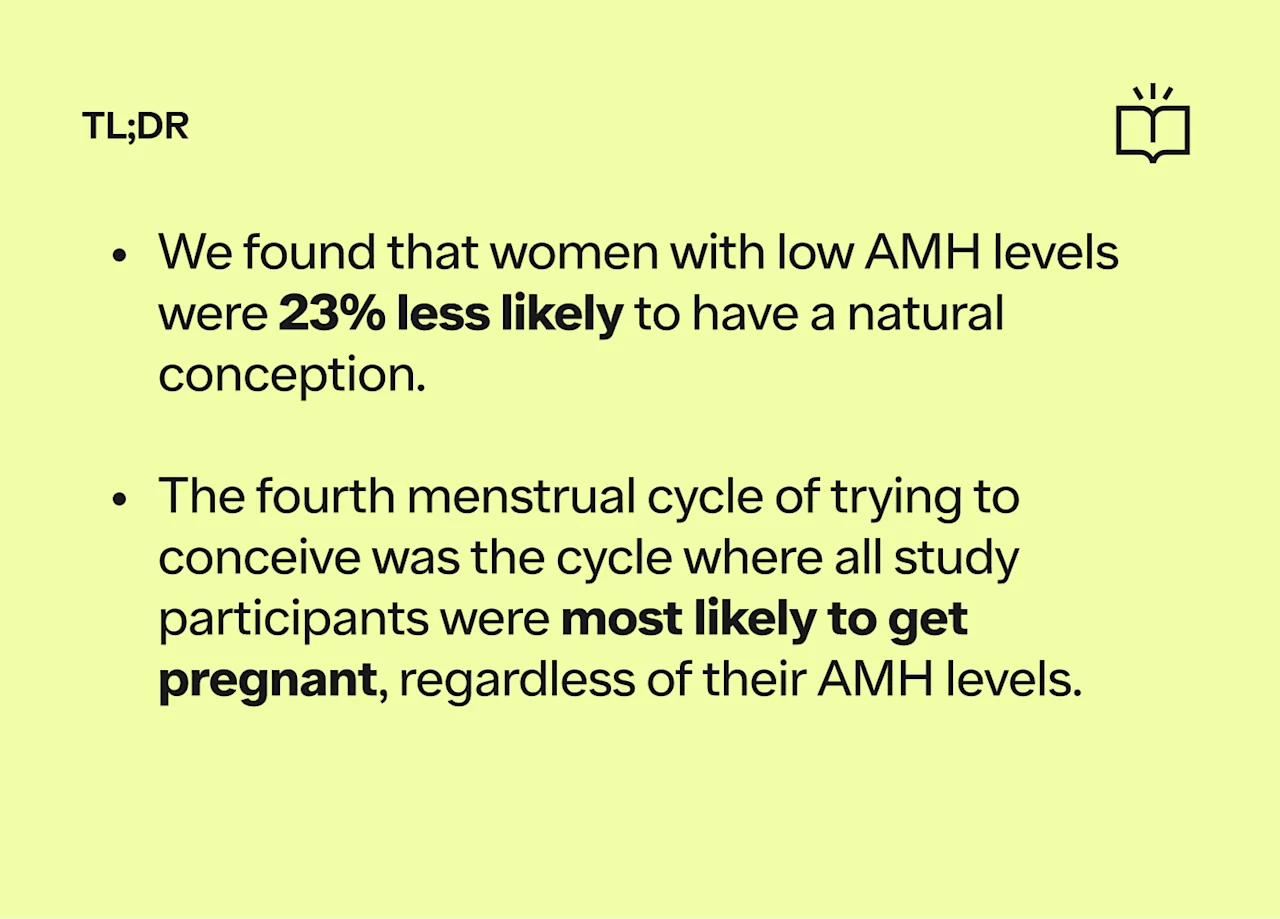
Among the study participants, 42% achieved pregnancy. When examining AMH levels, we found that women with low AMH levels (<1 ng/mL) had a statistically significant reduction in their chance of natural conception, with a 23% lower likelihood compared to women with normal AMH levels (1-5.5 ng/mL). There was no significant difference in conception rates between women with high AMH levels (5.5+ ng/mL) and those with normal levels
Interestingly, the instantaneous probability of conception peaked in the fourth cycle across all AMH categories. What this means is that for those in the study, the fourth menstrual cycle of trying to conceive was the cycle where they were most likely to get pregnant, regardless of their AMH levels. The likelihood of natural conception was as follows:
11.2% for low AMH levels
14.3% for normal AMH levels
15.7% for high AMH levels
Key Takeaways
Our research provides compelling evidence that low AMH levels are associated with a reduced chance of conception. This study, the largest cohort of its kind, offers new insights that can help physicians better counsel patients on their fertility journey. By understanding the implications of AMH levels, both patients and providers can make more informed decisions about family planning and fertility treatments. As we continue to advance our understanding of reproductive health, studies like this one underscore the importance of personalized care and data-driven decision-making in helping people achieve their family-building goals.