Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
New study compares one indicator of safety across different telehealth modalities on Ro’s platform
. . .
With the explosion of telehealth amid the COVID-19 pandemic, asynchronous care is becoming a common way to deliver healthcare services. Asynchronous care is a modality of telehealth that removes the need for the provider and patient to be available at the same time by making use of secure messaging and “store-and-forward” technology to enable patients and providers to communicate and send important information to each other at their respective convenience. In doing so, providers and patients can work together on an ongoing basis to create and manage an effective treatment plan.
Asynchronous care has become increasingly available in recent years, including through direct-to-patient healthcare companies like Ro. It’s also become more popular among patients for benefits including convenience, accessibility, and user-experience. Still though, more research is needed to study any differences in the quality, safety, or patient outcomes in this modality as compared with in-person or synchronous telehealth care.
Ro’s direct-to-patient platform enables patients and providers to connect via a variety of care modalities, including synchronous — audio and video visits — and asynchronous care. As such, Ro is uniquely positioned to contribute to the further study of asynchronous care.
What we analyzed
To advance our collective understanding of outcomes associated with asynchronous care, Ro’s Research Team studied side effects reporting across the different modalities of treatment on our platform. This research was conducted by Melynda Barnes, MD, Chief Medical Officer, Kevin Stern, Senior Manager of Data, Amy Westergren, Director, Senior Regulatory Counsel, and me.
This study built on research that Ro conducted last year that was published in the Journal of Urology & Research. That study focused on the rates of side effects experienced by patients being treated for erectile dysfunction (ED) through Roman, Ro’s digital health clinic for men. The analysis revealed that the types and distribution of side effects patients experienced were similar to other published research (though rates were comparatively lower overall). We also found that discontinued use of the medications at rates in alignment with published data in clinical trials.
In our follow-on study, we sought to identify whether there were any meaningful differences in reported side effects among patients who received synchronous (either a phone or video call) or asynchronous care. The rate of side effects reported is one important indicator of the safety of care.
What we learned
Our analysis evaluated the records of 10,000 patients on Ro’s platform to determine if asynchronous care leads to comparable or different patient outcomes in the form of patient-reported side effects.
Overall we found that patient-reported side effects were rare (less than 1.5%) and no serious adverse events were reported whether they received synchronous or asynchronous care.
Additionally, we found that:
1.12% of synchronously treated and 1.44% of asynchronously treated patients reported experiencing side effects;
There were no notable differences across the type or distribution of mild side effects;
There was not a statistically significant difference in the likelihood of an asynchronously or synchronously treated patient reporting a side effect.
These results suggest that asynchronous care delivered via Ro’s direct-to-patient platform did not lead to increased reports of side effects — an indicator of the safety of care — as compared with synchronous telehealth care.
This study is not without limitations. It is observational and only includes ED patients treated with one kind of medicine on a single platform. We will continue to invest in research related to asynchronous treatment on our platform to ensure we are facilitating care that is safe and effective, and hope that our study inspires other researchers to do so as well.
How this research drives innovation at Ro
The results from our studies on the rates of side effects reporting are promising from a safety perspective. However, we saw an additional opportunity to increase the rates of side effects reporting overall— even among patients for whom these side effects were mild and tolerable (i.e. the patients we suspect are not reporting them to their provider, whether in-person or telehealth).
If we could do so, this information could empower providers to offer patients better ongoing education and help to identify optimal treatments that support adherence and the best possible outcomes. Additionally, at scale, a more complete set of side effects data can be a powerful research and clinical tool, even for well-studied treatments.
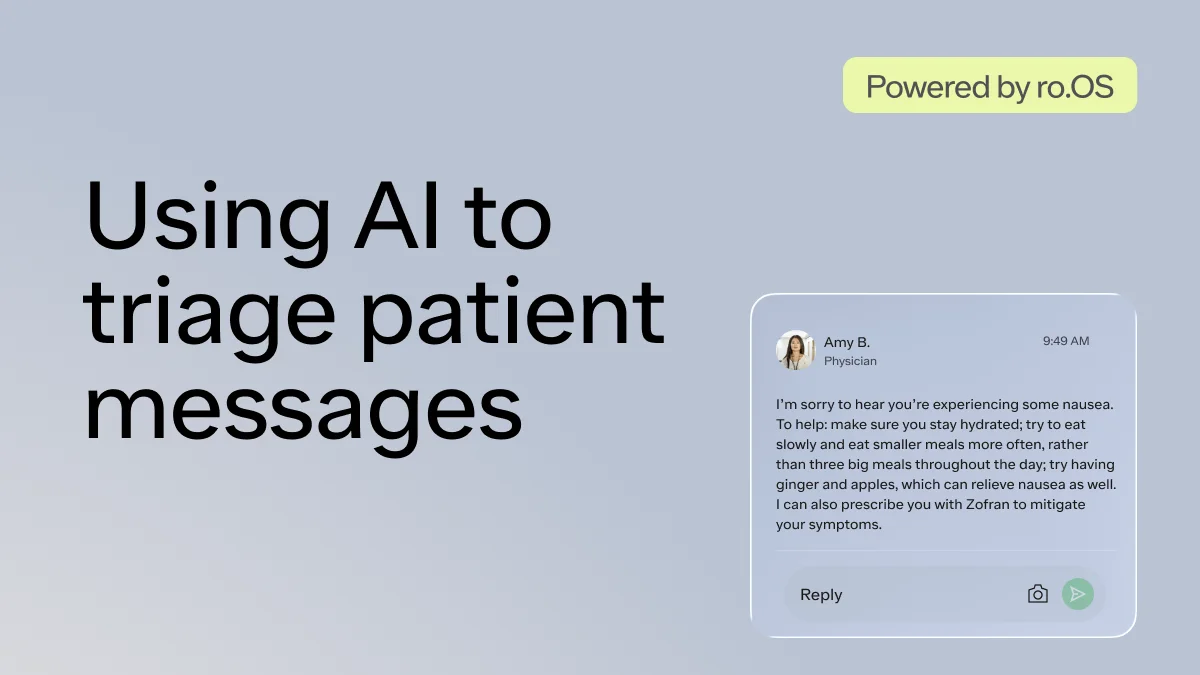
To support this more comprehensive view of our patients’ side effects, we launched an automated patient-reported outcomes data collection tool. This tool prompts patients to report whether they experienced any side effects and provides a button to allow them to connect with their provider via chat to discuss these experiences with them. We are still studying the impacts of this initiative (and plan to publish our findings), but so far outcomes have been positive: more patients are reporting side effects, connecting with providers to adjust their medication, and continuing their treatment plan.
Further considerations
Research like this, that focuses on the outcomes and safety of care delivered via telehealth, can facilitate defining standards, improving quality of care, and expanding treatment access to more patients and for more conditions.
In our efforts to support this research, we continue to study the patient experience, quality of care, and outcomes associated with care delivered through our direct-to-patient platform. This includes evaluating how the modality of care — synchronous or asynchronous — affects downstream measures. In this case, it was encouraging to see that our research indicated comparable patient-reported side effects among patients who received synchronous and asynchronous care.
More research is required to continue to evaluate the safety of asynchronous care across different conditions, circumstances, and outcomes. However, emerging evidence suggests that when appropriate, it can serve as another high-quality option for patients to seek the care that they want and need — while improving affordability, accessibility, and the patient experience. This is important because asynchronous care can help to address many of the factors that limit patients’ ability to get the care they need, including things like the fear or stigma associated with in-person care or access to broadband or video technologies for video visits.
As telehealth, including asynchronous care, continues to become a foundational part of the healthcare system, researchers and practitioners should focus on identifying the most ideal formats, processes, and approaches for collecting relevant clinical information, safely treating, and communicating with patients within the suite of virtual options.
Read the full study here: https://formative.jmir.org/2022/1/e32126
* * *
Please email me, Dr. Lauren Broffman, Ro’s Associate Director of Research, if you have questions or comments on this research or suggestions for future posts or insights. My email is [email protected].