Here's how technology can help
We are in the middle of a transformation in obesity care. GLP-1 medications are reshaping how we treat obesity, and they aren’t limited to just pounds lost on a scale. These medications improve cardiometabolic health, reduce the risk of developing chronic diseases and give many patients hope after years of frustration that they can take control of their health.
But here’s the truth: the promise of GLP-1s comes with a major challenge. Adherence is still low, and one of the biggest culprits is side effects.
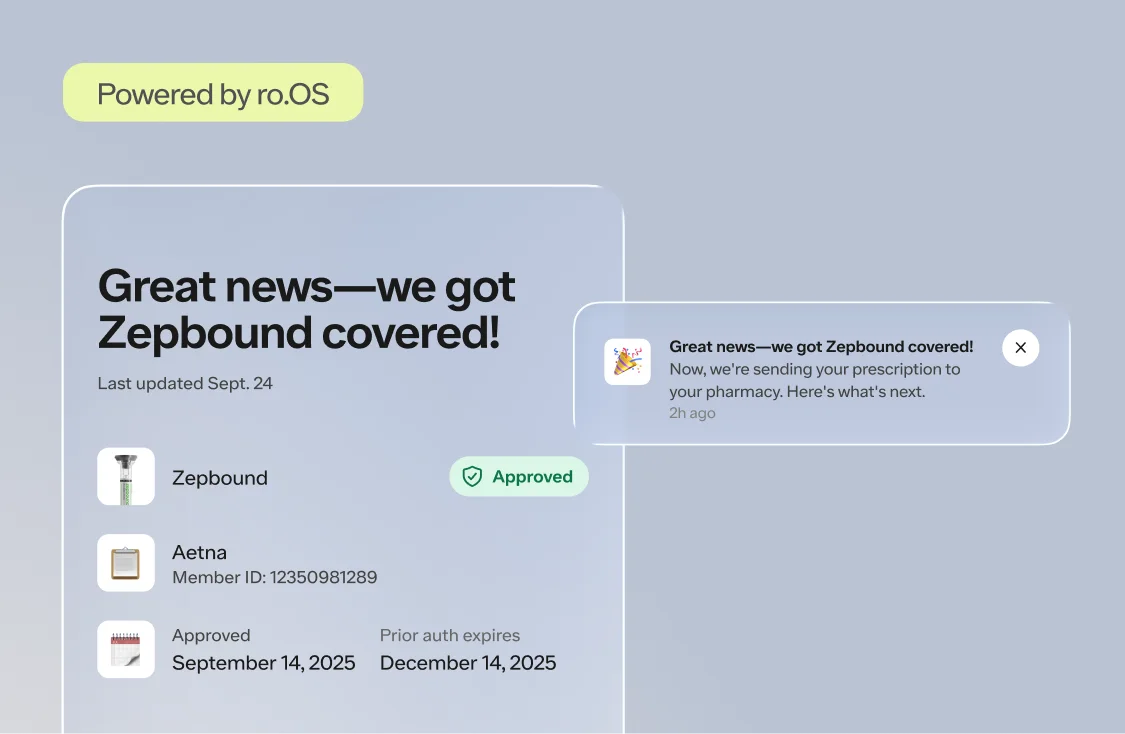
In healthcare, we often recognize that side effects are a barrier to success, but then we fail to equip patients with the support they need to manage them. We talk about adherence as a patient issue, when in fact it’s a care delivery system issue. When it comes to GLP-1s, it’s encouraging to see incremental progress on the well-known issues of cost and insurance coverage, which are obstacles to patients getting started or sticking with GLP-1s. But when it comes to side effect management, the healthcare system can—and should—be doing better.
The System is Not Set Up for On-Time, Personalized Support
Patients starting GLP-1 therapy should be well aware that side effects are possible–as their provider should educate them that these are powerful medications and side effects are common during dose titration. But knowing something might happen and knowing what to do when it does happen are two very different things.
The truth is, much of our care delivery system isn't built to help patients manage side effects in a timely, personalized way. The system assumes patients will not only speak up if something is wrong, but know how and where to reach their care team with those concerns. But that model doesn’t work when patients are feeling unwell, unsupported, and unable to access care outside of scheduled visits.
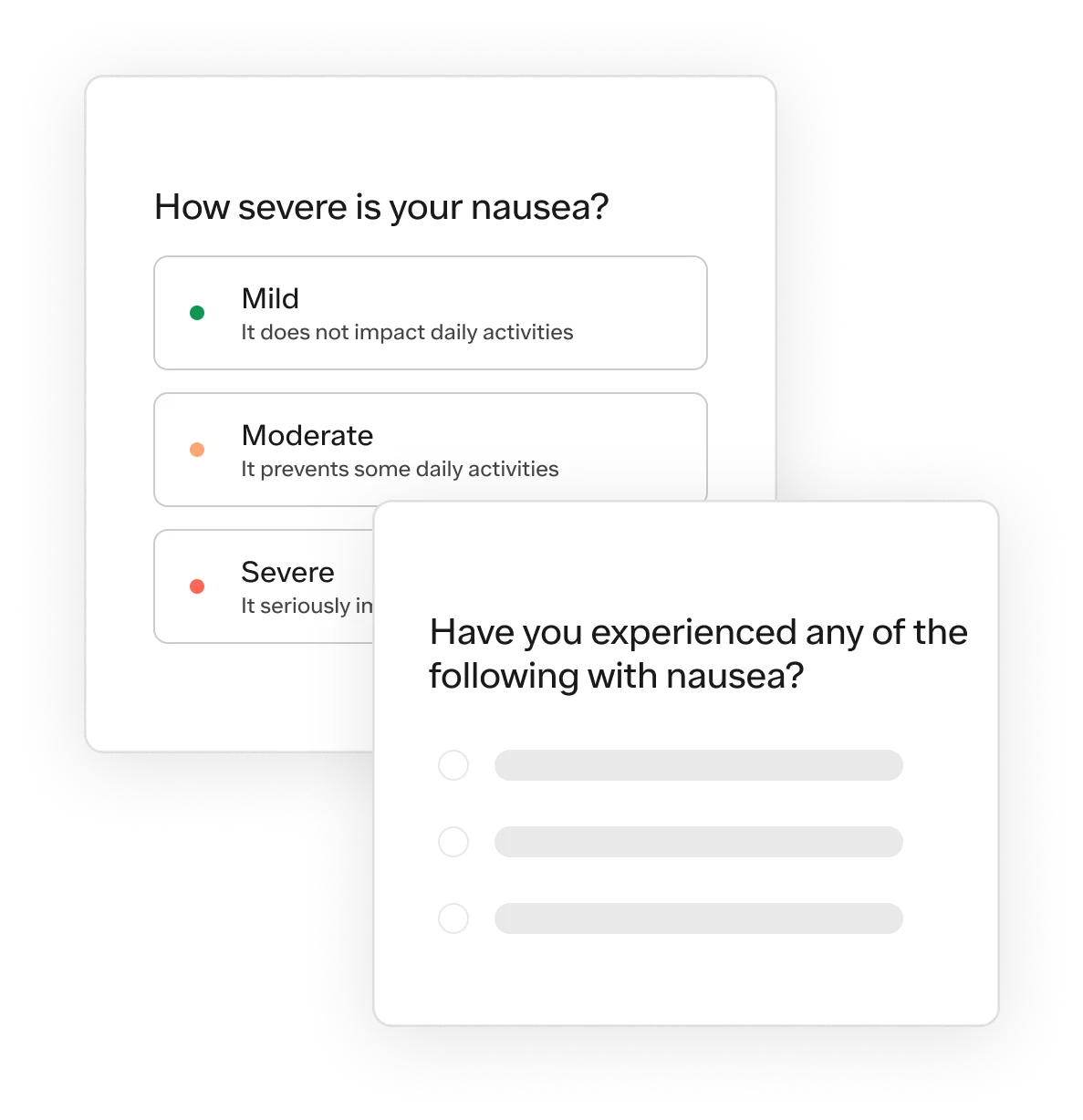
If we want people to stay on their treatment and to achieve the best possible outcomes, we have to meet them when and where they need us most. That means making it easier for patients to report side effects, for providers to understand their symptoms and severity, and for either party to communicate as needed to manage them.
What Data Shows about Managing GLP-1 Side Effects
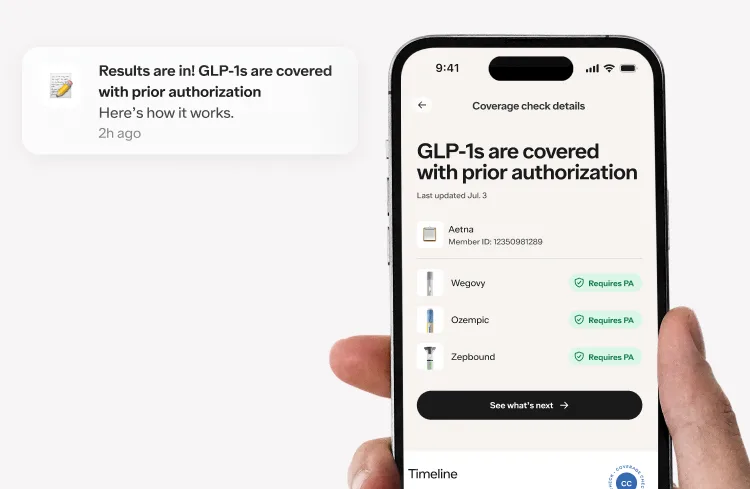
At Ro, we recently published research on patient-reported side effect data from thousands of patients treated with GLP-1s. Importantly, we looked at data from two different real-world scenarios when patients report side effects: first, when prompted during their regularly scheduled treatment check-ins, and, second, when they reach out unprompted on their own.
In the first study, we found that in nearly 40% of cases, the patient’s perception of severity didn’t match the clinical evaluation of severity. In 24% of those mismatches, the symptoms were more serious than the patient realized.
This mismatch matters. If a patient experiences a rapid heartbeat and ignores it, they could miss a sign for urgent care. On the other hand, if a patient is feeling overwhelmed by mild nausea that could be easily addressed but doesn’t know how to manage it, they might skip their next dose or stop treatment unnecessarily, risking continuity of care.
In the second study, we found that when given the ability to report side effects at any time via an asynchronous reporting tool: 43% of reports were submitted outside of regular office hours, 24% were submitted on weekends, and yet, across all times of day and week, the median provider response time was just 89 minutes (severe side effects were auto-escalated for immediate support).
These numbers underscore two things about what patients want and the system should strive to deliver: patients need support on their own schedule, and timely provider response can make all the difference—whether a patient is experiencing a severe reaction or a mild upset stomach.
Tapping Tech to Streamline Side Effect Management
Side effects are inevitable with GLP-1s, as they are with any pharmacological treatment. But when managed well, they don’t have to derail a patient’s journey. At its best, managing side effects is a safety measure, an adherence tool, and a patient trust builder—all in one.
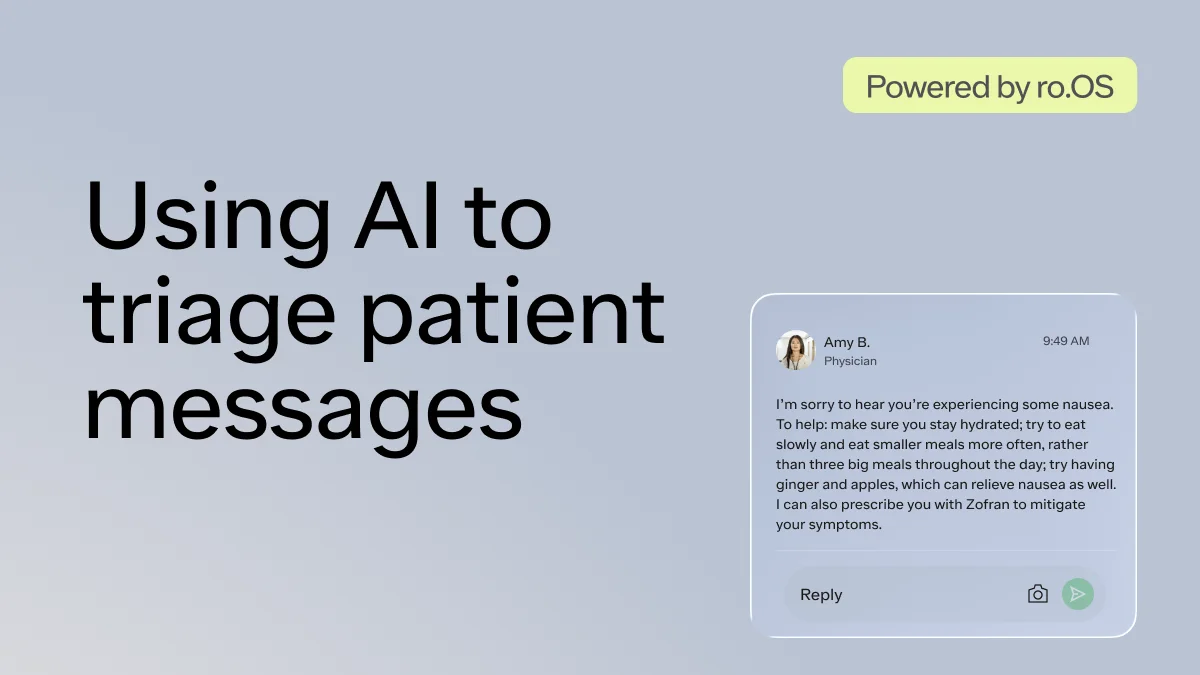
Side effect management should not be a burden for patients nor a black hole for providers. Digital health tools can help accomplish this. Telehealth can enable patients to report a side effect at 9:30 PM on a Friday via and receive guidance within hours—not days. Software can also help providers respond quickly to the most pressing issues first with smart triage tools while using data analytics to identify trends across thousands of patients. This creates a powerful feedback loop: patients receive timely, personalized support and providers stay ahead of adherence risks. This ultimately can improve care quality at both the individual and population level.
With the millions of people seeking obesity treatment, the future requires care delivery systems that can scale without sacrificing quality. These GLP-1s are powerful tools, but they’re tools that only work when people can use them long enough to see results. To help patients do that, we must rethink how side effects are reported, support is delivered, and care management is improved over time. With the right digital health technologies, we can help make side effects manageable for patients—even predictable for providers—and high-quality care easier for all. Patients deserve that level of support.