Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Obesity can be a key factor in and an indicator for one’s overall health. In fact, obesity is associated with a wide range of metabolic health risks that increase someone’s chances of developing some of the most prevalent and deadly chronic diseases (e.g., heart disease, stroke, diabetes, hypertension, and cancer).
The good news is research shows that weight-loss driven improvements in metabolic health can reduce downstream risk of developing or dying from these conditions. When Ro introduced our obesity care offering, the Body membership, we sought to help patients not only lose weight, but to improve their overall health. This was important to us because – even if someone’s primary focus is weight loss or a quality of life outcome – improving their metabolic health may help them achieve those goals.
The Body membership’s effect on metabolic health
To assess whether patients in the Body membership are achieving those improvements in their overall and metabolic health – as we always do at Ro – we studied the data.
For this study, we used metabolic lab tests. While lab tests are traditionally used to detect health issues on an individual level, they can also be used to track progress within a patient population. If the patient population is experiencing positive changes, lab results will reflect that. Conversely, if things aren’t improving, lab results will help us to investigate why. Just like measuring other clinical outcomes, lab results garner insights that help us continue to strengthen the Body membership for our patients.
Our lab results study posed the question: How are patients in the Body membership doing from a metabolic health perspective?
Which lab tests are relevant for weight management?
Tracking progress frequently includes weight logging and documenting behavioral milestones (i.e., diet and exercise patterns). But the following tests can also help track progress, and measure whether weight is lost in a healthy and sustainable manner:
Blood Sugar: Hemoglobin A1c (HbA1c) is a measure of the average blood sugar (glucose) levels over the past two to three months. Too high of an A1c measure means that a patient may have prediabetes or, if higher, diabetes. One of the key reasons tracking HbA1c is so important during weight loss is its connection to insulin resistance. When insulin resistance occurs, the body needs to produce more insulin to keep blood sugar levels in check. High insulin levels can promote fat storage and make it more difficult for the body to burn fat.
Lipid Profile: Losing weight can often lead to improvements in cholesterol levels, but this isn’t always the case. A lipid profile typically includes total cholesterol, LDL (bad cholesterol), HDL (good cholesterol), and triglycerides. These markers are crucial for understanding cardiovascular health. High levels of LDL cholesterol and triglycerides, combined with low HDL cholesterol, is associated with increased risk of heart disease. Tracking these levels helps ensure that weight loss isn’t negatively affecting heart health and that fat is being lost in a safe, effective way.
Our study: sample and methodology
One lab test gives you a snapshot of a patient’s health. To get a sense of population health, especially to measure the efficacy of GLP-1 treatments and care delivered in the Body membership, it’s helpful to track lab results over time.
In 2023, we collected thousands of baseline metabolic lab tests. The dataset is a valuable source of population health data, as it reveals important characteristics about the patients seeking treatment through Ro. In this study, we offered a follow-up lab to a sample of more than 1,000 Body members who met the following criteria:
Had completed a baseline metabolic lab test
Received > 10 refills, approximating one year on the program
Were on a semaglutide maintenance dose of 1.7mg, 2.0mg, or 2.4mg
Reside in a state with Quest Diagnostics locations
Subscribed to Ro emails, which was used for recruitment for participation in the study
Of these:
293 patients opted in. Out of those who opted in, 131 completed their labs.
In this study, 70.2% of patients were female, with a mean age of 47.5 (SD = 8.7) and a mean onboarding BMI of 34.3 kg/m2 (SD=5.2).
We analyzed baseline and follow-up lab results by calculating the average absolute and relative changes in metabolic biomarkers. To assess statistical significance, we used paired t-tests and Wilcoxon signed-rank tests, depending on the data distribution. Additionally, we determined the percentage of patients whose biomarker levels improved enough to fall into a better reference range. For example, this included shifts in LDL levels from “high” to “normal” or triglycerides decreasing from “significantly high” to “high”.
Our results:
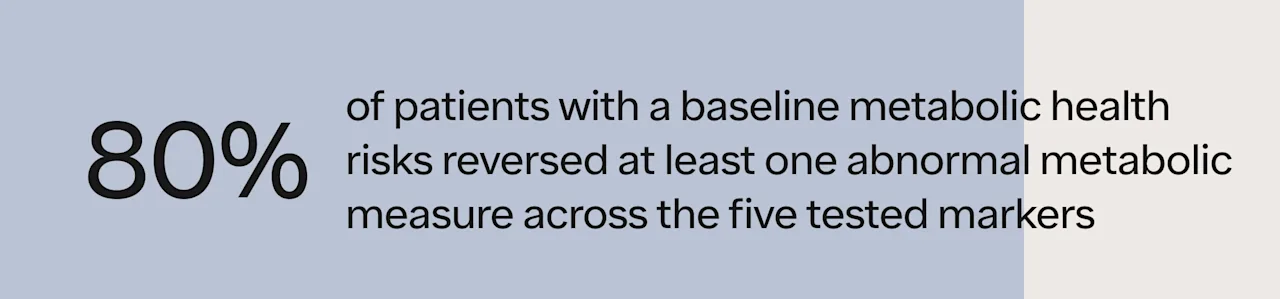
Over the course of a year in the Body membership, patients achieved the following improvements in their metabolic health:
We were also excited to see that patients achieved significant clinical improvements in their HbA1c values. We anticipate publishing and presenting the HbA1C lab results at a leading research conference next year – stay tuned!
Conclusion:
We’re proud of the positive impact that Ro is making in the lives of patients. These findings are profound: improving metabolic health is linked with benefits spanning quality of life, better organ function, and lower risk of developing chronic diseases. These benefits add up to demonstrate why treatment with GLP-1 medications paired with high-quality, personalized obesity care can be life-changing. It is also further evidence that our Body membership – the treatment plans, clinical guidance, side effect and care management, and support for lifestyle changes – is delivering effective care, at scale for patients nationwide.