Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Obesity is one of the most pressing health challenges facing the country today. However, GLP-1s have emerged as a powerful tool for treatment. At the same time, telehealth has become an increasingly common option for patients to access obesity care. Together, these trends are making effective GLP-1 treatments more accessible to those who need them most.
That said, it’s important not to assume that a treatment proven effective in one setting—such as a clinical trial or a brick-and-mortar clinic—will perform the same way in another. Ro’s technology enables us to closely track and measure our patients progress and health outcomes – and we’re committed to doing so.
To ensure Ro patients are getting the highest quality care possible, we conducted a study to measure one-year weight loss outcomes among patients treated with branded semaglutide through our platform. This real-world evidence offers meaningful insights into how treatment with a GLP-1 medication paired with access to high-quality, personalized obesity care via telehealth can help patients achieve their goals.
Our study: sample and methodology:
We analyzed one-year weight loss outcomes for a random sample of 475 Ro Body members. To ensure a valid and reliable analysis, we included only patients who met the following criteria:
Were taking branded semaglutide (Wegovy and/or Ozempic)
Completed only one onboarding visit through our platform: Patients who onboarded multiple times (i.e. cancelled their membership and later returned) may have experienced significant gaps in treatment; limiting the analysis to one onboarding visit ensured relative consistency in treatment.
No history of type 2 diabetes: Patients with a history of Type 2 Diabetes were excluded because research shows significant variability in weight loss outcomes between patients with Type 2 Diabetes and those with obesity or overweight but without diabetes.
Follow-up weights submitted within the time frame of interest: We only included patients who reported follow-up weights between 359 and 369 days from treatment initiation.
Members included in the sample were 66.7% female, had a mean age of 46.3 (SD=9.8), a mean onboarding BMI of 33.3 kg/m2 (SD = 5.0). Percentage weight loss was determined using the formula:
[(onboarding weight - follow up weight within the given time window) / onboarding weight] x 100
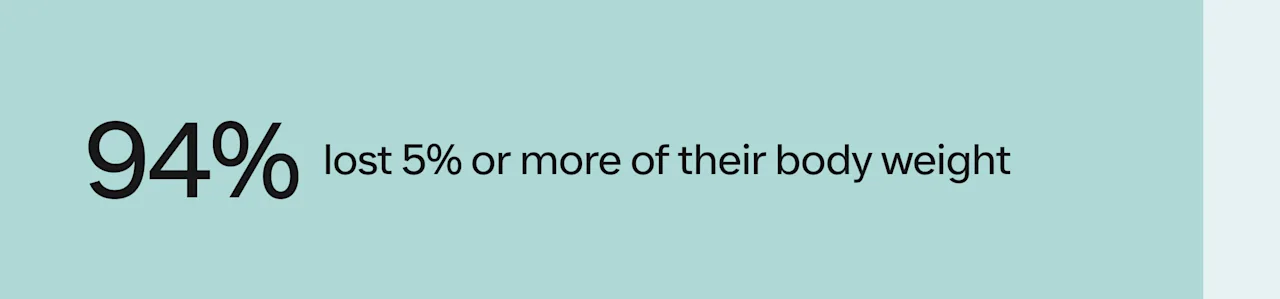
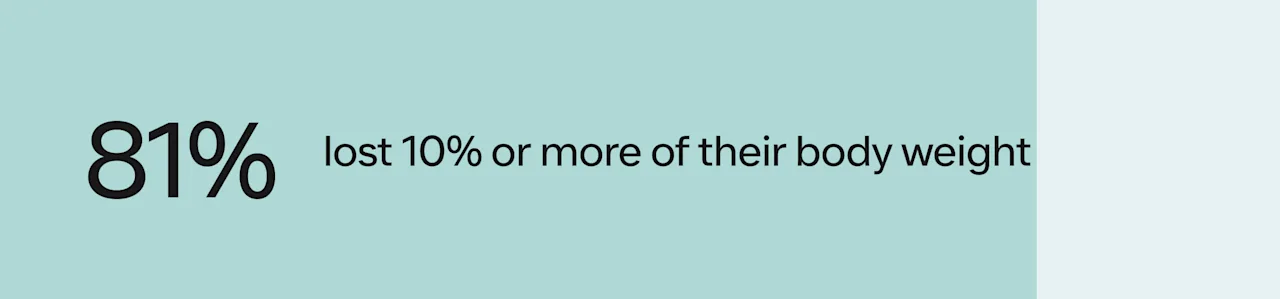
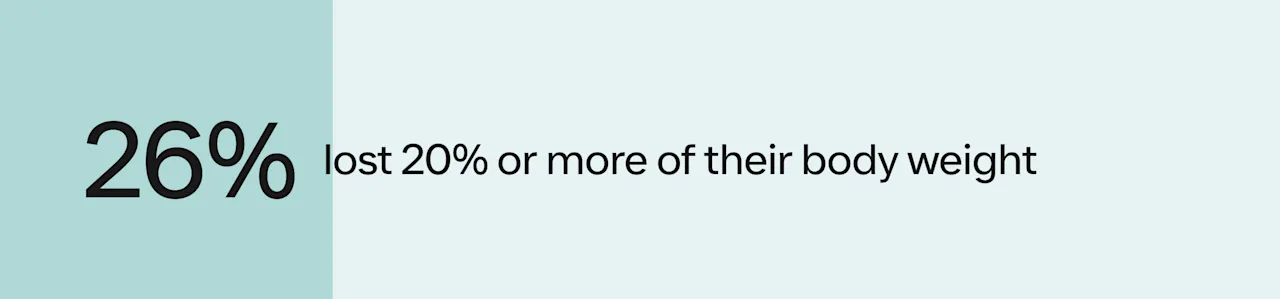
Categorical weight loss data was calculated as the proportion of patients whose percent body weight loss exceeded 5, 10, 15, and 20%. We calculated standard descriptive statistics, including mean, median, and standard deviation to both determine the outcome and assess data quality by checking for anomalies across other summary values.
Patients’ results with Ro Body:
Results show that Ro Body members lost, on average, 15.8% (SD = 6.4) of their body weight over the course of a year of treatment. The majority of patients achieved clinically significant weight loss.

These outcomes are similar to what we would expect based on results from the STEP 1 trial and other published real world evidence.
What our results mean:
From our conversations with patients, we know that motivations for weight loss are deeply personal and diverse. For some, weight loss is a goal in and of itself. For others, it’s about improving health and increasing their quality of or longevity of life, and for others, it’s about reclaiming an identity they feel was lost. Each pound lost represents more than a number on a scale—it signifies progress toward better health and achieving those goals.
By tracking real-world outcomes, we not only celebrate our patients’ successes but also validate the effectiveness of our platform in delivering high-quality care. These results demonstrate that Ro is helping empower patients to take control of their health and achieve life-changing results.