Testosterone Health: Clomiphene Treatment Plan
Hello from Roman! This page contains your treatment plan. Be sure to take your time and read everything below, as well as the package insert included with your medication.
Learning as much as you can about your condition will help you know the questions to ask your doctors and make your relationships that much more productive. It is also essential for you to understand the potential risks and benefits of your treatment.
Roman now is an added asset to your healthcare team. Keep your Ro affiliated doctor informed. If you experience any of the following, log into your member account to contact your Roman provider:
The medication doesn’t work or becomes less effective over time
You experience side effects
Your health status changes or you experience new symptoms
You are prescribed new medications or change how you are taking any of your existing medications
Quick Facts
You have been prescribed clomiphene for the treatment of low testosterone. Follow your healthcare provider’s specific instructions for your individual dosing, since your specific dose and how often you take it may vary. One typical regimen to start is half a tablet (25 mg) every other day.
Potential side effects include mood changes, breast tenderness, low sex drive, and visual abnormalities, including blurry vision, double vision, and rarely blindness. Tell your provider if you experience any of these side effects or other effects that you think may be due to the medication.
As part of your treatment monitoring, you will undergo a series of blood tests to make sure the treatment is working for you (to improve your symptoms and increase your testosterone level).
People who should NOT take clomiphene include those with hypersensitivity or allergy to clomiphene, intracranial (brain) lesions or tumors, pituitary gland tumors, liver disease, uncontrolled thyroid disease, uncontrolled adrenal dysfunction. Tell your provider if you have any of these conditions.
How should clomiphene be taken for low T?
Clomiphene comes in 50 mg oral tablets. It is taken with water once a day or as prescribed. There is a wide range of dosing. The most common dosing regimens are half a tablet (25 mg) every other day or everyday, or one tablet (50 mg) every other day or everyday.
What if I miss a dose?
If you accidentally miss a dose, take it when you remember. However, if your next dose is supposed to be within a couple of hours, skip the missed dose and resume your normal schedule. Do not take a double dose. Let your Ro-affiliated provider know if you miss a dose.
What if I take more than I am prescribed?
The amount of clomiphene that is toxic for humans to ingest is currently unknown. On tests done on mice, the amount of clomiphene found to kill half of the test subjects was 1,700 mg/kg. And on tests done on rats, the amount of clomiphene found to kill half of the test subjects was 5,750 mg/kg. Both of these doses are hundreds to thousands of times higher than the daily dose in humans (and also much higher than if you were to take an extra daily dose by accident).
However, taking more than you are prescribed may cause symptoms. These include nausea, vomiting, flushing, visual changes, and pelvic or abdominal pain. If you are experiencing any of these symptoms (or are not experiencing these symptoms but believe you may have taken too much anyway), contact your healthcare provider and poison control.
How does clomiphene work for low T?
Clomiphene is a type of medication known as a Selective Estrogen Receptor Modulator (SERM). It tells the pituitary gland, which is like a hormone command center in the brain, to release more leutinizing hormone (LH), which, in turn, tells the testes to make more testosterone. SERMs are drugs that bind to the estrogen receptors throughout the body. Somewhat paradoxically, in some tissues clomiphene blocks estrogen from having its normal effects, but in other tissues clomiphene acts just like estrogen and has the same effects.
How do I know if Clomid®️ is working? How long will it take?
Clomid®️ (clomiphene citrate) is successful at raising testosterone in most men, but not all. For men with primary testicular dysfunction, Clomid may not be able to raise testosterone levels because the testes may not be capable of manufacturing testosterone in response to stimulation from the pituitary gland (and high LH levels). Helping your body produce the testosterone it needs without the need for foreign testosterone is appealing but for some men it just isn’t possible.
However, for men in whom Clomid does raise testosterone levels, there are two possible outcomes:
Most men will get substantial symptom relief. Depending on your initial symptoms, this may mean increased sex drive, better energy levels, improved mood, and more.
Some men may experience an increase in testosterone levels but may still not have adequate symptom relief. The reasons for this are not always fully understood.
It’s important to understand that it may take 2–3 months of treatment to see an improvement in symptoms. It’s important to give it time to see if symptoms will be alleviated. Let your provider know if you’re in the smaller group of men not experiencing symptom relief. Sometimes, it merely means you need a higher dose.
What if clomiphene doesn’t work for me?
As stated above, clomiphene is not always successful at raising testosterone levels substantially, and sometimes it does raise testosterone levels but symptoms are not adequately controlled. One possibility that should be investigated is that the symptoms are not completely due to low T, or even not all due to low T. Symptoms of low T overlap with many other causes, including but not limited to underactive thyroid, anemia, depression, and sleep apnea.
Another possibility is that the symptoms are caused by low T and will respond to treatment with testosterone even if they do not respond to clomiphene. The reasons for this aren’t fully understood either.
Your Ro-affiliated provider will use lab testing and periodic follow up visits (which will ask about symptoms and side effects) to confirm that clomiphene is working for you. If clomiphene isn’t helping your low T, they will help you figure out the best next steps. If clomiphene does not work for you, you may need to see a healthcare provider who specializes in male hormones (urologist or endocrinologist) for further evaluation and treatment.
What are the benefits and drawbacks of clomiphene?
Producing more testosterone by taking clomiphene has several benefits when compared to raising testosterone levels by adding foreign testosterone, whether by injection, cream or pill. First, Clomiphene will not shrink the testes or cause sperm counts to plummet. This is because clomiphene does not interfere with the signaling of the pituitary gland to the testes. When men use foreign testosterone, in any form, the pituitary gland gets the signal that there are high levels of testosterone and it stops telling the testes to perform their functions—like making sperm. This interferes with sperm production and clearly is not good for men who want to maintain fertility.
Many men also like the idea of taking a pill instead of shots or creams (creams that can be transferred to females or children unintentionally). Some men simply prefer the concept of having their testes produce their needed testosterone instead of using testosterone from a foreign source. The advantages of low T treatment with clomiphene include:
Clomiphene is a good option for men who want to maintain their fertility
It is easy to use (taken as a tablet)
It may have fewer side effects than testosterone
It is a relatively affordable generic drug
Clomiphene also has a few disadvantages compared to treatment with testosterone.
It is less likely to work in men with primary hypogonadism (low T due to malfunctioning testes), which is why men are first carefully selected before starting Clomiphene therapy
It is not effective in some men who do respond to testosterone
It has variable effects on the estrogen receptor, which causes certain side effects in some men, like decreased sex drive
It is an off-label medication and does not have an FDA indication for the treatment of low T
What additional testing do I need?
Before starting treatment for low testosterone, patients undergo blood testing to determine their testosterone levels and to search for potential causes of low T. Follow-up testosterone levels and other blood work are monitored while being treated for low T.
As part of the Testosterone Health Program, you may have check-ins including blood tests on a schedule similar to the below. Note that exact timing and specific blood tests may vary slightly based on logistics of scheduling with the lab and your individual case.
In about 8–12 weeks, you will receive another Kit at-home test in the mail. It is important that you return it as soon as you are able. With that new test result and your follow-up online visit reporting about how you have improved (or not), your provider can renew your medication, increase your dose, offer other options for you to consider, or recommend you see a specialist in person. Keep notes and write down your questions. That always helps to make the consultation more meaningful.
If all is going well, you will have an informal check in at about the 6 month mark and, if there are no problems and the medication is working as expected, you will simply receive another Kit at-home test at the 9 month mark. Again, return the test as soon as possible so your doctor and you can confer at the 10 month mark and evaluate your treatment plan. Once again, keep notes and be sure all your questions are answered when you connect with the team.
This pattern will repeat one more time 6 months later but once you are on a working treatment plan, only annual evaluations will be needed.
At each check-in, you will complete an online visit asking about how the medication is working in terms of relieving your symptoms and if there are any side effects. You will have also completed the Kit at-home test, which may include:
Testosterone level. Your testosterone level will be checked at each check-in to make sure it is in the healthy range. This result, in combination with whether your symptoms are improving (and by how much), are the major factors that determine whether the treatment is working.
What if my testosterone levels don’t go up? Depending on your individual case, your provider may increase your dose of clomiphene or how often you take your current dose.
What if my testosterone levels are too high? Depending on your individual case, your provider may lower your dose of clomiphene or how often you take your current dose.
Prostate-specific antigen (PSA). Increasing your testosterone levels can also increase your PSA, a substance made by the prostate gland that circulates in the blood. It’s important to monitor this level to make sure it doesn’t get abnormally high. The most important cause of an elevated PSA to know about is prostate cancer. Other common causes of elevated PSA include older age, prostate inflammation, and enlarged prostate (benign prostatic hyperplasia, or BPH). Tell your Ro-affiliated provider if you have ever had any prostate problems including BPH or prostate cancer. Remember, Roman is just one member in your healthcare team. There is no substitute for discussing prostate cancer screening with your primary care provider to decide what screening approach is best for you.
What if my PSA goes up? Depending on your individual case and how high your PSA gets, your provider may lower your dose of clomiphene or how often you take your current dose, or advise that you stop treatment, temporarily or permanently.
What if my PSA goes down? There are no negative effects of a low PSA level.
Hemoglobin and hematocrit (H&H). These numbers indicate your blood count, specifically the concentration of red blood cells. Low testosterone can lead to having too few red blood cells and by increasing your testosterone levels it is possible to make too many red blood cells. This is what your hemoglobin and hematocrit measures. The problem with too many red blood cells is that blood becomes thicker and more likely to cause dangerous clots. Tell your Ro-affiliated provider if you have ever had any blood clots, including stroke, heart attack, deep venous thrombosis or pulmonary embolism.
What if my H&H goes up? Depending on your individual case and how high your H&H gets, your provider may lower your dose of clomiphene or how often you take your current dose, or advise that you stop treatment, temporarily or permanently.
What if my H&H goes down? This would not be expected from treatment with clomiphene, but depending on your individual case and how low your H&H is, your provider may repeat the blood test or recommend that you be referred to an in-person provider who can perform a full diagnostic workup of anemia (abnormally low H&H).
Estradiol. Estradiol is the main form of estrogen in the body (see below under “How is testosterone made in the male body?” for more information on estradiol and why biological males have estrogen). Increasing your testosterone levels can also increase your levels of estradiol.
What if my estradiol goes up? Depending on your individual case and how high your estradiol gets, your provider may lower your dose of clomiphene or how often you take your current dose, or advise that you stop treatment, temporarily or permanently. Another option may be to start a medication that lowers estradiol levels (anastrozole).
What if my estradiol goes down? This is not expected from treatment with clomiphene.
Hemoglobin A1c (HgbA1c). HgbA1c is composed of the hemoglobin protein with a sugar attached to it. It is most frequently thought of as a measure of blood sugar control in people living with diabetes. In people with diabetes, the HbA1c is often high when the diabetes is not controlled well as it is a measure of a person's average blood glucose level over the prior 3 months. Increasing your testosterone levels may lower the HbA1c, which is a good thing in most cases. It is a helpful measure to monitor, especially in someone who has diabetes. Tell your provider if you have or have ever had diabetes, prediabetes, or an abnormal HbA1c.
What if my HgbA1c goes up? This would not be expected from treatment with clomiphene, but depending on your individual case and how high your HgbA1c gets, your provider may repeat the blood test or recommend that you be referred to an in-person provider who can perform a full diagnostic workup of elevated blood sugar.
What if my HgbA1c goes down? There is no known detrimental effect of decreasing HgbA1C.
It is important to remember that your online visit with Roman for evaluating for low testosterone does not replace routine in-person care. There may also be recommended screening tests for you depending on your age, sex, and family history that require in-person evaluation.
You should still plan on seeing your in-person healthcare provider as you normally would, especially if treatment is not working for you. In that case, your in-person provider may be able to perform additional tests to evaluate any potential underlying causes of your condition.
Warnings
The full list of contraindications, precautions, and drug interactions is at the bottom of this page. However, it is important to highlight a few things here:
There is a risk of visual disturbance (like blind spots, blurry spots, flashes appearing, and rarely blindness), which may make activities such as driving a car or operating machinery more hazardous than usual, particularly under conditions of variable lighting. If you have any visual symptoms, you should discontinue treatment, tell your healthcare provider immediately, and have a complete eye evaluation as soon as possible
There have been cases of hypertriglyceridemia (high triglyceride levels in the blood) reported. Your healthcare provider may want to test your triglycerides before starting treatment and/or periodically during treatment.
Cases of pancreatitis (pancreas inflammation) have been reported. Stop clomiphene and seek treatment immediately if you develop nausea, vomiting, or severe abdominal pain.
If any changes to your health or new symptoms you think may be related to taking clomiphene, stop taking it immediately and notify your prescribing doctor or nurse practitioner
What is low testosterone (low T)?
Before explaining what low testosterone (low T) is, let’s go over what testosterone is. Testosterone is a sex steroid hormone found in both men and women. Let’s break down what that means.
Hormones are molecules made in glands found throughout the body. Hormones can control everything from your metabolism (thyroid hormones) to your sexual and reproductive functions (hormones made in the testes and ovaries).
Steroid hormones are made from cholesterol.
Sex hormones affect sexual development, sexual function, and reproduction.
Although testosterone is usually thought of as a male hormone, it is important for both males and females for normal sexual functioning. In males, testosterone levels normally peak during late adolescence and start to decline around age 30. As it declines slowly over time, levels can drop low enough to cause the symptoms of low T.
Low T is diagnosed when testosterone falls below a certain value and a man has symptoms of low T. In the United States, testosterone is measured in nanograms per deciliter (ng/dL) and normal levels are generally considered to be 300–1,000 ng/dL. Men with symptoms typical of low T of testosterone below 350 ng/dL are considered for treatment on the Ro platform.
How is testosterone made in the male body?
In biologically male bodies, testosterone is primarily made in the testes (a.k.a. testicles), which also produce sperm. These two jobs belong to two sets of specialized cells:
Sertoli cells are responsible for sperm development in special tubes called seminiferous tubules
Leydig cells are responsible for producing testosterone
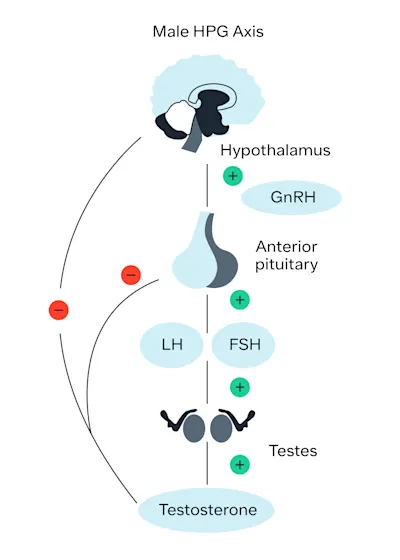
Testosterone production is carefully coordinated between a part of the brain called the hypothalamus, another part of the brain called the pituitary gland, and the testes. Normally, the system works as follows:
The hypothalamus releases a hormone called gonadotropin-releasing hormone (GnRH).
GnRH signals the pituitary gland to release two hormones, luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
LH signals the Leydig cells in the testes to produce testosterone; FSH signals the Sertoli cells, also in the testes, to start sperm production.
This whole process is a tightly controlled feedback loop. When testosterone and sperm production are high, the signals to make them (LH and FSH) go down. The opposite is also true. When testosterone levels and sperm quantity decrease, LH and FSH increase.
If any part of this system doesn’t work properly, it can cause testosterone levels to decrease to levels below normal (“low T”). When low T occurs because the testes themselves do not work properly and therefore cannot make testosterone (and/or sperm), we call it primary hypogonadism. When low T occurs because the pituitary gland does not work properly and does not signal the testes to make testosterone (and/or sperm), we call this secondary hypogonadism. This distinction is important because treatment can differ for primary and secondary hypogonadism.
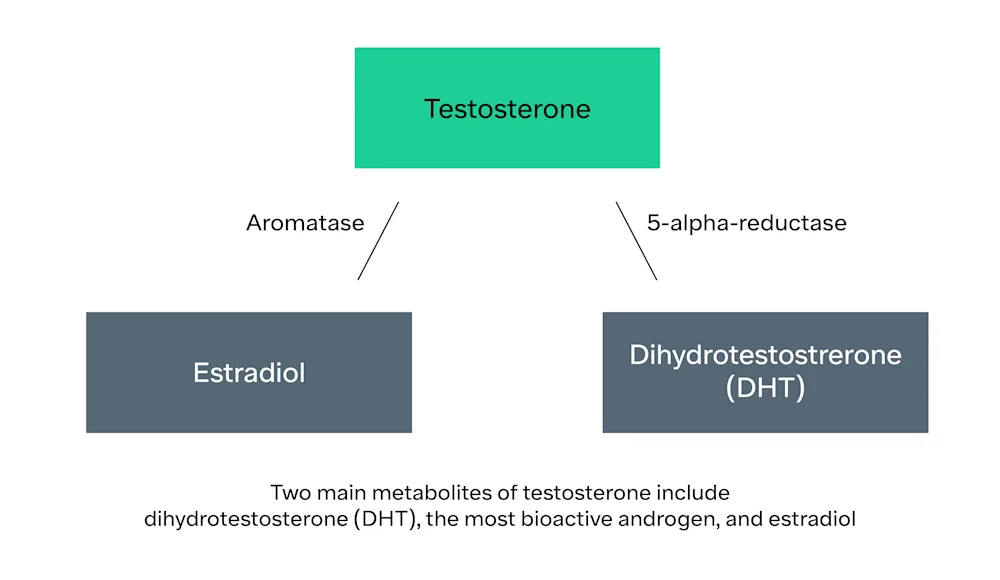
Testosterone can be converted into two other hormones by two different enzymes:
It can be converted into dihydrotestosterone (DHT) by the enzyme 5-alpha reductase
It can be converted into estradiol (the most common form of estrogen) by the enzyme, aromatase. This is important because estradiol levels can go up when testosterone levels go up, causing symptoms (side effects) of high estrogen like breast tenderness.
What causes low testosterone?
As stated above, low T can be caused by primary or secondary hypogonadism, where primary hypogonadism means the testes aren’t responding to the signals sent by the pituitary gland and secondary hypogonadism means the pituitary gland isn’t signaling the testes properly. Each one has its own causes and sometimes a person can have a mixture of primary and secondary hypogonadism.
Causes of primary hypogonadism (Low T, High LH)
Genetic disorders (e.g., Klinefelter syndrome, enzyme mutations)
Infections (e.g., mumps, HIV)
Radiation
Chemotherapy
Drugs (e.g., antifungals, glucocorticoids)
Trauma
Liver cirrhosis
Chronic kidney disease
Prior anabolic steroid use/abuse
Autoimmune
Idiopathic (occurs on its own without a known cause)
Causes of secondary hypogonadism (Low T, Low/Normal LH)
Genetic disorders (e.g., pituitary hormone mutations, leptin mutations, Prader-Willi syndrome)
Drugs (e.g., anabolic steroids, opioids, glucocorticoids, marijuana)
Several chronic and systemic illnesses (e.g., cirrhosis, chronic kidney disease, chronic lung disease, acquired immunodeficiency syndrome (AIDS))
Anorexia nervosa
Diabetes mellitus
Obesity
Sleep apnea
Hypothalamic and pituitary gland tumors
Infiltrative disease (e.g., sarcoidosis, hemochromatosis)
Head trauma
Aging (sometimes called androgen deficiency in the aging male or ADAM)
Idiopathic (occurs on its own without a known cause)
What are the symptoms of low T?
The most common reasons people seek out medical care are symptoms involving sexual function, such as low sex drive, erectile dysfunction (ED), and infertility. However, since testosterone has effects on so many body systems, many symptoms are possible. These include: Mood changes (e.g., depression, irritability)
Decreased sense of well-being
Fatigue
Decreased cognitive function (e.g., poor concentration, poor memory)
Decreased body and beard hair
Decreased muscle mass and strength
Growth of breast tissue in men
Decreased bone density
Weight gain
Problems responding to the hormone, insulin (insulin resistance)
Infertility
Decreased sex drive
Difficulty getting or maintaining an erection
Orgasm dysfunction (e.g., delayed orgasm, inability to orgasm)
Penile insensitivity
What else should I know about low T and low T treatment?
While there are many benefits of treating low T, some things are still under investigation.
Low T is a risk factor for cardiovascular disease, but we still don’t know if treating low T increases or decreases the risk for heart attack, stroke, and dying from cardiovascular disease.
Treatment of low T may result in improvements in erectile function, low sex drive, anemia, bone mineral density, lean body mass, and/or depressive symptoms.
We still do not know whether treatment of low T improves cognitive function, measures of diabetes, energy, fatigue, lipid profiles, and quality of life measures.
There is currently no evidence linking testosterone therapy to the development of prostate cancer.
There is no definitive evidence linking testosterone therapy to a higher incidence of blood clots.
Are there any alternative treatments or other things I can do for low T?
Treatments for low T include treating the underlying causes of low T, lifestyle modifications, and drugs that directly increase testosterone levels.
Treating the underlying cause of a medical problem is always the preferred choice whenever possible. For example, certain medications can cause low T and they may be able to be stopped or substituted with a different treatment. For example, opioids and glucocorticoids could potentially be substituted with other medications for pain and steroid replacement, respectively.
Treating obesity and sleep apnea may raise testosterone levels somewhat. Weight loss, in particular, has been shown to increase testosterone levels and improve sexual function when the weight loss is substantial. Lifestyle modification, including exercise and calorie reduction, are the foundation of weight loss, but many people can also benefit from medication or surgery. Exercise is recommended in men with low T regardless of other weight loss methods used. This is where medical/surgical treatments and lifestyle changes can work synergistically. A person may use medical therapy or surgery together with a lifestyle modification program to address weight loss or sleep apnea.
That’s why it is a good idea to check if you need treatment for low testosterone once you have made some progress. Often, patients elevate their testosterone levels with medication and their energy improves. They suddenly have the desire and ability to exercise. They lose weight and start to build muscle mass. They sleep better, eat better, and start to control their glucose better. Ultimately, they start making more testosterone without the need for medication.
And that’s the goal!
Drugs that directly increase testosterone levels come in three different types. The first is testosterone itself, which works by giving the body additional testosterone. This is also known as exogenous T, or testosterone replacement therapy (TRT). TRT comes in many different forms, including injections, creams, gels, patches, oral formulations, and pellets that are placed under the skin and release testosterone slowly over time. Injections and topical forms are the most popular ways of using TRT.
The second type of drug that can increase testosterone levels are drugs that stimulate the testes to produce testosterone. There are two main drugs that do this. The first is clomiphene and the second is a drug called human chorionic gonadotropin, or hCG. hCG is often called the “pregnancy hormone,” as levels go up during pregnancy. In fact, pregnancy tests look for high levels of hCG. hCG has a very similar chemical structure to LH and can be used in men to stimulate the testes to produce more testosterone. Like clomiphene, it has the benefit of not interfering with fertility. It also has the benefit of not interacting with estrogen receptors and potentially having effects other than raising testosterone. Some disadvantages of hCG are that it is expensive, it must be supplied by a compounding pharmacy, it requires refrigeration, and it needs to be injected several times per week.
The third type of drug that increases testosterone levels are drugs that prevent the conversion of testosterone to other hormones. 5-alpha reductase inhibitors, like finasteride and dutasteride, prevent the conversion of testosterone to DHT. However, this is not a good way to treat low T because DHT has some important actions similar to testosterone. In fact, lowering DHT levels may make symptoms of low T worse. Aromatase inhibitors, like anastrozole, are drugs that decrease the conversion of testosterone to estradiol, the main type of estrogen in the body. They may be used alone to increase testosterone levels in men with low T and high estrogen levels. However, more commonly, they are used in men receiving other treatments for low T to prevent the excess conversion of testosterone to estradiol.
Natural approaches to optimizing testosterone levels include getting enough sleep and exercise, eating adequate amounts of healthy fats and weight loss in those with overweight or obese. Certain supplements, like ashwagandha, may be somewhat helpful in increasing testosterone levels as well.
What is off-label prescribing?
The FDA requires that drugs go through a clinical testing process to establish that they’re safe and effective to treat a particular condition. Healthcare providers may prescribe a drug for an unapproved use if they judge that it is medically appropriate for their patient. This type of prescribing is called “off-label” prescribing. Off-label prescribing practices are sometimes validated by clinical experience and research and may be a widely recognized clinical practice. Healthcare providers have the discretion to prescribe drugs off-label based on a patient’s unique medical history, symptoms, and preferences. Talk to your Ro-affiliated provider if you have any concerns or questions about using clomiphene or anastrozole off-label. You can always message your healthcare provider through your Ro account.
Important Medication Information
Adapted from the Prescribing Information for clomiphene except where otherwise noted.
Read this information before you start taking clomiphene and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or treatment. If you have any questions about clomiphene, ask your doctor, nurse practitioner, or pharmacist.
What is the most important information I should know about clomiphene?
Clomiphene is a selective estrogen receptor modulator (SERM) most commonly used to treat infertility in women. Clomiphene can also be used off-label as an alternative therapy to testosterone replacement for raising testosterone levels in men.
Clomiphene has been shown to increase testosterone levels to a degree similar to that of testosterone gel (Taylor, 2010 and Mulhall, 2018)., There are no adequate or well-controlled studies that demonstrate the effectiveness of clomiphene citrate in the treatment of male infertility.
Testicular tumors and gynecomastia (enlarged breasts) have been reported in males using clomiphene. The cause and effect relationship between testicular tumors and clomiphene is not currently known.
Who should not take clomiphene?
People who are allergic to clomiphene or any of its components should not take clomiphene.
People with thyroid or adrenal gland conditions that are uncontrolled, or with tumors of the pituitary gland (or other brain tumors) should not take clomiphene.
People who are taking bexarotene (brand name Targretin), a drug used for cutaneous T-cell lymphoma, may have a higher risk of developing pancreatitis when taking both bexarotene and clomiphene.
While sometimes used to treat infertility in women, clomiphene should not be used by pregnant women. It should also not be used in women taking ospemifene (brand name Osphena), a drug used for painful sex in women due to menopause, as it may increase the risk of side effects.
Before you take clomiphene, tell your Ro provider if you have any of the following conditions:
Liver disease
Uncontrolled thyroid disease
Uncontrolled adrenal disease
Pituitary tumor
Other brain tumor
High triglyceride levels
What are the possible side effects of clomiphene?
Clomiphene can cause occasional blurry vision or other visual symptoms such as spots or flashes. Other side effects include enlarged or tender breasts, upset stomach, bloating, flushing, and headache. Mood changes and lower libido have also been reported.
There have been rare cases of hypertriglyceridemia (high triglyceride levels in the blood) reported. Your healthcare provider may want to test your triglycerides before starting treatment and/or periodically during treatment.
Cases of pancreatitis (pancreas inflammation) have been reported. Stop clomiphene and seek treatment immediately if you develop nausea, vomiting, or severe abdominal pain.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
This is not a complete list of reported side effects; see the Prescribing Information for more.