Plenity Treatment Plan
Your physician has reviewed your medical information and has prescribed medication for weight management. This medication is specifically intended to help you manage your weight and is NOT intended to treat any other medical conditions that you may have.
Quick facts
What is Plenity?
Plenity is a capsule containing a super absorbent hydrogel that absorbs up to 100 times its weight in water. It is FDA-cleared as an additive treatment for weight management in people with a Body Mass Index (BMI) of 25–40 to be used with a reduced calorie diet and exercise. Plenity is taken with 16 oz (2 cups) of water 20–30 minutes before lunch and dinner. The hydrated Plenity takes up room in the stomach promoting a feeling of fullness. Plenity does not get absorbed and leaves the body unchanged in a bowel movement. This decreases the risk of side effects compared to medications that get absorbed systemically. Weight loss with Plenity takes several weeks although the effects of feeling fuller with meals may be obvious from the beginning of use. A weight loss of at least 3% body weight after 8 weeks of use is highly predictive of success, with about 85% of people losing at least 5% of their body weight after 24 weeks. You are also more likely to see results by taking Plenity as consistently as possible (that is, without missing any doses), exactly as directed below. Studies have also demonstrated that people who consistently weigh themselves regularly are more likely to keep off the weight they lose over the long term (5-10 years and beyond). That is, if you are weighing yourself every day, you should continue to weigh yourself every day. If you are weighing yourself every week, keep weighing yourself every week.
How to use Plenity
Take three capsules (2.25 grams total) orally with 16 oz (2 cups) of water 20–30 minutes before lunch and again before dinner. Plenity use should be combined with a reduced calorie diet (at least 300 calories less than maintenance needs) and regular exercise (at least 30 minutes per day of moderate intensity exercise, like brisk walking).
Who should not use Plenity?
Plenity should not be used in the following groups:
People who have had weight loss surgical procedures or gastric balloons
People with a BMI of less than 25 or more than 40
Pregnant and breastfeeding women
People with allergies to ingredients in Plenity, including cellulose, citric acid, sodium stearyl fumarate, gelatin, or titanium dioxide
People with esophageal anatomic anomalies (e.g., webs, diverticuli, rings)
People with suspected digestive tract strictures (narrowing), such as patients with Crohn’s disease
People with inflammatory bowel disease
People with complications from prior gastrointestinal surgery that could affect how well the digestive tract functions and how quickly food moves through the digestive tract
People who have difficulty swallowing pills
People with eating disorders, like anorexia nervosa and bulimia nervosa
What are the possible adverse effects of Plenity?
The most common adverse events seen with Plenity in a large clinical trial were GI (digestive system) adverse effects
Diarrhea
Decreased bowel movements
Constipation
Abdominal distention
Flatulence (gas)
Nausea
The following occurred at the same rate as the placebo group.
Infections
Nasopharyngitis
Influenza
Upper respiratory infections
Back pain
Joint pain (arthralgia)
Headache
For more information on Plenity adverse events, see the Plenity Instructions for Use.
When should I contact my Ro-affiliated physician?
Contact your Ro-affiliated physician, and all of your healthcare providers, if you experience any new symptoms after beginning Plenity. If you have any serious signs or symptoms, like, but not limited to, blood in your stool, severe diarrhea, fainting, or severe abdominal pain, please seek out emergency medical treatment.
Introduction
Congratulations on starting your journey! We understand the challenge that weight loss poses, especially for those who have already tried to lose weight unsuccessfully or have lost weight only to regain it. Lifestyle modification is the backbone of weight loss therapy—there is no substitute for a scientifically informed weight loss plan that includes healthy eating and exercise. Plenity can help you make the changes you need to lose weight and keep it off—even if you’ve had difficulty with doing so in the past. Plenity is a new, safe, and effective weight management tool when combined with exercise and a reduced calorie diet.
A great deal of information and many tools (e.g., behavioral tips, the importance of exercise) are provided below to help you with your weight loss journey. You know yourself well and will be able to embrace all the small techniques that can help you reach your goal. The key is to learn as much as you can in order to make informed decisions with your healthcare providers.
Carefully review the personalized treatment plan your doctor made for you, as well as all of the materials provided. Do not hesitate to reach out if you have any questions.
Your treatment plan
Your doctor has reviewed your medical information and has prescribed Plenity 2.25 g twice daily as an addition to diet and exercise. Plenity has been scientifically proven to help approximately 60% of people achieve clinically significant weight loss when combined with lifestyle changes. Weight loss can be challenging, and Plenity is a useful tool with significant benefits over other weight loss treatments. One of the main benefits of Plenity is that it does not get absorbed into the body, which decreases the risk of side effects outside of the digestive system. This treatment plan not only provides information about Plenity but includes many scientifically supported tips to help you with your weight loss goals.
What is Plenity and how does it work?
Plenity is a super absorbent hydrogel. Hydrogels are gels that act like sponges, absorbing large amounts of water. Plenity absorbs up to 100 times its weight in water. It comes in a capsule that contains 0.75 grams. Three capsules (2.25 grams total) are taken orally with 16 oz (2 cups) of water 20–30 minutes before lunch and again before dinner.
Plenity is made of two all-natural ingredients: citric acid and cellulose. Once the capsules are swallowed, the outer part of the capsules disintegrate in the stomach, releasing the numerous Plenity particles. These particles interact with the 16 oz of water you drank, absorbing it. In fact, each Plenity particle can absorb up to 100 times its weight in water, and this makes them grow. Once the particles are fully hydrated, they take up about ¼ of the average stomach volume.
The hydrated Plenity mixes with food you’ve eaten creating a sense of fullness. Plenity then moves on to the intestines where, unlike food, it does not get absorbed. Instead, Plenity simply passes through the digestive system in its hydrated form. Once it reaches the colon (the large intestine), the body reabsorbs the water from the Plenity particles. The particles shrink back down, and then leave the body during a bowel movement. The fact that Plenity does not get absorbed accounts for its high tolerability and favorable side effect profile.
How should I use Plenity?
There are a few important things to keep in mind when using Plenity.
Take 3 (three) capsules of Plenity twice daily, 20–30 minutes before a meal.
Plenity should be used 20–30 minutes before lunch and 20–30 minutes before dinner.
It’s important to take Plenity with 2 cups (16 oz) of water. This “activates” the Plenity. The water will be absorbed by the Plenity, which will then fill about ¼ the volume of the stomach.
Plenity must be combined with a decrease in calories. In the Plenity clinical trial (see below), participants were told to decrease their calories to 300 per day less than their calculated maintenance needs. It’s important to understand that all weight loss interventions work by decreasing caloric intake. Plenity can help make this more achievable, but it is still possible to eat too many calories while taking Plenity.
Exercise is an important part of any weight loss program and becomes especially important when it comes to weight loss maintenance. In the GLOW study, participants were instructed to engage in 30 minutes of moderate-intensity exercise per day (such as brisk walking). Besides being important for weight loss, exercise is one of the most important behaviors that can help you live a longer, healthier life. When you’re taking Plenity, it is recommended that you exercise for at least 30 minutes at a moderate-intensity daily.
What are Plenity’s side effects?
One of the features that makes Plenity so appealing as a weight-loss tool is its favorable side effect profile. In the GLOW study, the Plenity group had the same rate and type of side effects as the group taking placebo pills and water. The rate of dropout due to side effects was also similar in the Plenity and placebo groups. While no individual side effect was more likely to occur in the Plenity group than the placebo group, when added all together, Plenity had more total gastrointestinal (GI) side effects than the placebo group. However, each individual GI side effect was similar between groups. Also, over 95% of adverse events were considered mild or moderate. Below you’ll find the most common adverse events seen with Plenity in the GLOW study.
GI (gastrointestinal) side effects, such as:
Diarrhea
Decreased bowel movements
Constipation
Abdominal distention
Flatulence (gas)
Nausea
The following occurred at the same rate as the placebo group:
Infections
Nasopharyngitis
Influenza
Upper respiratory infections
Back pain
Joint pain (arthralgia)
Headache
For more information on Plenity adverse events, see the Plenity Instructions for Use.
Who should not take Plenity?
Plenity should not be used in the following groups:
People who have had weight loss surgical procedures or gastric balloons
People with a BMI of less than 25
Pregnant and breastfeeding women
People with allergies to ingredients in Plenity, including cellulose, citric acid, sodium stearyl fumarate, gelatin, titanium dioxide
People with esophageal anatomic anomalies (e.g., webs, diverticuli, rings)
People with suspected digestive strictures (narrowing), such as patients with Crohn’s disease
People with inflammatory bowel disease
People with complications from prior gastrointestinal surgery that could affect how well the digestive tract functions and how quickly food moves through the digestive tract
People who have difficulty swallowing pills
People with eating disorders, like anorexia nervosa and bulimia nervosa
Additionally, people who follow a vegan diet may not want to take Plenity because the capsule includes gelatin, which is derived from animals.
Talk to your doctor before using Plenity if you have active gastrointestinal conditions, such as severe gastro-esophageal reflux disease (GERD), unhealed ulcers, or severe heartburn, as Plenity may not be for you.
What drugs does Plenity interact with?
Only one study has been completed and it investigated the interaction of Plenity with metformin. The study showed that metformin absorption is the same when taken with food as it is when taken with food and Plenity together. However, Plenity reduces metformin absorption when taken without food. Since Plenity should not be used without food (it is meant to be taken 20–30 minutes before a meal), this interaction should never occur.
It is not known if Plenity interacts with other medications. Therefore, all medications that are taken once daily should be taken in the morning (fasting or with breakfast) or at bedtime, as prescribed by your physician.
If you take medication with meals or close to meals, the medication should be taken after the meal has started.
Discuss all medications with your physician prior to beginning Plenity. If you are already taking Plenity, discuss it with all of your doctors before taking any new medications. If you are diabetic and taking medications to lower your blood sugar, discuss your use of Plenity with your doctor as you may need to adjust your medications.
Do I need to undergo any additional testing?
Since overweight and obesity are risk factors for a number of other health issues, certain lab tests are often recommended for those undergoing treatment for excess weight. These tests can be ordered by your primary healthcare provider and include:
Lipid panel: this tests your cholesterol and triglyceride levels
Fasting blood sugar (also called fasting glucose): this is the concentration of sugar in your blood after not eating for at least 8 hours.
Hemoglobin A1C (HbA1C): this test tells us about your average blood sugar over the previous 2–3 months.
Liver enzymes, including alanine aminotransferase (ALT) and aspartate aminotransferase (AST): these are enzymes required for metabolism that are made by the liver cells. Elevated levels can mean there is something wrong with the liver, although they are not specific for a certain disease.
Thyroid stimulating hormone (TSH): this test assesses thyroid function.
Certain special tests may be warranted in specific cases, including genetic tests for rare genetic causes of obesity and an assessment of adrenal function for those with specific signs and symptoms.
Tips on weight loss and weight maintenance
What’s the best way to cut calories?
The short answer is that there is no one best diet for everyone and different diets work for different people. All weight-loss interventions work by creating an energy deficit, which means that more calories are burned than consumed. This is true for diets, exercise, weight-loss drugs, bariatric surgery, and any combination of these methods. Other than bariatric surgery, dietary modification is the most successful means of losing weight.
But which diet is best? Low fat or low carb? What about keto, Atkins, Zone, Ornish, and intermittent fasting (IF)? Research shows that adherence to an eating plan is more important for weight loss success than the specific eating plan.
For example, one study published in the New England Journal of Medicine (NEJM) assigned people to four different groups with different percentages of calories coming from protein, fat, and carbohydrates.
The study showed that all diets produced similar weight loss after 6 months and that adherence to the diets and attendance at the prescribed group sessions were good predictors of success. All groups had some weight regain on average after 12 months, but 23% of the participants continued to lose weight between 6 months and 2 years. The study was criticized because participants did not achieve the nutrient targets and there was substantial overlap between groups, meaning their diets weren’t that different. However, this may illustrate how difficult it is to stick to more extreme macronutrient (macronutrients are carbs, fat, and protein) targets.
An especially well-done study by Gardner et al published in the Journal of the American Medical Association (JAMA) compared a low carbohydrate diet with a low-fat diet. In this study, the low carb and low fat groups did end up with substantially different percentages of their calories coming from carbs and fat. The low fat ate a diet with 48% carbohydrates, 29% fat, and 21% protein. The low carb group ate a diet with 30% carbohydrates, 45% fat, and 23% protein. Both groups lost the same amount of weight on average.
One of the more interesting findings in studies that compare interventions for weight loss is the substantial differences between individuals. This is true whether the interventions are dietary, surgical, or pharmacologic (weight loss drugs). For example: although both groups averaged the same amount of weight loss in the Gardner study, there was a large range of responses in both groups with some people losing over 30 kg (66 lbs) and others gaining over 10 kg (22 lbs) at the extremes of weight loss and gain.
These numbers represent the extremes in both groups, but they do suggest that different individuals respond very differently to different diets. This can be frustrating for some people who may not respond to a diet as others have. However, it also highlights that a person can be successful with a weight loss strategy even if other strategies have failed.
A word about fasting
Important: Plenity has not been evaluated with fasting regimens. Plenity is meant to be taken 20–30 minutes prior to lunch and again 20–30 minutes before dinner. Do not use Plenity unless you are using it prior to these meals. If you are interested in trying a fasting regimen, talk to your doctor before taking Plenity as it may not be appropriate for you.
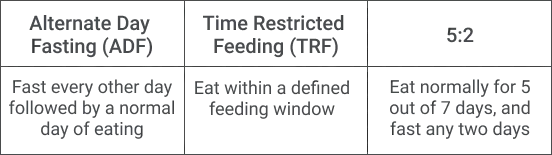
Intermittent fasting (IF) is all the buzz these days. But is it effective for weight loss? Does it have health benefits? There are many different fasting protocols. Probably the three most popular ones are alternate day fasting (ADF), time restricted feeding (TRF), and the 5:2 method.
ADF is exactly what it sounds like. Eat normally one day, fast the next, and keep alternating like this. Fast days can be a complete fast, where no calories are eaten, or they can just mean greatly reduced energy intake. TRF consists of restricting caloric intake to a specific “feeding window.” The most common way to do TRF is to restrict the eating window to 8 hours. For example, you may have your first meal at 12 pm and finish your last meal at 8 pm. This is commonly referred to as 16:8 (16 hours fasting followed by all meals within an 8 hour window). Finally, the 5:2 method consists of eating normally for 5 days and fasting two days per week. The fast days do not need to be consecutive. Like ADF, the 2 fast days may mean eating nothing at all or they may just mean eating very few calories.
Research shows that IF is effective for weight loss, but it is no more effective than continuous caloric restriction. In other words, the weight loss due to IF can be completely explained by reducing calorie intake. Some research shows that IF can improve insulin resistance even with the same amount of weight loss as a low-calorie diet, but more research is needed. Another small study showed that limiting food intake to 10 hours out of 24 hours (14 hour intermittent fasting) for 12 weeks led to weight loss and improved lipids in women with metabolic syndrome. Interestingly, the decreases in LDL were greater than what would have been expected from weight loss alone. Finally, there has been increasing interest in IF for disease prevention and longevity with multiple potential disease and age modifying mechanisms identified although there is no definitive evidence at this time.
So, what’s the bottom line? Should you try IF? Since weight loss does not have a one-size-fits-all solution, your goal is to find the most sustainable way to cut calories for you. This varies between individuals. Some people may find it easier to fast and relax more during the time they eat, while others will find fasting too uncomfortable. This was shown in a trial of 100 people where the IF group had a higher dropout rate than the calorie restricted diet group. If you decide to give fasting a try, make sure to discuss it with your primary healthcare provider. This is especially important if you are currently taking medications for type 2 diabetes or medications that should be taken with food. In these cases, the doses may need to be adjusted.
Are there scientifically backed weight loss tips?
There are many strategies that positively affect weight in some people. As with diets, drugs, and surgery, different individuals will respond to different things. The key to these weight loss strategies is to try them and only keep the ones that work for you.
Try eating more slowly
Eating more slowly may help you control your weight. I know. It sounds like an old wives’ tale. But some research suggests it might be true. For example, one study surveyed Japanese subjects and found that those who ate more quickly had a greater likelihood of being overweight. Another study showed that chewing food 50 times led to a decrease in caloric intake compared to chewing 15 times.
The mechanisms for this are not fully understood, but it’s possible that eating slower lessens hunger. For example, one study showed that eating slowly produced higher levels of GLP-1 and PYY (hormones that make you less hungry) after a meal than when eating more quickly. Regardless of how it works, it’s worth attempting eating slower when trying to lose weight or maintain weight loss.
What’s a calorie?
We always hear about needing to cut calories in order to lose weight. But what exactly does this mean? Let’s define what a calorie is first, and then get into why we need them and whether counting calories is a good idea.
A calorie is a unit of energy, just as a foot is a unit of distance and a pound is a unit of weight. Scientifically speaking, one calorie equals the amount of energy required to raise the temperature of one gram of water by one degree celsius. Yes, we know this is confusing.
What makes it even more confusing is that when we talk about calories in food, we mean something different. One calorie in food is actually equal to 1,000 of these scientific calories (this is also called one kilocalorie). Sometimes, to distinguish it, calories in food are written with a capital “C” as “Calorie.” More commonly, it is left lowercase. To straighten this out for you:
1 calorie in food = 1 Calorie = 1 kilocalorie = 1,000 calories (scientific definition)
Measuring food in units of calories gives an idea of the amount of energy in the food. Food naturally contains energy in the form of chemical bonds in carbohydrates, fats, proteins, and even alcohol. The more energy that is stored in these nutrients, the more calories food has.
Our bodies require a certain number of calories just to function each day. This is normally broken up into three components:
The energy our bodies use at rest: This is called the Basal Metabolic Rate (BMR) and accounts for 60–70% of the energy our bodies burn each day.
The energy our bodies use during movement: This is called the Non-Exercise Activity Thermogenesis (NEAT) and accounts for ~20–30% of the energy our bodies burn each day.
The energy our bodies use to process the foods we eat: This is called the Thermic Effect of Food (TEF) and accounts for ~10% of the energy our bodies burn each day.
If you are someone who exercises, your body burns additional calories from that exercise.
Don’t drink your calories
If you’re trying to lose weight, or to maintain weight loss you’ve already achieved, avoid liquid calories. Sugar sweetened beverages (SSBs), in particular, have been shown to induce weight gain in children and adults. Replacing SSBs with non-caloric beverages has been shown to help with weight loss.
The CDC states sugar-sweetened beverages (SSBs), “are any liquids that are sweetened with various forms of added sugars like brown sugar, corn sweetener, corn syrup, dextrose, fructose, glucose, high-fructose corn syrup, honey, lactose, malt syrup, maltose, molasses, raw sugar, and sucrose. Examples of SSBs include, but are not limited to regular soda (not sugar-free), fruit drinks, sports drinks, energy drinks, sweetened waters, and coffee and tea beverages with added sugars.” SSBs may also increase the risks of type 2 diabetes, cardiovascular disease and chronic kidney disease.
Try to stick with water, unsweetened tea, and coffee. Although diet beverages may seem like an attractive calorie-free option, there is some research showing that people who drink them have increased mortality compared to those who don’t. Until we know more, it may be best to skip diet soft drinks.
If you’re being cautious about drinking your calories, know that this does NOT apply to drinking protein shakes or meal replacements to help you control your calorie intake and lose weight. These shakes typically contain a balance of protein, carbohydrates and fat and are designed to replace a balanced meal while keeping the calories low.
Eat mindfully and avoid distracted eating
Mealtime was once a time when people would take a break from their day and eat a meal. Today, most people eat many meals while distracted. Whether it’s while driving, watching TV, or focusing on your computer screen, distracted eating may hinder your weight loss efforts. Research shows that distracted eating increases food intake immediately, but even more so later in the day.
If you’re trying to lose weight or maintain weight loss, it is best to avoid eating in front of screens or doing other things that distract you. Formal mindfulness training and meditation may be helpful, as well. These mindfulness interventions, sometimes referred to as mindfulness-based eating, have been shown to be effective for weight loss. They are also effective for depression and anxiety. These work best when they include formal mindfulness meditation with mindfulness exercises while eating.
Many resources exist in the form of books and CDs to teach mindfulness and formal training programs are available. Some of these programs are low cost or even free.
Eat a whole foods diet low in processed foods
Eating a diet that is mostly comprised of minimally-processed, whole foods may help your weight loss efforts and prevent weight gain/regain. “Processed foods are produced by adding salt, oil, sugar, or other culinary ingredients to minimally processed foods” and “ultra-processed foods are defined as multi-ingredient industrial formulations and include sugar sweetened beverages (SSBs), packaged breads, cookies, savory snacks, candy, ice cream, breakfast cereal, and pre-prepared frozen meals.”
An important study published in Cell Metabolism studied 20 subjects to assess the effects of eating a diet high in ultra-processed foods. For 2 weeks participants were given a diet high in unprocessed foods and for two weeks they were given a diet high in processed foods. They were allowed to eat as much as they wanted (ad libitum).
The study showed that subjects ate ~500 calories more during the 2 weeks when they ate an ultra-processed diet compared to the 2 weeks with the unprocessed diet. Furthermore, during the 2 weeks on the ultra-processed diet, they gained an average of 0.9 kg (2 lbs) and during the 2 weeks on the unprocessed diet, they lost an average of 0.9 kg (2 lbs).
The Gardner study cited above also suggests that eating unprocessed, or minimally processed, foods (foods that are close to how they are in nature) may help with weight loss. Two groups, a low carb group and a low-fat diet group, were instructed to: (1) “maximize vegetable intake; (2) minimize intake of added sugars, refined flours, and trans fats; and (3) focus on whole foods that were minimally processed, nutrient-dense, and prepared at home whenever possible.” Both groups lost weight in spite of the fact that they were not given caloric targets and did not count calories.
In this case, science reinforces what we already know intuitively. Eating whole, unprocessed foods that are close to their natural state is an important component of weight management. Also, beware of “healthy foods” from fast-food restaurants, like salads. They often contain dressings and sauces that quickly drive up the calorie count and can sabotage your weight loss efforts.
Weigh yourself regularly
Studies have shown that people who consistently weigh themselves at regular intervals are more likely to keep the weight off in the long term (5-10 years and beyond). How often you weigh yourself (multiple times a day, once a day, once a week, etc) is not as important as being consistent about checking your weight regularly. For example, if you prefer to weigh yourself every day, it’s important to keep weighing yourself every day. If you prefer weighing yourself once a week, you should keep weighing yourself once a week.
Track your food intake
Tracking what you eat may help you lose weight, although the research is mixed. One study showed that people who logged their food intake more often (2–3 times daily) lost more weight than those logging their food intake less frequently. Today, there are many apps available to help you with food tracking, such as myfitnesspal, myplate, and loseit! to name just a few.
Get enough sleep
Sleep deprivation has been linked with obesity in various studies. The mechanism is not totally clear, but it may be due to sleep deprivation’s effects on hormones that regulate appetite. Sleep has been shown to increase ghrelin levels and decrease leptin levels, which can be a cause of increased food intake and decreased energy expenditure. While everybody has their own individual sleep requirements, aim for at least 7-8 hours of restful sleep if you’re trying to lose weight and keep it off.
Get a coach
Having a coach help you through the weight loss process has been shown to be effective in the primary care setting. Coaching via telehealth has also been effective in aiding weight loss. Coaching may help through education, support, or accountability, but either way, it’s a good idea to get a coach.
Drink more water
Drinking more water has been shown to help with mild weight loss in overweight women and adults aged 55–75. Another large study that used urine samples to assess hydration found that people who were dehydrated had higher BMIs and were more likely to be obese, although it’s unknown whether the dehydration contributed to the higher body weight. Taking Plenity properly requires you to drink 2 glasses of water 20–30 minutes before lunch and again before dinner. Try drinking 2 glasses of water before breakfast as well in addition to drinking water when you are thirsty.
Have a plan/shopping list
“Failing to plan is planning to fail,” the saying goes. This couldn’t be truer than with dietary choices when trying to lose or maintain weight. Making good food choices is much harder when you’re starving after a long day at work and there’s a gallon of ice cream in your fridge just waiting to be devoured.
Making a shopping list with smart choices and sticking to it may be one of the most important things you can do when you’re trying to lose weight. Even in low-income households living in “food deserts,” people who always shop with a shopping list had lower BMIs and higher quality diets than those who did not always use a shopping list. Shopping lists may help shield us from having to make decisions when there are so many unhealthy choices in front of us, which can help us eat better and may help with weight control.
Use meal replacements
***Important: Plenity has not been studied with liquid meal replacement products. The safety and efficacy of combining Plenity with liquid MRPs is unknown.
This one obviously doesn’t go well with the tip above that recommends avoiding processed foods, but remember that you need to find what works best for you. For some people cooking meals may be too time consuming and is an obstacle to their weight loss efforts. In this case, meal replacements (MRs) may help.
MRs can come in the form of shakes, bars, soups, or prepackaged portion‐controlled meals. A 2019 study concluded that weight loss programs that included MRs resulted in more weight loss after one year than similar programs without MRs. Furthermore, the increased weight loss may persist for up to 4 years. It’s unclear how MRs work although they may help with weight loss by making it easier to stick with reduced calorie diet plans by increasing meal structure and decreasing mealtime decision making. MRs aren’t right for everyone, but they may be worth a try—especially if you’ve been struggling to prepare healthful, lower-calorie meals.
Decrease your variety of food that tastes too good
“Hyperpalatable” is a term used by scientists to describe foods that are highly processed and so delicious that they may cause addictive-like behaviors. These foods usually contain mixtures of fat, sugar, and salt that make it difficult to stop eating them. They are generally not found in nature. For example, people are much more likely to overeat sweet potato chips than they are to overeat sweet potatoes. The addition of fat and salt to the natural sweetness of a sweet potato creates a hyperpalatable food out of a natural food.
Increasing food variety has also been shown to increase food intake in the short-term, but we don’t know whether decreasing variety in the long-term has beneficial effects for weight loss. Since it’s plausible that decreasing food variety may help with your weight loss efforts, it’s a good idea to do so especially with hyperpalatable foods. You may also just try limiting your exposure to your personal trigger foods.
Be physically active
Being physically active is very important for those trying to lose or maintain their weight. Exercise is not as effective as dietary changes for weight loss, but it can help when added to dietary changes. Exercise seems much more important when it comes to preventing weight gain. It also seems to be helpful in preventing weight regain after weight loss. 90% of subjects in the National Weight Control Registry (NWCR) report exercising an average of one hour per day. Studies have shown that it takes 80 minutes of moderate exercise or 35 minutes of vigorous exercise per day to help with weight maintenance.
Even if you can’t meet these numbers, doing some physical activity is better than doing none. Aside from its importance in weight loss and maintenance, being physically active is one of the best things you can do for your health. Being physically active can lower your risk for hypertension, stroke, cancer, depression, diabetes, and it can even lengthen your life. This is true even without weight loss.
The Physical Activity Guidelines for Americans, 2nd Edition recommends that all adults perform at least 150–300 minutes per week of moderate-intensity physical activity (e.g., brisk walking) or 75–150 minutes per week of vigorous-intensity physical activity (e.g., running, spinning). Exercises geared toward increasing muscle strength (e.g., weight lifting, crossfit, pushups) are recommended 2 or more days per week. About 80% of adults and adolescents do not meet these recommendations.
Copy the habits of successful people
The National Weight Control Registry (NWCR) is a longitudinal study on over 10,000 people who have lost at least 30 lbs and kept it off for at least one year. The average weight loss was 66 lbs and the average time the lower weight was maintained was 5.5 years. This highly successful weight loss cohort has done a variety of things in the quest to lose weight and keep it off. The most important findings of the study are:
98% of people said they modified their food intake in some way. Dietary modification is considered to be essential in any weight loss program.
94% of people increased their physical activity. Walking is the most common form of physical activity, and 90% of people in the NWCR perform physical activity for an average of 1 hour per day.
78% of people report eating breakfast daily. IF (intermittent fasting) may be all the rage, but breakfast seems to be pretty common in the NWCR.
75% of people weigh themselves at least once per week. Many people are afraid to weigh themselves regularly, but regular self-monitoring is an important part of a weight loss or maintenance program.
62% of people watch fewer than 10 hours of TV per week. This is a lot less than most Americans.
55% of people lost weight by using some type of program. Many people can lose weight on their own, but some people may do better with outside help.
So there you have it. Modify your diet, exercise an hour per day, weigh yourself at least once a week, and limit TV. These things may work together to increase your chances of weight loss success.
When is weight a medical problem?
Overweight and obesity are among the most common and widespread medical issues in the developed world. The definition and classification of overweight and obesity are based on a person’s Body Mass Index (BMI) measured in kg/m² according to the following definitions:
<18.5: underweight
18.5-24.9: normal weight
25-29.9: overweight
30-34.9: Class 1 obesity
35-39.9: Class 2 obesity
40 or higher: Class 3 obesity
You can calculate your BMI by entering your weight and height here.
What is BMI? BMI is a person’s weight in kilograms (1 kilogram equals 2.2 pounds) divided by the square of their height in meters (1 meter equals ~3 feet 3 inches). While a BMI is not a direct measurement of body fat, research has shown that BMI is comparable to measurements of body fat that are more direct (e.g., skinfold thickness, underwater weighing, dual-energy x-ray absorptiometry or DEXA, bioelectrical impedance).
Just as important, BMI correlates with the development of diseases and their outcomes. Simply stated, BMI is an excellent, inexpensive, easy-to-perform test that indicates whether a person is underweight, overweight, obese, or at their optimal weight. Some exceptions include very muscular people in whom BMI overestimates body fat and people with low muscle mass in whom BMI underestimates body fat.
For too long, obesity was seen as a problem of willpower. However, many organizations now classify it as a chronic disease, including the American Medical Association (AMA) and the World Health Organization (WHO). It’s important to understand that just like other chronic diseases that do not have a cure, treatment needs to continue indefinitely. This is true for obesity regardless of the interventions made. The only intervention that generally does not need to be repeated is bariatric surgery, but this is because the changes (altered anatomy) are permanent. Nevertheless, even people who undergo bariatric surgery must commit to lifelong changes in lifestyle.
According to the Centers for Disease Control and Prevention (CDC), almost 40% of adults in the US are classified as obese along with almost 20% of children ages 2–19. When overweight and obesity are added together, they account for over 70% of US adults.
Although BMI has traditionally been used to categorize weight, many studies suggest that waist circumference is a greater risk factor than BMI. In fact, larger waist circumferences may be a risk factor for death even in those with a BMI in the normal range.
Overweight and obesity take a heavy toll on those with either condition. Some of the health consequences of obesity include:
An increased risk of dying from all causes
Cardiovascular risk factors such as high blood pressure (hypertension), abnormal cholesterol levels (high LDL, low HDL, and/or high levels of triglycerides; dyslipidemia), Type 2 diabetes
Coronary heart disease
Heart failure
Stroke
Chronic kidney disease
Gallbladder disease
Fatty liver disease, which can lead to liver failure and require a liver transplant
Osteoarthritis (a breakdown of cartilage and bone within a joint)
Sleep apnea and breathing problems
Some cancers, including endometrial, breast, colon, kidney, gallbladder, liver
Low quality of life
Depression, anxiety, and other mental health disorders
Pain and poor physical function
Obesity contributes to work absenteeism: individuals with obesity miss up to two additional workdays per year when compared to people without.
The weight loss industry is full of promises of effortless weight loss. Unfortunately, most of these promises are empty, and almost half of adults try to lose weight in any given year. 70 billion dollars is spent each year by people trying to lose weight. There is a great need for safe and effective weight loss tools to help people improve their health and quality of life.
Why do only some people gain weight?
Most people think that overweight and obesity are primarily problems with willpower. In reality, this couldn’t be further from the truth. Our eating behaviors and the amount of energy we expend are heavily influenced by our genes—and the tendency to gain weight has a large genetic component. Studies have shown that 31–90% of the variance of BMI between people is inherited. This means that the tendency to gain weight is largely, though not completely, determined by our genes.
The question many people ask is if obesity is largely determined by genetics, why did the modern obesity epidemic only start in the 1960s? Since the early 1960s, childhood and adult obesity have roughly tripled. How can genetics account for this?
The answer is that while the tendency to gain weight is heavily influenced by our genes, our environment and behaviors can help determine whether we actually gain weight. Scientists call environments that cause us to gain weight obesogenic environments. The increased availability of large portions of calorie-dense, inexpensive, hyperpalatable foods that are aggressively marketed—coupled with our modern sedentary lifestyles—is largely responsible for the modern obesity epidemic. Some people seem immune to these influences but it is their genes that protect them from weight gain even in this less-than-ideal environment.
The good news is that our genes are not our destiny. Eating behaviors and exercise can both protect us from weight gain in spite of our genes. In conjunction with starting Plenity, adopting the tips below can help in your weight loss efforts.
Why is it so difficult to lose weight and keep it off?
While most weight loss programs focus on losing weight, the reality is that keeping weight off once it’s lost is much more difficult than losing it. Most people know this. After all, it’s common for people to struggle for decades losing hundreds of pounds collectively only to regain the weight. Why does this happen?
We already explained how our genes, environment, and behavior conspire to determine our weight. Some of the biological pathways involved in determining our susceptibility to weight gain explain why keeping weight off is so difficult. Despite our best conscious efforts, the fact is there are many unconscious processes that determine how much we eat and how much energy we expend. The most important of these include brain pathways and hormones that work together to determine how hungry we are and how much energy we burn.
Orexigenic signals tend to cause us to eat more while anorexigenic signals tend to cause us to eat less. Orexigenic signals include:
Neuropeptide Y (NPY) and Agouti-related protein (AgRP): These are chemicals made in the brain that increase appetite and decrease metabolism and energy expenditure.
GIP and Ghrelin are gastrointestinal hormones that increase appetite and decrease energy expenditure.
Anorexigenic signals include:
Pro-opiomelanocortin (POMC) and cocaine- and amphetamine-regulated transcript (CART): These are chemicals made in the brain that decrease appetite and increase metabolism and energy expenditure.
Glucagon-like peptide-1(GLP-1), cholecystokinin (CCK), peptide YY (PYY), leptin, pancreatic polypeptide (PP), amylin: These are gastrointestinal hormones that decrease appetite and energy expenditure.
Research shows that the body “wants” to maintain a certain weight. It makes sense that when food is scarce (as during a calorie restricted diet) the body would shift how it functions by making you more hungry (so you seek food more aggressively) and burn calories more slowly. The body accomplishes this by increasing orexigenic hormones and decreasing anorexigenic hormones. In addition, the amount of energy burned, both at rest and during exercise, decreases. These changes that cause the body to “defend” a certain weight are often referred to as the “set point model.”
To summarize, losing weight causes an increase in hunger and a decrease in the amount of energy burned at rest and during exercise. These changes make it difficult to maintain the new bodyweight after weight loss has been achieved.
While these changes explain why keeping weight off is difficult, successful maintenance after weight loss is possible. As you’ll read below, exercise, behavioral changes, and medical treatments, such as Plenity, can greatly increase your chances of success.
Energy balance and weight loss
When all is said and done, all weight loss interventions are designed to change your energy balance, meaning that you burn more calories than you consume. It is possible to estimate how many calories the average person burns each day. For the average sedentary woman, 1,600–2,000 calories are burned. For the average sedentary man, 2,000–2,400 calories are burned. Depending on each individual’s weight and level of activity, these values may be higher or lower.
Energy balance refers to the balance between the calories burned by the body and the calories eaten. When people take in the same number of calories as they burn, they are said to have a neutral energy balance. In a neutral energy balance, an individual does not gain or lose weight. When people take in more calories than they burn, they are said to have a positive energy balance. In a positive energy balance, an individual gains weight. When people take in fewer calories than they burn, they are said to have a negative energy balance. In a negative energy balance, an individual loses weight.
Ways to be in negative energy balance include eating less (therefore taking in fewer calories) or exercising more (therefore burning more calories). This is why people talk about cutting calories when they talk about losing weight.
It’s important to note that, when it comes to calories, lower is not necessarily better for long-term weight loss. Research shows that diets containing fewer than 800 calories per day (known as very-low-calorie diets or VLCDs) do produce greater weight loss in the short term than conventional reduced-calorie diets. However, this benefit is not maintained over 18–26 months. VLCDs also increase the risk of adverse effects, including gallstones, cold intolerance, hair loss, constipation, dizziness, fatigue, headache, and dehydration. Therefore, VLCDs are not recommended over more moderate calorie reductions.
So should you count your calories? For some people, it may help to count calories for three or four days prior to starting a weight-loss regimen to get a better idea of their maintenance needs. You can use apps, like myfitnesspal or loseit!, to do this. However, for most people, counting calories every day is inconvenient and may not help with long-term weight loss. The more important thing is to find a sustainable way of eating that results in decreased caloric intake in the easiest way possible.
What did the clinical research on Plenity show?
The pivotal trial that earned Plenity FDA clearance was called the Gelesis Loss Of Weight trial or GLOW trial. The trial studied over 400 people ages 22–65 who had a BMI of 27–30 kg/m² who did not have type 1 diabetes or gastrointestinal or other endocrine disorders. Those with a BMI <30 had to have hypertension, diabetes, or abnormal lipid levels. The study lasted 24 weeks with a smaller number of patients continuing on to an extension study, called GLOW-EX.
The Plenity group took 3 capsules of Plenity with 2 glasses of water 20–30 minutes before lunch and dinner, and the control group took 3 placebo pills with 2 glasses of water 20–30 minutes before lunch and dinner. Both groups were counseled to decrease their caloric intake by 300 calories and to exercise moderately (e.g., brisk walking) for 30 minutes a day. Some of the most important results are summarized below.
59% of the Plenity group lost at least 5% of their body weight compared to 42% in the placebo group
27% of the Plenity group lost at least 10% of their body weight compared to 15% in the placebo group
Average weight loss in responders in the Plenity group was 10.2% of their body weight
Losing at least 3% of body weight after 8 weeks while taking Plenity was highly predictive of success (85% of these people lost at least 5% body weight at 24 weeks).
People with prediabetes (fasting blood sugar of 100–125 mg/dL) were even more likely to be successful than those with normal fasting blood sugar.
The GLOW-EX study enrolled 39 people who completed the GLOW study, 21 from the Plenity group and 18 from the placebo group. Both groups had lost ~7% of their body weight during the first 24 weeks of the GLOW study. All participants continued with Plenity for weeks 25–48. The study showed that the original Plenity group maintained their weight loss at 48 weeks and the placebo group actually lost additional weight when they added Plenity for the final 24 weeks.
The GLOW-EX study is significant because—contrary to other weight loss interventions—it showed that patients who used Plenity maintained the benefits for at least 48 weeks.
Other weight loss treatments
Aside from lifestyle interventions, there are other weight loss treatments that have been proven to be effective. The two most important ones are weight loss medications and bariatric surgery.
Weight loss medications
***Important: Plenity has not been studied with other weight loss medications, also known as anti obesity medications. The safety of combining Plenity with other weight loss medications is unknown and this combination is not recommended until more research is done.
There are currently 6 weight loss medications that are approved by the FDA. All of these drugs are indicated for people with a BMI of 30 or more or people with a BMI of 27 or more with at least one weight-related comorbidity (e.g., hypertension, diabetes, hyperlipidemia). They can cause moderate weight loss in some people and should be stopped after 12 weeks in people who are not responsive (weight loss of at least 5% of body weight in 12 weeks). There is a wide range of responsiveness to these treatments. None of these drugs should be used in pregnant or breastfeeding women.
Phentermine: This drug has stimulant properties and it decreases appetite. It is only approved for short-term treatment. It is considered a “scheduled” drug by the Drug Enforcement Administration (DEA), which means it has some abuse potential.
Phentermine/Topiramate (Qsymia®): This is a combination of phentermine and the anti-seizure drug, topiramate. The combination has been shown to be superior to either drug alone and both drugs work to reduce appetite. It is scheduled by the FDA and has abuse potential.
Liraglutide (Saxenda®): This is an injectable drug that is part of a family of drugs called GLP-1 agonists. They are most commonly used to treat diabetes. Saxenda contains the same drug as Victoza, which is used to treat type 2 diabetes but at a higher dose (3 mg vs 1.8 mg).
Lorcaserin (Belviq®): This drug works by activating a specific serotonin receptor (5-HT2C receptor) in the brain to promote a feeling of fullness (satiety). It is also scheduled by the FDA and has abuse potential. (THIS MEDICATION HAS BEEN WITHDRAWN FROM THE MARKET in 2020)
Naltrexone/Bupropion (Contrave®): This drug combines naltrexone, which is used to treat drug and alcohol addiction and bupropion, which is used to treat depression and help people quit smoking. Bupropion works by causing satiety (a sense of fullness) through activation of POMC neurons in the hypothalamus and naltrexone blocks the feedback mechanism to prolong the sense of satiety.
Orlistat (Xenical®, Alli®): This drug works by decreasing the amount of fat that is absorbed from the diet. It is available in prescription (Xenical®) and non-prescription (Alli®) strengths.
Bariatric surgery
***Important: Plenity should not be used by people who have undergone bariatric surgery.
Bariatric surgery is currently the most effective method for weight loss. Currently, bariatric surgery is indicated for people with a BMI of 40 or more (or >100 lbs overweight) or a BMI of 35 or more with at least one weight-related comorbidity, including:
Type 2 diabetes (T2DM)
Hypertension
Sleep apnea and other respiratory disorders
Non-alcoholic, fatty liver disease
Osteoarthritis
Lipid abnormalities
Gastrointestinal disorders
Heart disease
Practically speaking, almost everyone with a BMI of at least 35 qualifies. Some research also shows that even people who are not eligible obtain health benefits from bariatric surgery. The American Society for Metabolic and Bariatric Surgery (ASMBS) recently updated its position stating that bariatric surgery should be an option for many people with a BMI of 30 or more, especially taking into account obesity-related comorbidities.
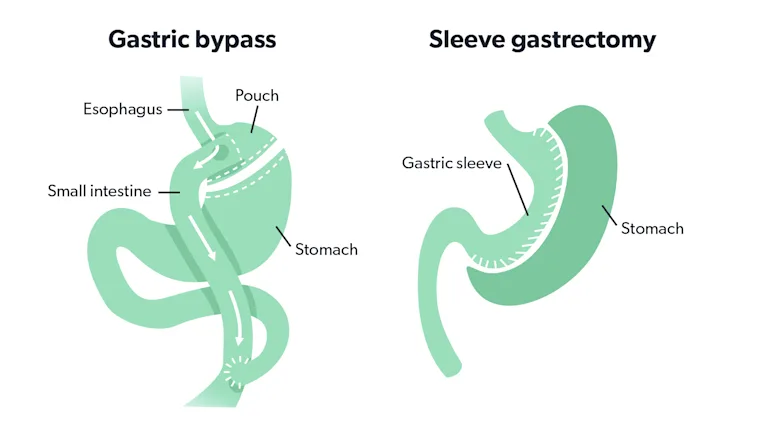
The two main procedures performed today are Roux-en-Y gastric bypass and laparoscopic vertical sleeve gastrectomy (sometimes just called sleeve gastrectomy). Older surgeries like duodenal switch and gastric banding are rarely done due to unacceptably high rates of adverse events.
In Roux-en-Y gastric bypass, the stomach is divided and a small pouch is created and attached directly to the small intestine further down than the original beginning of the small intestine. Most of the stomach and part of the small intestine are “bypassed”.
This makes the stomach smaller so it gets full more easily. It also bypasses a portion of the intestines that absorbs food and nutrients. However, most of the beneficial effects are thought to be caused by changes in GI hormones (e.g., increased GLP-1 and PYY and decreased ghrelin), nerve signaling, and other changes (e.g., altered gut microbiome). These work to decrease hunger and increase satiety. People who undergo a Roux-en-Y gastric bypass need to take vitamin and mineral supplements as they are at increased risks of deficiencies due to malabsorption as described above.
The sleeve gastrectomy involves removing about 75% of the stomach, leaving a thin gastric tube, or “sleeve”, attached to the usual beginning of the small intestine. This surgery is less invasive than the Roux-en-Y gastric bypass as there is less cutting and stapling of the digestive tract. There is also no redirection of the flow of food.
Sleeve gastrectomy seems to work by many of the same mechanisms as Roux-en-Y gastric bypass, including restricting food intake due to the changed anatomy, hunger hormone changes (increased GLP-1 and PYY and decreased ghrelin), and changes to the gut microbiome. Vitamin and mineral supplements are often prescribed after sleeve gastrectomy although some research shows it may not be necessary long-term.
Roux-en-Y gastric bypass and sleeve gastrectomy are effective for weight loss, causing a 50%–80% excess weight loss (EWL). This means that if someone is 100 lbs overweight, s/he can expect to lose 50–80 lbs with one of these surgeries. Some studies show that weight loss is similar for both surgeries, while others show that Roux-en-Y gastric bypass causes greater weight loss. Selecting the appropriate surgery should be done in consultation with a bariatric surgery team, which often includes a bariatric surgeon, a medical doctor, and a mental health professional.
Both Roux-en-Y gastric bypass and sleeve gastrectomy also have beneficial effects on obesity-related health measures, such as diabetes, hypertension, and lipid abnormalities. Some people can stop their medications for these disorders following bariatric surgery.
Both surgeries decrease mortality, but also have risks for complications. For example, a study published in 2019 showed that both forms of surgery decreased mortality over seven years but also increased the risk of complications and hospitalizations.
Bariatric surgery represents the most effective means of weight loss treatment available today. It isn’t for everybody, but if you are at least 100 lbs overweight and/or have obesity-related complications, and haven’t been successful with other methods, it’s an important option to consider.
Gastric balloon
***Important: Plenity should not be used by people with gastric balloons.
The gastric balloon, also called an intragastric balloon or a stomach balloon, is another option for weight loss that does not involve taking medications and does not involve surgery. The gastric balloon is approved for people with a BMI of 30-40 along with diet and exercise and is currently offered by three companies. A 2017 review of studies found that use of the balloon resulted in a nearly 10% loss of body weight.
The balloon is initially placed in the stomach with an endoscope, a type of flexible camera. Once in the stomach, the balloon is inflated with saline. It then remains in the stomach where it works by applying stretch, making the patient feel fuller. The gastric balloon is a temporary device while the patient learns new dietary habits that are intended to be lifelong. After the balloon has been in place for up to six months, it is deflated and removed from the stomach.
Some people experience pain and nausea after insertion of the balloon, but these symptoms tend to go away after a few days. There is a risk that the balloon deflates, in which case it may travel through the digestive system and cause a blockage. Another concerning risk is that the balloon can cause a hole in the stomach lining, which is called a gastric perforation and may be a surgical emergency. Between 2016-2018, the FDA received reports of twelve deaths that were associated with the gastric balloon. Some, but not all, of these deaths were associated with gastric perforation. The FDA has stated that they “will continue to monitor the safety and effectiveness of these approved devices.” One 2018 study found that, compared to laparoscopic bariatric surgery, gastric balloons had a higher rate of adverse events. This was measured by looking at the relative number of times patients required reintervention after the procedure (4.2% of the time for gastric balloons versus 1.0% of the time for laparoscopic bariatric surgery). The study suggested the use of gastric balloons be reconsidered.
Conclusion
This is a great deal of information and it can feel overwhelming. We understand. Remember, each attempt at weight loss helps you find the choices and treatments that will work for you. Each step, whether you achieve everything you set out to accomplish or not, helps determine the next steps that will work even better.
The good news is that you’re already here. You have already recognized that weight loss is appropriate for you and you are taking the steps to decrease your risk of heart disease, high blood pressure, type 2 diabetes, and certain types of cancer among other diseases.
Plenity is a very useful weight loss tool, but it does require work on your part as well. Remember that you are never alone. We are here to help you. If you have questions or if anything is unclear, reach out. We are here to support you.