Here's what we'll cover
Here's what we'll cover
Body acne, while not always as apparent as facial acne, can be annoying. And it isn’t something that comes with an instant fix. However, that doesn’t mean you can’t do anything about it.
Here’s what you need to know about body acne, from those pesky bumps on your chest to harder-to-reach “bacne.”
What is body acne?
Body acne—sometimes referred to as truncal acne (as in affecting the trunk of the body)—isn’t all that different from facial acne. Truncal acne, like facial acne, is acne vulgaris, which is the most common skin condition in the United States, affecting 40–50 million people at any given time (AAD, n.d.).
The data is not as clear about the prevalence of body acne. It is normal to have body acne, and it is estimated that more than half of people with facial acne also have body acne. It may be slightly more common in men, although the data is by no means definitive (Del Rosso, 2019).
Many people only mention their body acne after being directly asked about it, so it’s tough to know precisely how many people it affects. Severe truncal acne can lead to scarring if not treated appropriately (Del Rosso, 2019).
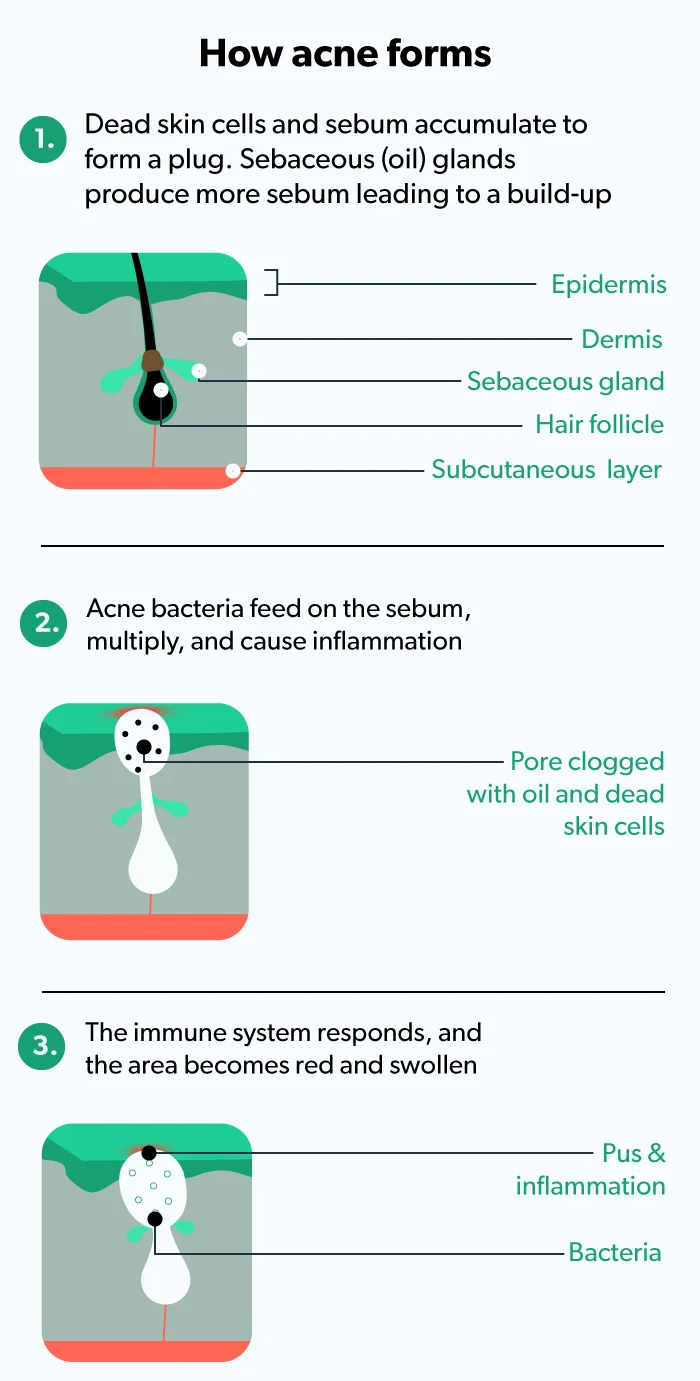
Like facial acne, body acne occurs when skin pores get clogged by excess oil (sebum), debris, and dead skin cells. The blocked pore creates an ideal environment for skin bacteria (C. acnes) to grow and flourish, leading to inflammation and infection. The combination of these factors causes the pimples that we all associate with acne. In the case of body acne, blemishes appear on the chest, back, or other parts of the body; facial acne is limited to the face (Sutaria, 2020).
In the case of truncal acne, excess oil may play less of a role than in facial acne because the skin on the rest of your body has fewer sebaceous glands (oil-producing glands) than on the face. Your truncal skin is more likely affected by things like friction (Del Rosso, 2019).
Signs and symptoms of body acne
As a general term, body acne appears on the back, chest, butt, legs, and bikini line. The different types are simply named based on the location of the acne breakouts, including:
Back acne
Chest acne
Butt acne
Bikini line acne
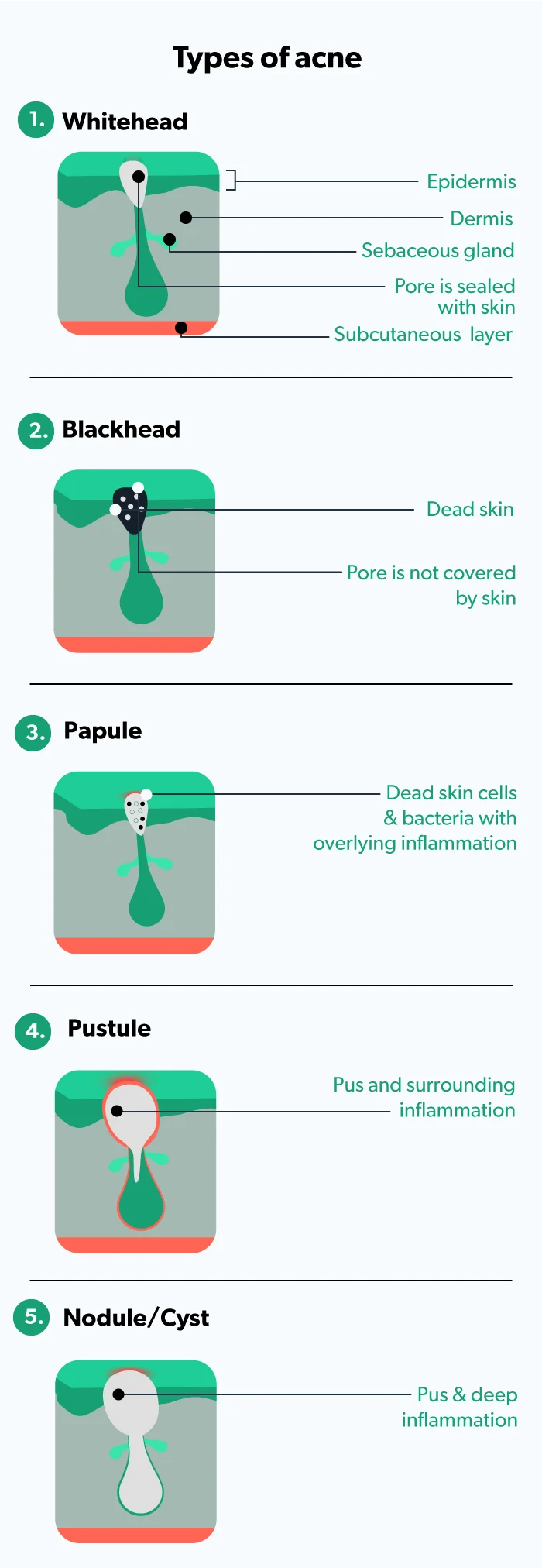
Most people already know the signs of acne, but sometimes acne blemishes look different from each other. In truncal acne, you can have a bunch of one type or a mix of various ones. The more inflammation and infection, the more severe the acne. The common signs of the different types of acne include (Sutaria, 2021):
Whiteheads: no inflammation and pore is sealed with skin (closed comedones)
Blackheads: no inflammation and pore is open (open comedones)
Papules: small amounts of inflammation
Pustules: more inflammation and pus in the pore
Nodules/cysts: deep inflammation and infection
Body acne causes and risk factors
Body acne may be due to any number of factors, including (Sutaria, 2021; Dréno, 2018):
Genetics
Hormonal changes (like pregnancy, menstruation, menopause, etc.)
Stress
Medical issues (like polycystic ovary syndrome or PCOS)
Cosmetics
Skincare habits
Medications (like corticosteroids)
However, body acne is more prone than facial acne to other causes, like friction or acne mechanica.
Back and chest acne
It’s possible to develop both inflammatory and non-inflammatory acne on your back and chest. Inflammatory acne is red and raised, whereas non-inflammatory acne—which includes whiteheads and blackheads—doesn’t involve any swelling or redness.
Many people get acne mechanica, which is acne caused by something rubbing the skin on their back or chest. This may be especially common for athletes, who use equipment that constantly rubs the same area (Mazhar, 2019). Similarly, sports bras may be common culprits for zits and other blemishes caused by rubbing and sweat.
Equipment isn’t always to blame, though. Sweating, even without workout gear rubbing the area, can kick off a breakout. That's why you should change out of your sports bra, workout clothes, etc., as soon as you can after exercise to reduce the amount of time your skin is in contact with any sweat trapped in the fabric.
Common causes of acne on the back and chest also include soaps, moisturizers, and hair products with oils in them. If you already have oily skin, stick to non-comedogenic products; these products don’t tend to have heavy oils, which could exacerbate issues with clogged pores. Prolonged sun exposure, especially without sunscreen, can dry out the skin, and trigger more oil production, which may end up clogging pores on your chest and back (Dréno, 2018).
Leg and butt acne
Sometimes those bumps on your butt (sometimes called “buttne”) or inner thigh are caused by prolonged sitting, sweating, or frequent friction on the skin—likely another instance of acne mechanica (Dréno, 2015; Dréno, 2018).
In other instances, your leg and butt zits may actually be folliculitis or inflammation of the hair follicles. Folliculitis may cause little red bumps or pimples with whiteheads around hair follicles that look like acne.
There are many different causes of folliculitis, and examples of this hair follicle infection include razor burn, hot tub rash, and barber’s itch. These bumps—which may appear red, swell, itch, or even contain pus—can be caused by (Winters, 2021):
Hot tubs (generally improperly cleaned ones)
Shaving, plucking, or waxing
Tight clothing
Weight gain
Certain medications
Bikini line acne
If your body acne appears around the bikini line, you’re most likely either dealing with folliculitis or ingrown hairs. Waxing may cause folliculitis, while shaving is a common culprit for both ingrown hairs and folliculitis (Kolalapudi, 2020; Sukakul, 2021).
How to get rid of body acne
Several therapies may help your body acne, but unfortunately, there’s no universally successful truncal acne treatment (Del Rosso, 2019). Working with a dermatologist, who can assess the specifics of your breakouts, like severity, skin type, etc., may be your best bet to crafting a skincare routine and body acne treatment plan.
Back and chest acne treatments
Topical retinoids, medications made from vitamin A (retinol), may help improve your acne. Tretinoin, one of the most commonly used prescription acne treatments, works against many factors that cause acne. They treat acne by unclogging pores, decreasing oil production, and reducing the inflammatory response. They help clear acne and prevent new eruptions—both on your face and body (Yoham, 2021).
Often, combination therapy is most successful for truncal acne (Del Rosso, 2019). Spot treatments and body washes and cleansers designed for acne-prone skin may both be helpful. Other treatments that can help with back and chest acne include:
Benzoyl peroxide: a topical body acne treatment that may help clear and prevent breakouts by attacking and reducing the C. acnes (formerly P. acnes) bacteria that live on the skin. It may be used alone or in combination with other topical or oral treatments and may even help reduce acne in as little as five days (Zaenglein, 2016).
Skincare products that use alpha-hydroxy acids, or AHAs: Glycolic acid (a commonly used AHA) can potentially improve acne by killing skin bacteria and decreasing inflammation at low concentrations. However, glycolic acid is often used at high concentrations (>10%) for chemical peels. Chemical peels work by exfoliating the outermost layers of skin. These procedures can help back acne but may lead to scarring if used for chest acne (Tang, 2018; Castillo, 2018).
Acne products that include salicylic acid, a beta-hydroxy acid (BHA), may be beneficial. Although more research is needed, some studies show that salicylic acid helps unclog pores (Zaenglein, 2018).
Topical azelaic acid can improve your body acne by unclogging pores, killing skin bacteria, and decreasing inflammation (Zaenglein, 2018; Del Rosso, 2019).
Dapsone gel may help your body acne by decreasing inflammation and may be a helpful addition to other acne treatments (Zaenglein, 2018; Del Rosso, 2019).
Lastly, for severe cases of body acne, oral medications (i.e., pills) are an option. Oral antibiotics (like doxycycline) and oral retinoids (like isotretinoin) may improve acne that is not responding to topical therapy. Your dermatologist will help guide your treatment and monitor your progress, especially if you are on oral medicines for your acne (Del Rosso, 2019).
Tretinoin Important Safety Information: Read more about serious warnings and safety info.
Azelaic Acid Important Safety Information: Read more about serious warnings and safety info.
Butt acne treatments
While some factors make certain people more susceptible to developing acne mechanica or folliculitis, it can be relatively easy to get rid of if you know the cause. Once you’ve identified the habit that is causing your butt acne, stopping it will usually improve the blemishes.
Avoid prolonged contact with sweat by rinsing off and changing your clothes soon after you work out. Opt for looser clothing if repetitive rubbing is the cause. If shaving is the issue, use a sharp, clean razor and shave in the direction the hair grows to help prevent future cases of folliculitis. If you already have folliculitis, applying warm compresses 3–4 times a day for 15–20 minutes may help heal your bumps faster (Winters, 2021).
Bikini acne treatments
If you’re treating bumps along your bikini line, make sure you avoid using harsh exfoliants on this sensitive skin. Shaving with a sharp, clean razor in the direction of hair growth may help prevent bumps in the future. You should also use shaving cream and clean your razor after each swipe. Warm compresses may speed the healing of existing blemishes (Winters, 2021).
How to prevent body acne?
While there’s no way to 100% prevent body breakouts, you can change certain habits to help keep your body clear, including:
Using skin and hair products that say things like non-comedogenic, oil-free, non-acnegenic, or “won’t clog pores”
Washing your skin with a gentle cleanser, especially after sweating
Avoiding scrubbing or over-cleansing
Moisturizing regularly
When to see your healthcare provider
Many people find their body acne both frustrating and embarrassing. The good news is that body acne can be treated. Over-the-counter topical treatments can often help with mild acne, but it may take some trial and error to find what works for your skin. If your acne doesn’t improve, is causing dark spots or scars, or is getting worse, seek medical advice from a dermatologist who can discuss many of the prescription treatment options with you.
There’s a good chance that a combination of therapies will be needed to improve your body acne. Treatment is important because if you let severe acne go untreated for too long, you can end up with body acne scars that are even harder to treat.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
American Academy of Dermatology (AAD). (n.d.). Skin conditions by the numbers. Retrieved November 1, 2021 from https://www.aad.org/media/stats-numbers
Castillo, D. E., & Keri, J. E. (2018). Chemical peels in the treatment of acne: patient selection and perspectives. Clinical, Cosmetic and Investigational Dermatology , 11 , 365–372. doi: 10.2147/CCID.S137788. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30038512/
Del Rosso, J. Q., Stein-Gold, L., Lynde, C., Tanghetti, E., & Alexis, A. F. (2019). Truncal acne: a neglected entity. Journal of Drugs in Dermatology:JDD , 18 (12), 205–1208. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31859617/
Dréno, B., Bettoli, V., Araviiskaia, E., Sanchez Viera, M., & Bouloc, A. (2018). The influence of exposome on acne. Journal of the European Academy of Dermatology and Venereology : JEADV, 32 (5), 812–819. doi: 0.1111/jdv.14820. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5947266/
Dréno, B., Bettoli, V., Perez, M., Bouloc, A., & Ochsendorf, F. (2015). Cutaneous lesions caused by mechanical injury. European Journal of Dermatology: EJD , 25 (2), 114–121. doi:10.1684/ejd.2014.2502. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26069089/
Kolalapudi, S. A., Mahesh, A. R., Arumilli, P. C., Kotha, S., Krishna Snigdha, A. G., & Saka, S. (2020). Dermatoses occurring after parlor procedures. Journal of Cutaneous and Aesthetic Surgery , 13 (4), 357–360. doi: 10.4103/JCAS.JCAS_43_20. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061649/
Mazhar, M., Simpson, M., & Marathe, K. (2019). Inner thigh friction as a cause of acne mechanica. Pediatric Dermatology , 36 (4), 546–547. doi: 10.1111/pde.13817. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30883890/
Sutaria, A. H., Masood, S., & Schlessinger, J. (2021). Acne vulgaris. [Updated Aug 9, 2021]. In: StatPearls [Internet]. Retrieved on Nov. 4, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK459173/
Sukakul, T., Bunyaratavej, S., Chaweekulrat, P., Trakanwittayarak, S., & Varothai, S. (2021). Facial hair shaving behavior and skin problems of shaved areas of males. The Journal of Dermatology , 48 (9), 1409–1413. doi: 10.1111/1346-8138.16034. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34254359/
Tang, S., & Yang, J. (2018). Dual Effects of Alpha-Hydroxy Acids on the Skin. Molecules , 23 (4), 863. doi: 10.3390/molecules23040863. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6017965/
Winters, R. D., & Mitchell, M. (2021). Folliculitis. [Updated Aug 11, 2021]. In: StatPearls [Internet]. Retrieved on Nov. 4, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK547754/
Yoham, A. L., & Casadesus, D. (2020). Tretinoin. [Updated Dec 5, 2020]. In: StatPearls [Internet]. Retrieved on Nov. 4, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK557478/
Zaenglein, A., Pathy, A., Schlosser, B., Alikhan, A., Baldwin, H., & Berson, D. et al. (2016). Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology , 74 (5), 945-973.e33. doi: 10.1016/j.jaad.2015.12.037. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26897386/
Zaenglein, A. L. (2018). Acne vulgaris. The New England Journal of Medicine , 379 (14), 1343–1352. doi: 10.1056/NEJMcp1702493. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30281982/










