Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Nobody ever wants to hear that they have cancer, but some forms of cancer are much more treatable than others. Testicular cancer is one of these.
While testicular cancer is the most common cancer in men aged 15 to 45 years old, it's considered to be highly curable (over 90%). This is especially true when it is diagnosed and treated at an early stage (Gaddam, 2021).
So what’s the key to detecting and treating testicular cancer early? Learning how to check for testicular cancer at home, the signs of testicular cancer, and when you should go see a healthcare provider.
What is a testicular self-exam?
Testicular cancer is caused by a complex interaction of risk factors in your environment and genetics. It represents about 1% of all tumors in men; however the incidence of testicular cancer is growing (Gaddam, 2021).
Cases of testicular cancer have been rising, especially in industrialized nations. Over the last 40 years in the United States, the frequency of testicular cancer diagnoses have doubled. This makes early detection and treatment even more important (Gaddam, 2021).
A testicular self-exam is a quick and simple procedure that you can do at home. It allows you to get familiar with your own body and notice any changes that might signal a health problem.
Learning how to check for testicular cancer at home is an effective way to promote (Rovito, 2018):
The health of your genitals and urinary tract
Self-awareness of your body
Your overall health and wellness
If you find anything out of the ordinary, you can see your primary healthcare provider or a urologist and get treatment without delay, even if it isn't likely cancer.
How to check for testicular cancer
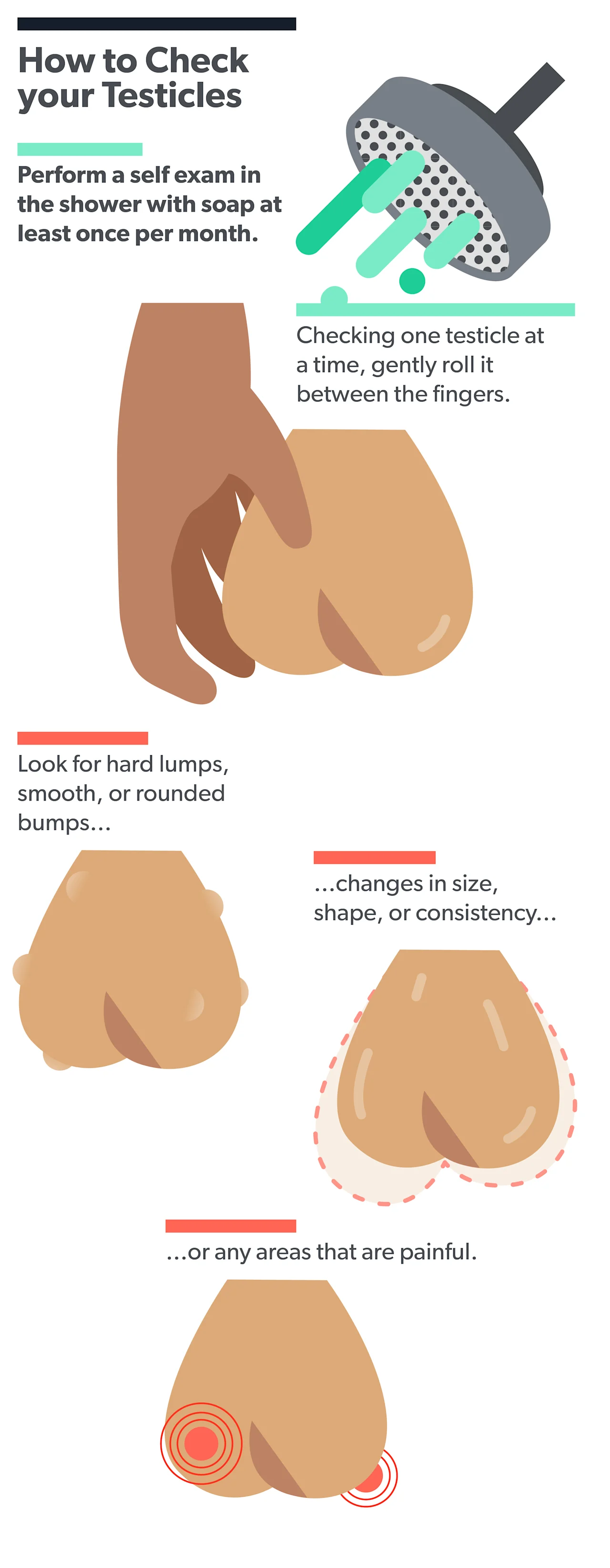
The best time to perform a testicular self-exam is after a shower when the skin is warm and relaxed. This check is easy to perform and takes only a few minutes.
Stand unclothed in front of a mirror.
Hold your penis out of the way and examine the skin of the scrotum.
Use your right hand to gently roll your right testicle between your thumb and fingers.
Look and feel for new lumps, bumps, painful spots, new changes in testicular size, or any other changes.
Repeat with your left hand on your left testicle.
You are looking for changes in the size, shape, or feel of your testicles. It's entirely normal for one testicle to be a different size or shape than the other, but those differences shouldn’t change over time. It’s also normal for one testicle to hang lower than the other.
You might feel a soft, ropy cord leading upward from the top of the back of each testicle. There is no need to worry about this. This is called the epididymis and is a normal part of your scrotum. It helps store and move sperm.
You might also notice other things about your testicles, such as ingrown hairs, a rash, or other skin problems. These aren’t signs of cancer, but you may still want to discuss them with your healthcare provider.
Who should perform a testicular self-exam, and how often?
The U.S. Preventive Services Task Force (USPSTF) is an organization that rates the evidence for and against different preventative healthcare measures. Then they make recommendations for when and how often healthcare providers should offer them to their patients (Fadich, 2018).
For example, they recommend the age when you should start having cholesterol screenings or how often you should get a colonoscopy.
In a controversial 2004 decision, the USPSTF chose to stop supporting regular testicular self-exams. They made this recommendation because testicular cancer is highly treatable, even when caught later. They felt that it might result in too many false alarms and needless anxiety for men (Fadich, 2018).
Some cancer researchers have petitioned the USPSTF to change its recommendations. They argue that regular testicular self-exams can be used to (Rovito, 2018):
Increase early diagnosis of testicular cancer
Increase the diagnosis of other urinary and genital health conditions
Increase men’s knowledge about their health and body
Increase men’s comfort with discussing genital health concerns with providers
Since these exams aren’t officially recommended yet, there isn’t a standard guideline for who should perform them and how often. Some healthcare providers have suggested that all men perform a testicular self-exam once a month after puberty, similar to the recommendations for women and monthly breast self-exams.
Signs of testicular cancer
Once you learn how to check for testicular cancer, you should know the signs you are looking for. The most common sign of testicular cancer is a painless, pea-sized lump on your scrotum that’s found by either you during a self-exam or by a sex partner (Baird, 2018).
There’s a chance it may also be noticed when you have images or scans done for other health reasons or when you are examined for a different illness or injury in the groin area (Baird, 2018).
Some less common symptoms of testicular cancer that have been reported include (Baird, 2018):
Pain in your testes or scrotum
Dull ache in your scrotum or lower abdomen
Unusual firmness in your testicles
A feeling of heaviness in your scrotum
Swollen scrotum
Rarely, men with testicular cancer might have symptoms that may indicate cancer has spread to other areas of the body (Baird, 2018):
Nausea, vomiting, or diarrhea
Enlarged breasts
Headaches
Low back pain
Swollen lymph nodes
Lump in the neck
Respiratory symptoms
Infertility
There are a number of non-cancer illnesses that have symptoms similar to the ones listed above. So there’s no reason to jump to conclusions if you feel something off. However, it is important to find out the exact cause of what you’re experiencing. Your healthcare provider can rule out other illnesses and provide treatment for whatever diagnosis you might have (Baird, 2018).
When to see a healthcare provider
If you experience any of the following symptoms, you should contact your healthcare provider (Gaddam, 2021):
Pain
Swelling
Unusual lumps or masses
Rash
Not all of these are signs of testicular cancer, but they do indicate a possible health issue that needs medical attention.
For example, pain isn’t a common sign of testicular cancer, but it is a possible sign of testicular torsion. Testicular torsion is an emergency situation where the blood vessels flowing to your testicle are blocked. If you experience sudden, sharp pain, you should immediately go to an emergency department (Velasquez, 2021).
When you see a provider about the possibility of testicular cancer, they will ask questions about your general health and the symptoms that you’re having. Then they will perform a physical exam and an ultrasound scan of your testicle. Further tests might include blood tests, a biopsy, or a CT scan. You also might be referred to other specialties such as urology, oncology, or radiology to help make a diagnosis (Gaddam, 2021; Cedeno, 2021).
Many factors determine how successful cancer treatment will be. In general, the sooner you find out and start treatment, the more likely you are to have a good outcome. Even if you have more advanced testicular cancer, there are still treatment options that could cure you (Gaddam, 2021).
Testicular cancer is one of the most curable types of cancer. Up to 90% of cases can be cured, and the 5-year survival rate of men diagnosed with testicular cancer is over 95%. This is why it is so important to learn how to check for testicular cancer and practice regularly (Gaddam, 2021).
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Baird, D. C., Meyers, G. J., & Hu, J. S. (2018). Testicular cancer: diagnosis and treatment. American Family Physician, 97 (4), 261–268. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29671528/
Cedeno, J. D., Light, D. E., & Leslie, S. W. (2021). Testicular seminoma. [Updated Aug 12, 2021]. In: StatPearls [Internet]. Retrieved on Sep. 26, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK448137
Fadich, A., Giorgianni, S. J., Rovito, M. J., Pecchia, G. A., Bonhomme, J. J., Adams, et al. (2018). USPSTF testicular examination nomination-self-examinations and examinations in a clinical setting. American Journal Of Men's Health, 12 (5), 1510–1516. doi: 10.1177/1557988318768597. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6142159/
Gaddam, S. J. & Chesnut, G. T. (2021). Testicle cancer. [Updated Jul 25, 2021]. In: StatPearls [Internet]. Retrieved on Sep. 26, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK563159/
Rovito, M. J., Leone, J. E., & Cavayero, C. T. (2018). "Off-Label" Usage of Testicular Self-Examination (TSE): Benefits Beyond Cancer Detection. American Journal of Men's Health, 12 (3), 505–513. doi: 10.1177/1557988315584942. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5987946/
Velasquez, J., Boniface, M. P., & Mohseni, M. (2021). Acute scrotum Pain. [Updated Jul 18, 2021]. In: StatPearls [Internet]. Retrieved on Sep. 26, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK470335/












