Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Surgery can be scary or uncomfortable for a lot of people, but if you’re told you need a prostatectomy—prostate surgery that involves removing part or all of the prostate gland—you may experience an added element of discomfort. You will also likely have many questions to ask your doctor before or after surgery. A big one is: will I be able to have an erection and have sex after prostatectomy?
What to expect from prostate surgery
Before understanding how prostate surgery can affect your sex life, it’s important to understand how the procedure works. More formally known as a prostatectomy, prostate surgery involves removing part or all of the prostate gland.
A simple prostatectomy refers to taking out just the inner part of the prostate gland. This treatment is often used for an enlarged prostate (benign prostatic hyperplasia). A radical prostatectomy involves removing the entire prostate gland, and is typically reserved for treating prostate cancer.
Prostate removal of some form may be recommended if you’re experiencing any of the following (McVary, 2021; NIH, 2019):
Problems emptying your bladder (urinary retention)
Frequent urinary tract infections
Prostate bleeding
Bladder stones and prostate enlargement
Very slow urination
Kidney damage
Recovery following surgery
Depending on the type of prostate surgery you get, you’ll remain in the hospital for 2–4 days after the procedure. You will also leave surgery with a catheter in your bladder.
Your healthcare team will encourage you to move around to get blood circulating and teach you some physical exercises and breathing techniques to repeat every few hours. Full recovery takes about six weeks and most men can urinate normally once they’ve healed (NIH, 2019).
Can I have sex after prostate surgery?
Yes, but there may be some changes you’ll learn to adapt to.
Like all surgeries, a prostatectomy carries some potential risks and side effects, including blood clots, infection, and more. But the procedure can also affect your sex life, the most common issue being erectile dysfunction (ED), meaning you can't get or keep an erection that's hard enough for penetration.
After surgery, some men will lose the ability to produce semen. This occurs in men with prostate cancer following radical prostatectomy, which often includes the removal of another organ that makes semen (seminal vesicles). After this kind of surgery, a man will have a dry orgasm, which is a permanent change.
Recovery from prostate surgery and how it may impact sexual health looks different for every person. While some might find a dry orgasm less satisfying due to the lack of semen, others can adjust to their new baseline orgasm (ACS, 2020; NIH, 2019).
Erectile dysfunction and prostate surgery
ED is the most common sexual side effect of prostate surgery. Research has shown that up to 85% of men who’ve had the whole prostate removed (radical prostatectomy) have problems with erections after surgery (Emanu, 2016).
Why exactly does this happen? Tiny nerve bundles that are crucial for an erection run along the prostate’s side that control erections. In some cases, the surgeon may be able to use what’s called a nerve-sparing approach during the procedure to avoid injuring these nerves. But the nerve-sparing approach isn’t an option for those with cancer that has grown very close to these nerves. If all of these nerves have to be cut, you’ll no longer be able to have spontaneous erections. That said, some men are able to have erections again with the help of certain treatments, which we’ll get to a little later on.
If you only have nerves on one side of the prostate removed, you may still be able to get erections, but it’s less likely than if no nerves were cut. If you get erections again depends on a few factors, including age and your ability to get erections before surgery.
All men who’ve had a prostatectomy will experience some decrease in their ability to have normal erections, but younger men are more likely to regain function. But again, every person is different. If you are able to regain spontaneous erections, it will probably happen slowly—it can take anywhere from months to a few years (McCullough, 2005).
Penis rehab and ED treatments
A few treatment strategies may help you get erections following prostate surgery.
Doctors may recommend what’s known as penile rehabilitation, or penis rehab for short. Many health experts theorize that the sooner you’re able to get an erection after surgery, the more likely you can gain control of ED over time. Penis rehab would begin once the body has had a chance to heal, which is usually several weeks after the operation. It’s an ongoing process that can last up to two years, and trying to get regular erections to help keep the tissue in your penis healthy is part of the journey.
The goal of penile rehabilitation is to preserve erectile function as possible through medications or devices, which we’ll explore below. The success of penile rehabilitation depends on a lot of different factors, especially on the number of nerves that were removed or preserved (Albaugh, 2019).
ED medications
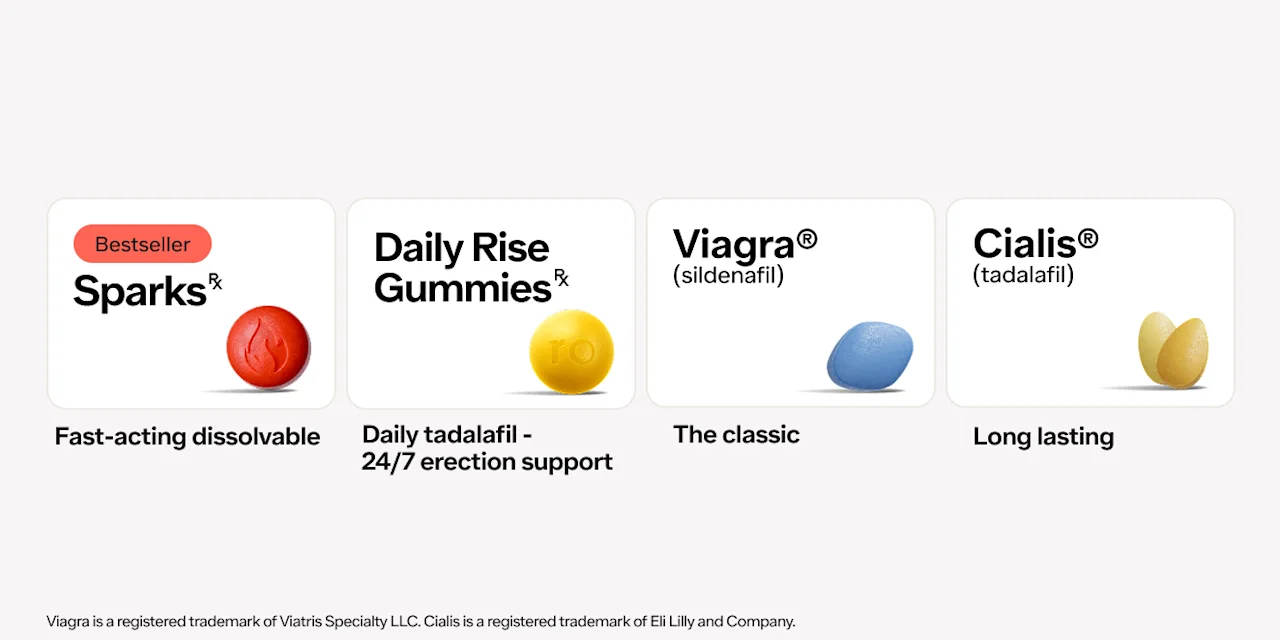
For some people, prescription drugs are recommended. Oral medications known as PDE5 inhibitors are common treatments for ED. The most common PDE5 inhibitor is sildenafil (brand name Viagra). Others include tadalafil (brand name Cialis), vardenafil (brand name Levitra), and avanafil (brand name Stendra) (Krzastek, 2019). These pills often don’t work well during the first few months after surgery, but at 18 months after surgery, the pills may be helpful in getting a firm erection (McCullough, 2005).
Medical devices
In some cases, a specific type of device may be helpful in restoring erections. Known as vacuum therapy or penis pumps, this treatment uses a vacuum pump to draw blood into the penis. Because a penis pump causes erections regardless of nerve damage, it can be an important tool to help restore erections (Hecht, 2016).
Lifestyle changes
Certain lifestyle modifications can also help with ED and support penile rehabilitation. Things like a lack of physical activity, obesity, an unhealthy diet, and cigarette smoking have all been shown to contribute to sexual dysfunction. Taking actions to modify these behaviors can improve symptoms of ED and benefit your overall health.
Health issues like diabetes, cardiovascular disease, high blood pressure, and certain mental disorders can also contribute to ED, so working with a health professional to manage these is always a good idea (Krzastek, 2019).
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Viagra Important Safety Information: Read more about serious warnings and safety info.
Cialis Important Safety Information: Read more about serious warnings and safety info.
References
ACS. (2019). How Cancer Can Affect Ejaculation. Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/fertility-and-sexual-side-effects/sexuality-for-men-with-cancer/ejaculation-and-treatment.html
ACS. (2019). Surgery for Prostate Cancer. Retrieved from cancer.org/cancer/prostate-cancer/treating/surgery.html
Albaugh, J., Adamic, B., Chang, C., Kirwen, N., & Aizen, J. (2019). Adherence and barriers to penile rehabilitation over 2 years following radical prostatectomy. BMC Urology , 19 (1). doi:10.1186/s12894-019-0516-y. Retrieved from https://bmcurol.biomedcentral.com/articles/10.1186/s12894-019-0516-y
Emanu, J. C., Avildsen, I. K., & Nelson, C. J. (2016). Erectile dysfunction after radical prostatectomy: prevalence, medical treatments, and psychosocial interventions. Current Opinion in Supportive and Palliative Care , 10 (1), 102–107. doi:10.1097/SPC.0000000000000195. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5005072/
Farag, Y. M., Guallar, E., Zhao, D., Kalyani, R. R., Blaha, M. J., Feldman, D. I., et al. (2016). Vitamin D deficiency is independently associated with greater prevalence of erectile dysfunction: The National Health and Nutrition Examination Survey (NHANES) 2001–2004. Atherosclerosis , 252, 61–67. doi:10.1016/j.atherosclerosis.2016.07.921. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5035618/
Hecht, S. L., & Hedges, J. C. (2016). Vacuum Therapy for Erectile Dysfunction. Contemporary Treatment of Erectile Dysfunction , 175–185. doi:10.1007/978-3-319-31587-4_13. Retrieved from https://link.springer.com/chapter/10.1007/978-3-319-31587-4_13
McVary, K. T. (2021). Surgical treatment of benign prostatic hyperplasia (BPH). UpToDate. Retrieved from https://www.uptodate.com/contents/surgical-treatment-of-benign-prostatic-hyperplasia-bph
Krzastek, S. C., Bopp, J., Smith, R. P., & Kovac, J. R. (2019). Recent advances in the understanding and management of erectile dysfunction. F1000Research , 8, F1000 Faculty Rev-102. doi:10.12688/f1000research.16576.1. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30740217/
McCullough A. R. (2005). Sexual dysfunction after radical prostatectomy. Reviews in Urology, 7 Suppl 2 (Suppl 2), S3–S10. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16985895/
National Institutes of Health (NIH). (2019). Simple prostatectomy. Retrieved from https://medlineplus.gov/ency/article/007416.htm