Here's what we'll cover
Here's what we'll cover
What is erectile dysfunction?
The term erectile dysfunction (ED) can have two different but related meanings. In a broad sense, erectile dysfunction is the inability to achieve or maintain an erection suitable for sexual intercourse (Sooriyamoorthy, 2020). The inability to achieve a satisfactory erection can have many causes, but healthcare providers officially call it ED when it isn’t caused by another underlying condition.
Erections are complex things involving multiple systems in your body. Your brain, blood vessels, and nerves all take part. Erections can arise in two different ways. They can be triggered mentally in response to things a person with a penis sees, hears, smells, or imagines. Or they can pop up reflexively after physical stimulation (Miller, 2000).
Whichever way it comes about, the body then goes through a series of reactions. Without going into all of them, as they get pretty complicated, the end result is that more blood flows into the penis while the outflow is reduced. The penis becomes rigid, and an erection is formed.
Anything that gets in the way of this workflow, between stimulation and erection, can cause ED. There can be physical or psychological causes, ranging from high blood pressure to performance anxiety and more.
Age is the most significant risk factor for ED. This is because testosterone generally decreases, and risks for other medical conditions that affect ED increase as we get older. Data suggests that over half of men between the ages of 40 and 70 have experienced ED (Feldman, 1994). Many lifestyle choices can increase this risk as well. Smoking, obesity, and the use of alcohol or illicit drugs all raise the odds of ED (Heidelbaugh, 2010).
Determining the cause of ED is very important, as it might signal a more significant health problem. It can be a symptom of a condition the patient may not know they have, such as cardiovascular disease (CVD) or diabetes mellitus, among many others (Salonia, 2013).
Other medical conditions that can cause ED include hypertension, hypogonadism (low testosterone), benign prostatic hyperplasia (enlarged prostate, also called BPH). In many cases, ED is simply the side effect of a medication. Some of the most commonly prescribed drugs in the United States list ED as a potential adverse effect (Sooriyamoorthy, 2020).
ED can have a physical or psychological basis. Studies have implied that ED and depression can each be contributing factors for the other. Men with depression are 39% times more likely to develop ED than those without, and men with ED are almost three times more likely to have depression (Liu, 2018).
Testing for erectile dysfunction
Because it could be a sign of a more serious medical condition, it’s important that you speak with a healthcare provider if you are experiencing any kind of sexual dysfunction. There are many tests available to help your healthcare provider diagnose ED and determine the root cause, if any. In many cases, it can be done without an in-person visit, such as online via telemedicine.
First, they’ll want to know your complete medical history to see if there’s an obvious reason, such as a medication you’ve been taking. Some common types of prescription drugs reported to cause ED are (MedlinePlus, n.d.):
Psychiatric medications, such as antidepressants
Antihistamines
High blood pressure medications, including thiazides, beta-blockers, and some alpha-blockers
Diuretics (“water pills”)
Parkinson’s disease medications
Hormonal medicines
Chemotherapy
Painkillers, especially opiates
Your provider will want to discuss your sexual history and sexual activity. Be honest with them about recreational drug use and habits such as smoking, which can affect ED. You’ll likely take a simple questionnaire called the International Index of Erectile Function (IIEF).
The five-question version (IIEF-5) asks you to rank a few erection-related issues. These include the frequency with which you’re able to get erections, the difficulty of maintaining them, and how often the erections were hard enough for penetration (Heidelbaugh, 2010). An extended, fifteen-question version (IIEF-15) goes deeper, asking for details such as frequency of ejaculation or orgasm, libido, and your relationship with your sexual partner (Miller, 2000).
At this point, in many cases, a diagnosis of ED can be made, and appropriate treatment can be prescribed. This might be a combination of medication and lifestyle changes, if necessary. If your provider suspects that your ED stems from another condition, or if the medications aren’t helping, they may wish to perform further tests to figure out the cause.
Some of these can also be done through telemedicine, such as screenings for possible mental health conditions like depression, anxiety, or stress. One way to test if ED is physical or psychological is nocturnal penile tumescence (NPT) monitoring. In plain English, that just means finding out if you get erections in your sleep.
While not 100% accurate, especially in patients who toss and turn a lot, your provider may ask you to do a common self-test called the stamp test. The process is simple: place a ribbon of stamps that are still connected by perforations around the base of the penis before bed, and seal them in a snug circle. If the ribbon is broken in the morning, it’s likely because you achieved an erection in your sleep. This would imply the cause is psychological, not physical (Keller, 2012).
In most cases, it’s only if the problem persists, or if they have reason to suspect a more severe underlying condition, that your provider would wish to schedule an in-person physical exam. AT this point, there are a number of tests that can help determine the cause. They’ll do a physical examination of your cardiovascular, neurologic, and genitourinary systems. They may also perform a urinalysis and blood tests, including (Heidelbaugh, 2010):
Fasting serum glucose level to test for diabetes
Lipid panel to test for high cholesterol, atherosclerosis, or heart disease.
Thyroid-stimulating hormone (TSH) test for thyroid disorders
Morning total testosterone level, to test for hypogonadism, aka low testosterone
Another test for physical causes is penile doppler ultrasound. Ultrasound works by sending sound waves into the body, which bounce off certain tissue types into a sensor. Your healthcare provider can get a look at your blood flow in action, allowing them to see whether the cause is vascular (relating to the blood vessels) (Varela, 2020).
Vascular-based ED is considered an early warning sign for future cardiovascular problems. A ten-year study found men with certain vascular abnormalities detected by ultrasound were three times likelier to have major adverse cardiovascular events (Caretta, 2019).
Treatment options
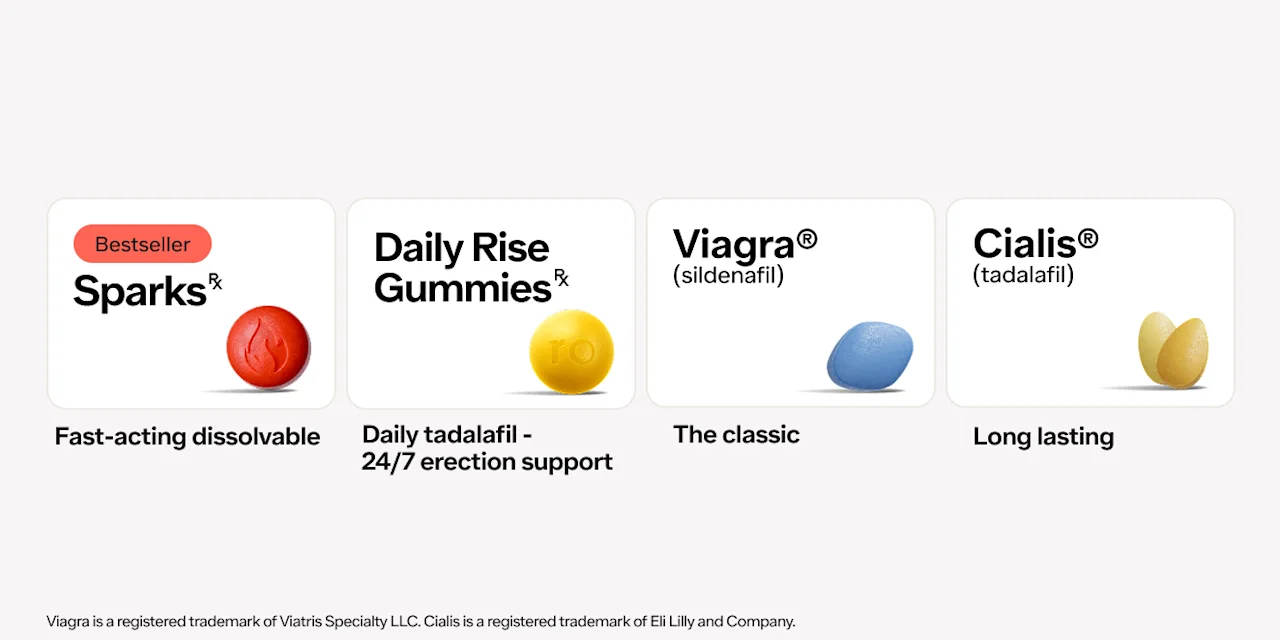
Luckily, ED is highly treatable. Typically, if there is no obvious underlying condition, the first step would involve medications called phosphodiesterase type 5 (PDE5) inhibitors (Rew, 2016). These include sildenafil (brand name Viagra), tadalafil (brand name Cialis), vardenafil (brand name Levitra), and avanafil (brand name Stendra). Lifestyle changes may also be suggested.
If an underlying condition is found, you treat that, and hopefully, the ED will go away. In some cases, PDE5 inhibitors may be prescribed as a stopgap measure while waiting for the underlying condition’s treatment to kick in.
There are further options for patients who do not respond to PDE5 inhibitors or cannot take them. One approach includes self-administered injections or suppositories placed into the urethra. These medications include alprostadil, bimix, or a combination of the two called trimix. In simple terms, they all work by encouraging the muscles to relax, thus allowing better blood flow into the penis. (Khera, 2011).
People who find injections or urethral suppositories uncomfortable may consider a vacuum constrictor device (VCD) instead. These work by “forcing” an erection, using a vacuum pump to pull blood into the penis before cutting off the outflow with an elastic ring placed around the base. And for those for whom none of the above work, a surgically implanted prosthesis may be the best solution (Rew, 2016).
Erectile dysfunction is a sensitive topic for many people. You may be reticent to approach your healthcare provider about it. If you’re of a certain age, they may broach the subject with you. Remember, it’s not just about what’s going on down there.
Your ability to get and maintain an erection connects to many other systems in your body. It could be a reflection of a very serious problem. But luckily, there are many simple tests that can be done to identify the cause of your ED and get you on a healthy path to feeling better.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Viagra Important Safety Information: Read more about serious warnings and safety info.
Cialis Important Safety Information: Read more about serious warnings and safety info.
Caretta, N., De Rocco Ponce, M., Minicuci, N., Palego, P., Valente, U., Garolla, A., Ferlin, A., & Foresta, C. (2019). Penile doppler ultrasound predicts cardiovascular events in men with erectile dysfunction. Andrology, 7 (1), 82–87. doi: 10.1111/andr.12561 Retrieved from https://pubmed.ncbi.nlm.nih.gov/30407754/
Feldman, H. A., Goldstein, I., Hatzichristou, D. G., Krane, R. J., & McKinlay, J. B. (1994). Impotence and Its Medical and Psychosocial Correlates: Results of the Massachusetts Male Aging Study. Journal of Urology, 151 (1), 54-61. doi:10.1016/s0022-5347(17)34871-1 Retrieved from https://pubmed.ncbi.nlm.nih.gov/8254833/
Heidelbaugh, J. J. (2010). Management of erectile dysfunction. American Family Physician, 81 (3), 305–312. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20112889/
Keller, L. M. M., Buyyounouski, M. K., Sopka, D., Ruth, K., Klayton, T., Pollack, A., Watkins-Bruner, D., Greenberg, R., Price, R., & Horwitz, E. M. (2012). Stamp test delivers message on erectile dysfunction after high-dose intensity-modulated radiotherapy for prostate cancer. Urology, 80 (2), 337–342. doi: 10.1016/j.urology.2012.04.048 Retrieved from https://pubmed.ncbi.nlm.nih.gov/22749428/
Khera, M., & Goldstein, I. (2011). Erectile dysfunction. BMJ Clinical Evidence, 2011,
Retrieved from https://pubmed.ncbi.nlm.nih.gov/21711956/
Liu, Q., Zhang, Y., Wang, J., Li, S., Cheng, Y., Guo, J., Tang, Y., Zeng, H., & Zhu, Z. (2018). Erectile dysfunction and depression: A systematic review and meta-analysis. The Journal of Sexual Medicine, 15 (8), 1073–1082. doi: 10.1016/j.jsxm.2018.05.016 Retrieved from https://pubmed.ncbi.nlm.nih.gov/29960891/
MedlinePlus (n.d.). Drugs that may cause erection problems. Retrieved 25 January 2020, from https://medlineplus.gov/ency/article/004024.htm
Miller, T. A. (2000). Diagnostic evaluation of erectile dysfunction. American Family Physician, 61 (1), 95–104, 109–110. Retrieved from https://pubmed.ncbi.nlm.nih.gov/10643952/
Pizzol, D., Demurtas, J., Stubbs, B., Soysal, P., Mason, C., Isik, A. T., Solmi, M., Smith, L., & Veronese, N. (2019). Relationship between cannabis use and erectile dysfunction: A systematic review and meta-analysis. American Journal of Men’s Health, 13 (6), 1557988319892464. doi: 10.1177/1557988319892464 Retrieved from https://pubmed.ncbi.nlm.nih.gov/31795801/
Rew, K. T., & Heidelbaugh, J. J. (2016). Erectile dysfunction. American Family Physician, 94 (10), 820–827 Retrieved from https://pubmed.ncbi.nlm.nih.gov/27929275/
Salonia, A., Capogrosso, P., Clementi, M. C., Castagna, G., Damiano, R., & Montorsi, F. (2013). Is erectile dysfunction a reliable indicator of general health status in men? Arab Journal of Urology, 11 (3), 203–211. doi: 10.1016/j.aju.2013.07.008 Retrieved from https://pubmed.ncbi.nlm.nih.gov/26558083/
Sooriyamoorthy, T., & Leslie, S. W. (2020). Erectile dysfunction. In StatPearls. StatPearls Publishing. Retrieved on Feb. 12, 2021 from https://pubmed.ncbi.nlm.nih.gov/32965924/