Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Whether you're actively trying to conceive or avoiding conception, we want you to have the info required to help you achieve your reproductive goals — whatever they may be. Read on to learn more about your chances of getting pregnant, and how those chances are affected by things like your cycle, age, previous and current birth control use, conditions like polycystic ovary syndrome (PCOS), and more.
What is conception?
Conception is a little more nuanced than the love story of egg meets sperm. Of course, the meeting of egg and sperm is a necessary prerequisite to a pregnancy, but it's a bit more complicated than that.
Biological women are born with all the eggs they’ll ever have (1–2 million) and have approximately 400,000 eggs left by the time puberty hits. However, almost all of these eggs are suspended in an undeveloped state and every month, you lose about 1,000 undeveloped eggs.
Around ovulation, an ovarian follicle releases one egg, which then travels from the ovary into the Fallopian tube on its way to the uterus. If any sperm were waiting around in the reproductive tract before ovulation occurred (they can survive in the female reproductive tract for up to ~5 days), or if sperm make their way into the reproductive tract and all the way to the egg within 24 hours of its release, fertilization can occur. If the egg is not fertilized, it exits the body during menstruation.
However, a fertilized egg (embryo) does not necessarily equal successful conception. Fertilized eggs travel to the uterus and implant in the uterine wall around 6–7 days after fertilization. From here, the embryo can continue developing into a successful pregnancy. Approximately 10–40% of fertilized eggs don’t make it to implantation.
Pregnancy and your cycle
Many people wonder about the chances of getting pregnant during their cycle. Can you still get pregnant after ovulation or while you're on your period? To answer these questions, let’s first review the menstrual cycle.
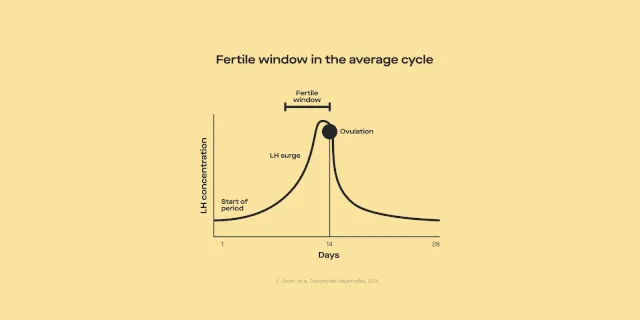
People who get their period regularly, and don't have any conditions (like PCOS) that influence ovulation, typically ovulate around the middle of their cycle (around day 14). You have the highest chance of getting pregnant around ovulation. Since sperm can live up to five days in the female reproductive tract, having sex on the days leading up to ovulation makes it likely that there will be some sperm waiting around for the egg once it's released. That being said, chances of conception get higher the closer you get to ovulation.
But can you get pregnant after ovulation or during your period? Outside the “fertile window” (i.e., the five days before ovulation and within 24 hours of ovulation), it is not physiologically possible to conceive if you have regular-length cycles and periods. This means that you can't get pregnant while on your period, nor can you get pregnant days after ovulation. Remember that not everyone ovulates on day 14, so your fertile window may be different.
How long, on average, does it take to conceive?
In a study of almost 3,000 US couples trying to conceive (TTC), 62% of women aged 28–30 and 28% of women aged 40–45 got pregnant within 6 months. The average across the entire study was 58%. Looking at a longer timeframe, 79% of women aged 25–27 and 56% of women aged 40–45 got pregnant within 12 months. The average across the entire study was 75%. This study did not use any specific methods to promote conception.
However, if you've been cycle tracking and timing intercourse, this next study might be more relevant. In this study, women between the ages of 20 and 44 were taught how to use natural family planning (e.g., monitoring cervical mucus and basal body temperature) when they started trying to conceive. Researchers found that 38% will conceive within one month of TTC, 68% within three months, 81% within six months, and 92% within 12 months. In summary, most couples conceive within 6 months of timed intercourse.
How does birth control impact the time it takes to conceive?
You may be concerned about whether being on birth control affects how long it takes you to conceive. A team of researchers looked into this question by doing a systematic review of the existing work on how different methods of birth control impacted the likelihood of getting pregnant within 12 months of TTC.
They found that over 83% of women who stopped non-barrier birth control methods (e.g., oral contraceptive pills, contraceptive implants or injections, and IUDs) became pregnant within 12 months of TTC. So overall, there is no significant delay in the return of your fertility after spotting these methods.
Is there a chance of conceiving if you're currently on birth control?
Chances are, if you're currently using birth control, you're not TTC — but how successful your birth control method is at preventing pregnancy differs significantly based on what you're using.
According to the Centers for Disease Control and Prevention (CDC), the least effective birth control method is spermicide — of couples who only use this method for a year, 21 out of 100 will experience an unintended pregnancy with typical use.
This number falls to 13 out of 100 over the course of a year for male condoms and further drops to 7 out of 100 for the pill, the patch, and the ring. While a 7 in 100 failure rate seems high for these hormone-based methods, it's important to remember that this rate takes into account user error. Because women don't always take the pill as directed or replace their patches and rings on schedule, failure rates for these methods are higher than they would be with perfect use.
Some birth control methods require less action on the part of women; for example, once you get an IUD, there's nothing you have to do, except for remembering to get it replaced every 3-10 years (depending on the type you get). These methods, called long-acting reversible contraceptives (LARCs for short), have failure rates of less than 1%. Other examples of LARCs include contraceptive implants or injections.
How does age affect the time to conceive?
Most people know that fertility decreases as you age. These changes in fertility are a function of both how many eggs we have left and how healthy those eggs are. Together, the changes in egg quality and quantity make it trickier to conceive as age goes up. Research shows that the time to pregnancy may differ among women of different ages.
For example, one study with almost 3,000 couples found that while 62% of women between 28 and 30 conceive within six cycles, this drops to 56% for women between 34 and 36, and 28% for women between 40 and 45. Even though the exact estimates differ across studies, one thing remains constant: Time to pregnancy tends to get longer as age goes up.
The main takeaway here? Your chances of conceiving on each day of your fertile window change as you age, and this may in part explain why time to pregnancy is longer among older people.
How do medical conditions impact your chances of getting pregnant?
Different medical conditions may impact how often you ovulate, how likely a fertilized egg is to implant, and how likely a pregnancy is to be carried to term.
PCOS and conception
PCOS affects anywhere from 5–20% of people with ovaries and is one of the leading culprits of infertility among couples seeking treatment at fertility clinics. In people with PCOS, ovulation is irregular and occurs less frequently. This means that people with PCOS ovulate infrequently (if at all), and ovulation doesn't always occur at predictable intervals. People with PCOS may be at increased risk of adverse pregnancy outcomes which means they may need additional visits with their doctor when trying to conceive and after conception has occurred.
Endometriosis and conception
Endometriosis is a condition characterized by the growth of uterus tissue outside of the uterus. It can cause excessive cramping, pressure, bloating, headaches, and bleeding. Somewhere between 6 and 10% of people with ovaries have endometriosis, and among those with infertility, up to 50% may have endometriosis (whether it be diagnosed or undiagnosed).
Thyroid dysfunction and reproductive health
When there are higher or lower levels of thyroid hormones, it can alter our reproductive hormones and disrupt the menstrual cycle — which makes conception trickier. But just because you have hypo- or hyperthyroidism doesn't mean you can't get pregnant. In one study of a group of almost 400 women suffering from infertility, 24% of participants were found to have hypothyroidism — but within a year of treatment, 76% were able to conceive.
If you have a diagnosed medical condition, talk to your healthcare provider before TTC. They will be able to give you crucial insight into how your diagnoses may impact your chances of conception (if at all), and suggest steps to help you maximize those chances.
How can you increase your chances of natural conception?
Because many factors influence your chances of conceiving, there are several different things you can do to tip the scales in your favor.
One thing you can do to boost your odds is to track your cycles and time intercourse or insemination around ovulation. After all, if you aren't having sex or inseminating during the fertile window, your chances of conception are zero. Because the chances of conception increase in the five days before ovulation and peak the day before ovulation, you should be having sex within this window if you're looking to conceive.
Certain lifestyle factors may also modulate how likely you are to conceive because they affect how regularly you ovulate, your egg quality, and your ovarian reserve. For example, having a very low or high BMI may contribute to infertility. Smoking is another factor that may make it harder to conceive. Studies show that smokers are 54% more likely to have trouble conceiving after 12 months of trying compared to nonsmokers.
There are so many factors that affect the likelihood of conception that sometimes it may seem like a miracle if it happens at all. While we can't control things like our age or diagnoses, there are steps you can take to boost your chances of getting pregnant: testing your fertility hormones to see whether underlying conditions like PCOS may be a factor affecting your fertility, using ovulation predictor kits or tracking cervical mucus to pinpoint ovulation (and timing intercourse accordingly), and embracing healthy habits.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Azziz, R. (2018). Polycystic ovary syndrome. Obstetrics and Gynecology, 132 (2), 321–336. doi:10.1097/AOG.0000000000002698. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29995717/
Bulletti, C., Coccia, M. E., Battistoni, S., & Borini, A. (2010). Endometriosis and infertility. Journal of Assisted Reproduction and Genetics, 27 (8), 441–447. doi:10.1007/s10815-010-9436-1. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941592/
Cena, H., Chiovato, L., & Nappi, R. E. (2020). Obesity, polycystic ovary syndrome, and infertility: a new avenue for GLP-1 receptor agonists. The Journal of Clinical Endocrinology and Metabolism, 105 (8), e2695–e2709. doi:10.1210/clinem/dgaa285. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32442310/
Centers for Disease Control and Prevention (CDC). (2023). Contraception. Retrieved from https://cdc.gov/reproductivehealth/contraception/index.htm
Cox, E. & Takov, V. (2022). Embryology, ovarian follicle development. StatPearls . Retrieved on Mar. 21, 2023 from https://www.ncbi.nlm.nih.gov/books/NBK532300/
Girum, T. & Wasie, A. (2018). Return of fertility after discontinuation of contraception: a systematic review and meta-analysis. Contraception and Reproductive Medicine, 3 , 9. doi:10.1186/s40834-018-0064-y. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6055351/
Gnoth, C., Godehardt, D., Godehardt, E., et al. (2003). Time to pregnancy: results of the German prospective study and impact on the management of infertility. Human Reproduction,18 (9),1959–1966. doi:10.1093/humrep/deg366. Retrieved from https://academic.oup.com/humrep/article/18/9/1959/708200
Jarvis, G. E. (2016). Early embryo mortality in natural human reproduction: What the data say. F1000Research, 5,
doi:10.12688/f1000research.8937.2. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5443340/
Kölle, S. (2022). Sperm-oviduct interactions: Key factors for sperm survival and maintenance of sperm fertilizing capacity. Andrology, 10 (5), 837–843. doi:10.1111/andr.13179. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35340118/
Oliver, R. & Basit, H. (2022). Embryology, fertilization. StatPearls . Retrieved on Mar. 29, 2023 from https://www.ncbi.nlm.nih.gov/books/NBK542186/
Practice Committee of the American Society for Reproductive Medicine. (2018). Smoking and infertility: a committee opinion. Fertility and Sterility, 110 (4), 611–618. doi:10.1016/j.fertnstert.2018.06.016. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30196946/
Roos, N., Kieler, H., Sahlin, L., et al. (2011). Risk of adverse pregnancy outcomes in women with polycystic ovary syndrome: population based cohort study. BMJ (Clinical research ed.), 343 , d6309. doi:10.1136/bmj.d6309. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21998337/
Stanford, J. B., White, G. L., & Hatasaka, H. (2002). Timing intercourse to achieve pregnancy: current evidence. Obstetrics and Gynecology, 100 (6), 1333–1341. doi:10.1016/s0029-7844(02)02382-7. Retrieved from https://pubmed.ncbi.nlm.nih.gov/12468181/
Verma, I., Sood, R., Juneja, S., & Kaur, S. (2012). Prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility. International Journal of Applied & Basic Medical Research, 2 (1), 17–19. doi:10.4103/2229-516X.96795. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3657979/
Wesselink, A. K., Rothman, K. J., Hatch, E. E., et al. (2017). Age and fecundability in a North American preconception cohort study. American Journal of Obstetrics and Gynecology, 217 (6), 667.e1–667.e8. doi:10.1016/j.ajog.2017.09.002. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28917614/