Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
If you’re trying to become pregnant, anything less than immediate success can be super stressful. After just a month or two, you may be tempted to get a fertility test.
Before you take that step, understand that many couples don’t become pregnant right away. If you’re a woman and younger than 35, experts typically won’t recommend fertility testing until you’ve been trying to become pregnant for at least a year. If you’re 35 or older, that time threshold drops to six months due to a higher risk of infertility in this age group (ACOG, 2020).
If you do decide that you’d like to have a fertility test done, you have options. You can either test your fertility at home or reach out to a healthcare provider who can look at your and your partner’s fertility using several methods—including semen analyses designed to identify male infertility issues, such as low sperm count (Walker, 2021).
But male fertility testing is another topic altogether. Here, you’ll find information about fertility testing options for women.
How to test your fertility
You may assume that the first step in the process is some kind of fluid or blood test—either at home, at a doctor’s office, or a fertility clinic. But before ordering this kind of test, many fertility specialists begin with a simple menstrual cycle assessment.
If a woman has regular and predictable cycles of menstrual flow (bleeding) and other ovulation symptoms—such as bloating, fatigue, and breast tenderness—these are signs that her ovaries are functioning properly. In some cases, your healthcare provider may want to review your family and medical history and perform a physical exam. These steps can reveal problems or obstacles—many of which are correctable—that are preventing you from becoming pregnant.
For example, issues related to past sexually transmitted infections like chlamydia could be at play. So could your exercise habits, drug or alcohol use, or smoking history. Internal irregularities, like endometriosis or polycystic ovarian syndrome (PCOS), could also be factors (Walker, 2021).
Long story short, a complete medical “workup” could reveal barriers to fertility that test results miss. But if you’ve had a workup—or if you’re not interested in anything that intense—there are several testing options at your disposal.
Types of fertility tests
There are multiple tests that medical providers can perform to check your fertility. Some of these can also help you figure out the optimal time you should try to get pregnant.
Ovulation testing
Many women are familiar with fertility strips. These urine-based testing strips can identify when your luteinizing hormone (LH) is high. This information is useful because this mid-cycle surge is the best time to try to conceive. These tests can also help healthcare practitioners assess whether you're ovulating.
Along with these LH strips, blood tests can reveal your progesterone levels. If these levels are high, this also suggests you’re ovulating.
And if these tests indicate that normal and healthy ovulation is happening, your medical provider may turn to ovarian reserve tests, which check to see if your ovaries are able to release a mature egg that can be fertilized. These are done by testing your AMH or FSH levels (Walker, 2021).
Anti-Mullerian hormone (AMH) levels
One ovarian reserve test is a blood test that looks at a woman’s anti-mullerian or AMH levels. If a woman has low AMH levels, this can be a sign of fertility problems related to her ovaries (Walker, 2021).
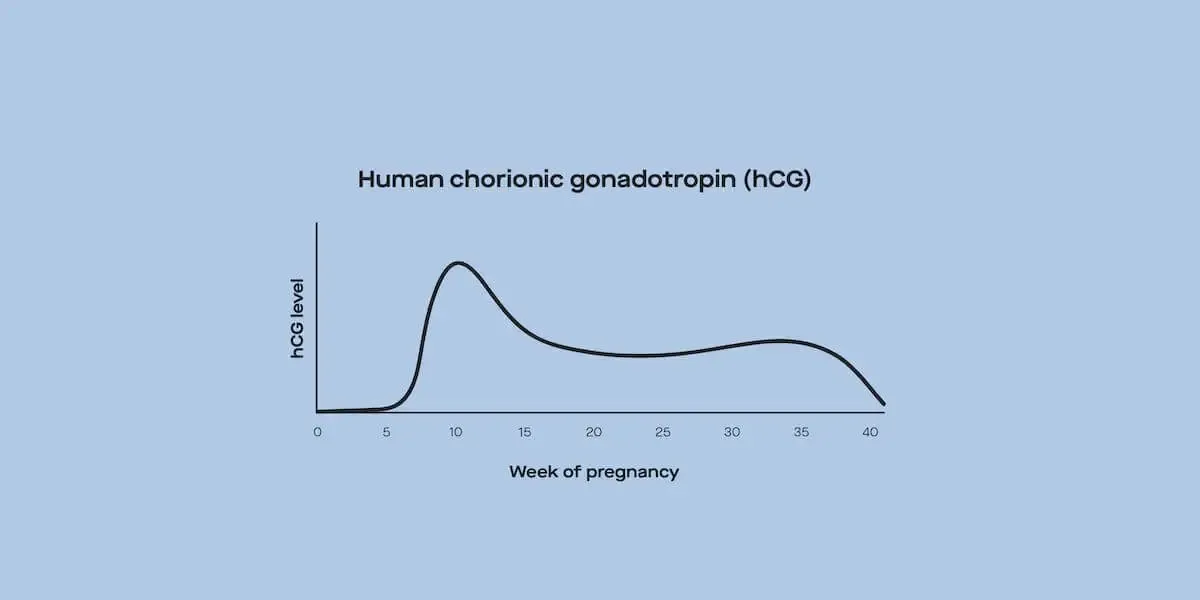
Anti-Mullerian hormone (AMH) is released by the ovarian follicles—tiny fluid-filled sacs in your ovaries that contain immature eggs called oocytes (Richards, 2010). Its levels are closely related to the healthy functioning of these follicles and their ability to produce mature eggs. AMH tends to steadily decline as a woman ages, and by the time of menopause, it’s almost undetectable (Wang, 2018).
Follicle-stimulating hormone test
Follicle-stimulating hormone (FSH) encourages the growth of follicles in the ovaries until an egg is released for fertilization. This release is usually referred to as ovulation. The FSH blood test checks the levels of this hormone and another hormone called estradiol that can indicate fertility problems even if FSH levels are normal.
You might assume that a higher level of FSH is better. But the opposite is true. High levels of FSH—which is usually measured on Day 3 of a woman’s cycle—suggest that the ovarian follicles may not have released a mature egg for fertilization (Walker, 2021).
While FSH evaluation is a common fertility test, some research has found that it may not be as helpful as AMH testing when it comes to identifying infertility (Wang, 2018).
At-home fertility tests
Along with the urine-based daily strips that look at luteinizing hormone levels, multiple companies now offer at-home fertility tests for women. These tests vary slightly from one to the next, but most rely on mail-in blood samples collected from a simple finger prick.
These tests tend to examine many of the same hormone markers that medical professionals would look at if you had the tests done in a clinic or doctor’s office—including FSH and AMH levels. Estradiol, prolactin, and thyroid hormones are also often part of the at-home tests. Research by one at-home test provider found that these finger-prick tests are just as accurate as those involving blood drawn from a vein (Burke, 2019).
Most of these tests cost between $125 and $200. Some may be paid for with health savings accounts, but most are not covered by insurance. And while some of these at-home testing services offer support features, such as access to physician consultations, they provide only a small part of the more-complete fertility assessment offered by medical clinics, which we’ll cover below.
Other fertility tests for women
If your medical provider suspects that problems related to your uterus or fallopian tubes (tubes that transport eggs from the ovaries to the uterus) may be the cause of your fertility issues, there are some specialized procedures that can help them confirm this suspicion, including a tubal evaluation and a uterine cavity exam.
Tubal evaluation
Endometriosis and other health conditions can affect the proper functioning of the fallopian tubes. Several tests, including some that rely on laparoscopy (a minimally-invasive procedure that uses a tiny camera to look inside of your body), can help a medical professional identify fertility-related issues (Walker, 2021).
Hysterosalpingography is another type of test that can help experts evaluate the health of your fallopian tubes, as well as your uterus. It’s a kind of X-ray procedure that involves water- or oil-based contrast dyes that are pushed through the fallopian tubes to check for any blockages.
While hysterosalpingography was first intended as a way to get a better look at a woman’s reproductive system, some research has found that the procedure—by flushing out the uterine cavity—may actually improve pregnancy odds because it can help remove some blockages caused by things like mucus (Dreyer, 2017).
Uterine cavity exam
If a healthcare provider suspects that issues related to the uterus are causing a woman’s fertility problems, a special type of sonogram exam—known as a saline infusion sonogram—can help identify abnormalities inside the uterus (Walker, 2021).
There are many other fertility-related procedures or prognostics that your healthcare provider may deem necessary. But the ones above are some of the most common.
Fertility results explained
If you’re having a hard time getting pregnant, it can be disheartening. And, as you can see, there are many reasons why you may be having a difficult time conceiving. While fertility tests can provide some helpful information, that information—by itself—won’t tell you much about how best to proceed.
In most cases, you’ll need a medical expert to assess your results and help you figure out the best path forward. While at-home testing companies offer access to MDs and other helpful consultants, you may ultimately need to meet with a fertility specialist to get to the bottom of any ongoing fertility challenges.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
American College of Obstetricians and Gynecologists (ACOG). (2020). Retrieved Dec. 22, 2021 from https://www.acog.org/womens-health/faqs/evaluating-infertility
Dreyer, K., van Rijswijk, J., Mijatovic, V., Goddijn, M., Verhoeve, H. R., van Rooij, I., et al. (2017). Oil-Based or Water-Based Contrast for Hysterosalpingography in Infertile Women. The New England Journal of Medicine , 376 (21), 2043–2052. doi: 10.1056/NEJMoa1612337. Retrieved from https://www.nejm.org/doi/full/10.1056/nejmoa1612337
Hunt, S. & Vollenhoven, B. (2020). Assessment of female fertility in the general practice setting. Australian Journal of General Practice , 49 (6), 304–308. doi: 10.31128/AJGP-01-20-5205. Retrieved from https://www1.racgp.org.au/ajgp/2020/june/female-fertility-in-general-practice-setting
Walker, M. H. & Tobler, K. J. (2021). Female Infertility. [Updated Jan 1, 2021]. In: StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK556033/
Wang, S., Zhang, Y., Mensah, V., Huber, W. J., 3rd, Huang, Y. T., & Alvero, R. (2018). Discordant anti-müllerian hormone (AMH) and follicle stimulating hormone (FSH) among women undergoing in vitro fertilization (IVF): which one is the better predictor for live birth?. Journal of Ovarian Research , 11 (1), 60. doi: 10.1186/s13048-018-0430-z. Retrieved from https://link.springer.com/article/10.1186/s13048-018-0430-z