Here's what we'll cover
Here's what we'll cover
Have you ever felt a burning sensation or tightness in your chest? You may have wondered what it is and if you should go to a healthcare provider or treat it at home.
Acid reflux has certain symptoms in common with other digestive and heart-related issues. Learn how to tell the difference between them and which treatments work best.
Why does acid reflux happen?
Acid reflux is a common condition affecting about 20% of the population. Acid reflux affects your digestive tract and happens when stomach acid regurgitates or flows back up to your esophagus or food pipe (Antunes, 2021).
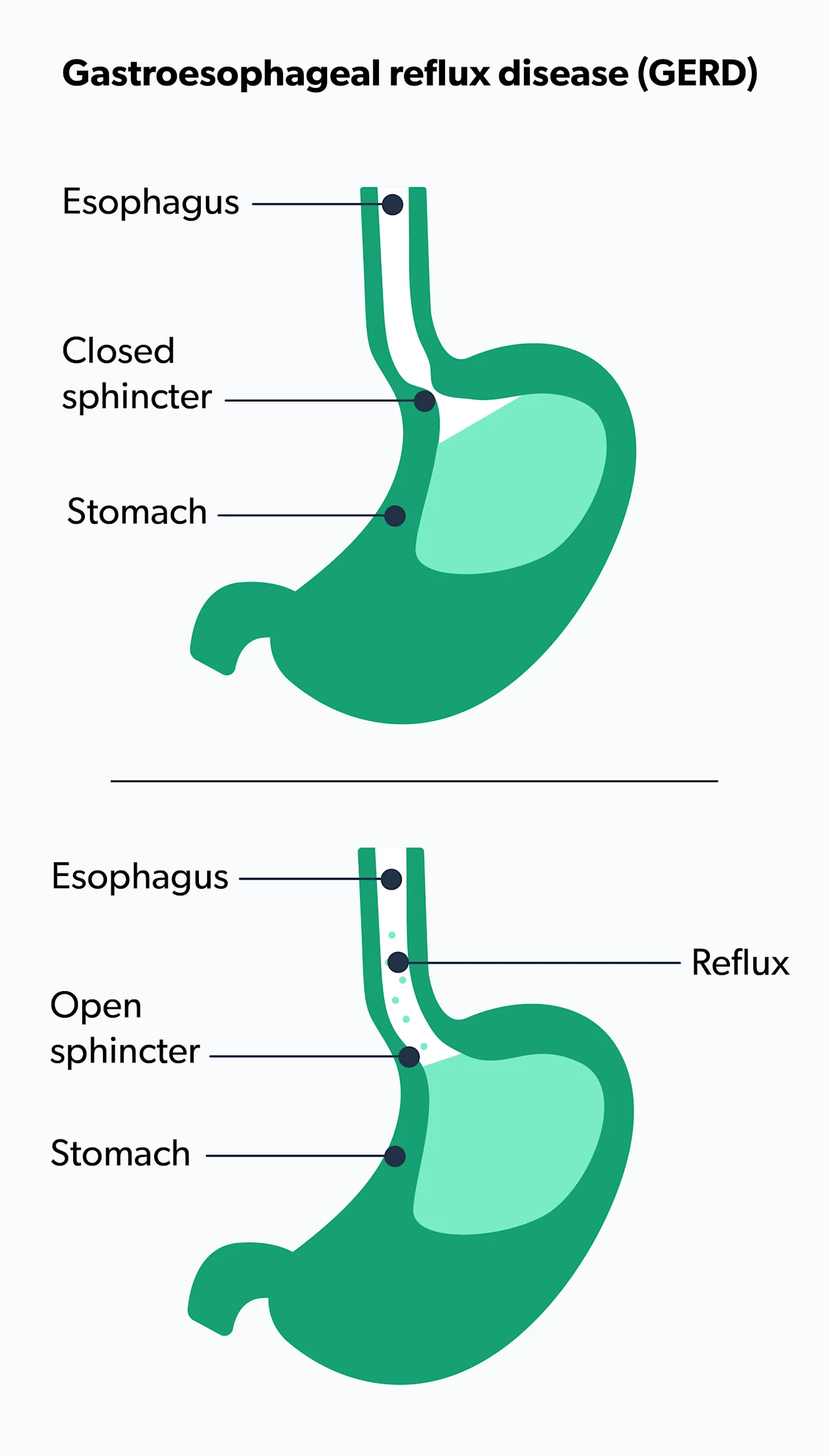
When you first put food in your mouth and chew it, it passes down to the stomach through the esophagus. At the very end of the esophagus, at the connection to the stomach, is a muscle called the lower esophageal sphincter (LES).
Your stomach is protected from its own acid production with specialized cells and mucus inside the stomach. The LES keeps your stomach contents away from the thinner lining of the esophagus. Weakness or pressure in or on the LES allows the stomach acid to regurgitate or flow back up. Regurgitation causes indigestion, heartburn, and acid reflux (Antunes, 2021).
Almost everyone gets indigestion or heartburn occasionally. However, if you have heartburn more than twice a week, you may have gastroesophageal reflux disease (GERD). Its name reflects gastro (stomach) and esophageal (food pipe) with reflux for the acid regurgitation. The word disease indicates it's a specific physical condition affecting the body (Hachem, 2016).
There are different types of GERD, and they have various symptoms (MacFarlane, 2018):
Erosive esophagitis (EE)—Some gastroenterologists may call this erosive reflux disease (ERD). EE occurs when the lining of the esophagus is damaged (eroded).
Non-erosive reflux disease (NERD)—This is when the reflux or regurgitation doesn’t damage the esophagus lining, but there are other symptoms of GERD.
What are the symptoms of GERD?
Two of the most common symptoms of acid reflux and GERD are heartburn and regurgitation.
Heartburn is a burning feeling in your chest behind the breastbone. It usually happens after a large, spicy, or fatty meal. Although it can happen at any time, heartburn is usually worse when lying down or at night. This occurs because lying flat makes it easier for the acid to wash up from your stomach into the esophagus (Antunes, 2021).
People with GERD may have heartburn that gets so bad at night that it may wake them from their sleep. GERD with heartburn may cause physical discomfort, interfere with your productivity, and decrease your quality of life.
The second most common symptom of acid reflux and GERD is regurgitation. Regurgitation is when the food or drink you swallowed moves back up the throat. Some people get nauseous from regurgitation. Babies and young children diagnosed with GERD usually have repeated regurgitation or “spitting up.” In babies under 18 months old, this is common and not usually a cause for concern unless the baby is in pain. It is estimated that half of all babies have reflux in their first few months of life. Adults rarely vomit from regurgitation (Poddar, 2018).
Some people may have GERD without heartburn. Other symptoms that may be GERD include (Richter, 2018):
Excess saliva, backwash, water brash, and nausea
Your body may react to the regurgitation and irritation of the acid reflux with extra saliva to try to flush it away.
You may experience a sour taste in your mouth from the strong acid regurgitating in your esophagus rising towards the back of your throat (backwash). When the acid reflux mixes with excess saliva, it is called water brash, which can cause a constant sour taste in your mouth.
It can also cause you to have bad breath even if you have excellent oral hygiene. Some people develop dental problems from constant acid reflux, including gum disease and discolored teeth from enamel erosion (Richter, 2018).
For some people, regurgitation can stimulate their gag reflex and make them nauseous. Others may feel nauseous from the constant sour taste.
Sore throat
Some people with GERD may have a sore throat from the constant regurgitation of irritating stomach acid. The acid reflux may also cause hoarseness or the feeling of a constant lump in your throat.
Dry cough
Acid reflux or regurgitation can trigger the nerves in the lower throat, causing you to cough to alleviate the irritation. Almost 30 percent of all people with chronic cough have GERD. If you have a constant dry cough that happens after eating or at night, and you don’t smoke, have asthma, or a constant post-nasal drip, you may have GERD even if you don’t have heartburn (Richter, 2018).
Dyspepsia or upset stomach
Dyspepsia can also be called indigestion or an upset stomach. Dyspepsia is when there is discomfort in your upper stomach with heartburn, nausea, and bloating. You may feel uncomfortably full even if you haven’t eaten a large meal. You may burp a lot or even throw up. If you keep having symptoms of dyspepsia, please seek medical advice. Persistent dyspepsia can be a symptom of stomach and digestive tract ulcers (Richter, 2018).
Dysphagia or difficulty swallowing
Some people with GERD have difficulty swallowing food or liquid, a condition called dysphagia. This is more common in older adults. If you develop this symptom, please see your healthcare provider.
Although dysphagia is sometimes seen in people with GERD, severe conditions can also cause this problem and require professional medical attention. These include esophageal stricture (narrowing of the esophagus), esophageal cancer, or neurological conditions like Parkinson's, multiple sclerosis, or a stroke.
Asthma and respiratory problems
Some people with GERD may have respiratory problems. Acid reflux can cause the muscles lining the airways of your lungs to spasm, leading to wheezing and shortness of breath. People with GERD and asthma may find their asthma gets worse when they have reflux symptoms. In general, however, respiratory issues are not a common symptom of GERD, so please seek medical attention immediately if you are short of breath.
Emergency GERD symptoms
Go to the emergency room immediately if you have:
Intense and severe chest pain
Chest pain radiating to your shoulder, jaw, neck, or back
Heartburn much worse than before
These may be symptoms of a heart attack.
Other symptoms that may seem like GERD can be caused by severe conditions instead. If you vomit up bloody or black material that looks like coarse ground coffee, or if your stools are very dark or tarry, go to the nearest emergency room.
What are risk factors for GERD?
There are multiple risk factors for GERD. People with obesity, a hiatal hernia, or pregnant people are more at risk for developing GERD. These people are at higher risk because they have high levels of pressure in their abdomen. People with diabetes are also at risk due to diabetic neuropathy or nerve damage affecting the LES muscle (Boeckxstaens, 2015).
The way you live your life can also increase your GERD risk. Here are some lifestyle factors that increase your risk of GERD (Richter, 2018):
Smoking tobacco products
Taking over-the-counter non-steroidal anti-inflammatory drugs (such as Advil or Motrin)
Eating large meals
Eating spicy foods or anything deep-fried or fatty
Drinking alcohol, coffee, and carbonated drinks
How do you diagnose GERD?
Your primary care healthcare professional may make the initial diagnosis and begin treatment. If there is concern for inflammation of the esophagus, or if there is a need to rule out other conditions, your healthcare provider may refer you to a gastroenterologist. They may do one of these tests to see if you have GERD or any complications (Koch, 2016):
X-ray imaging
A standard x-ray test used in diagnosing gastrointestinal issues is called an upper GI series. You'll take a barium swallow (a chalk-like drink) or barium pill to take before the test. Barium helps the radiologist visualize the upper part of your digestive system, including the esophagus, stomach, and part of your small intestine.
Endoscopy
Under sedation, the gastroenterologist threads a thin, flexible tube with a camera and light down your esophagus. They're looking for inflammation and strictures and may take a biopsy to diagnose Barrett's esophagus or esophageal cancer.
Esophageal manometry
A flexible thin tube is threaded into your esophagus to check how well your esophageal muscles work when you swallow by measuring their coordination, force, and rhythm.
Esophageal pH monitoring
A thin, flexible, wearable monitor (sometimes called a catheter) is placed in your nose down to your esophagus for 24 hours to measure how and when stomach acid regurgitates.
Your gastroenterologist and radiologist will let you know your diagnosis after your test. Some GERD cases are severe and may require surgery.
GERD Complications
Most people with GERD have mild to moderate symptoms. A few may have more severe issues. If you have heartburn for an extended period, you may be at greater risk for GERD complications.
These include esophagitis or inflammation of the esophagus and strictures or a narrowing of the esophagus where it is difficult to swallow. More serious conditions include a precancerous condition called Barrett's esophagus, where there is permanent damage to the esophagus lining. Some people with Barrett's esophagus develop esophageal cancer (Khieu, 2020).
It's essential to take steps to prevent and treat GERD symptoms, lowering your chances of complications.
What can you do if you have GERD or GERD-like symptoms?
You can relieve some of the symptoms by adjusting your diet and certain habits. You may also take over-the-counter medications found at any drug store or mass retailer. Many people usually start with antacids like Alka-Seltzer, Mylanta, or Tums. Stronger medications include histamine H2 receptor blockers like Pepcid or Tagamet. Other GERD medications include proton pump inhibitors (PPIs) like Prevacid or Prilosec. PPIs are usually taken for 14 days. These medications are also available in a stronger prescription strength if needed (MacFarlane, 2018).
The symptoms of GERD can be uncomfortable. Once you know what causes your symptoms and incorporate dietary and lifestyle changes or seek medical guidance on which medications you may need, you may be able to control or even completely relieve your symptoms.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Antunes, C., Aleem, A., & Curtis, S. A. (2020). Gastroesophageal reflux disease. StatPearls [Internet]. Retrieved from: https://www.statpearls.com/ArticleLibrary/viewarticle/22098
Boeckxstaens, G., El-Serag, H. B., Smout, A. J., & Kahrilas, P. J. (2015). Republished: Symptomatic reflux disease: the present, the past and the future. Postgraduate medical journal, 91 (1071), 46-54. Retrieved from: https://pmj.bmj.com/content/91/1071/46.short
Hachem, C., & Shaheen, N. J. (2016). Diagnosis and management of functional heartburn. American Journal of Gastroenterology, 111 (1), 53-61. doi: 10.1038/ajg.2015.376. Retrieved from: https://journals.lww.com/ajg/Abstract/2016/01000/Diagnosis_and_Management_of_Functional_Heartburn.20.aspx
Khieu, M., Mukherjee, S. (2020). Barrett esophagus. StatPearls [Internet]. Retrieved from: https://www.statpearls.com/ArticleLibrary/viewarticle/18143
Koch, O.O., Antoniou, S.A. Advances in diagnosing GERD. European Surgery; 48 , 203–208 (2016). doi: 10.1007/s10353-016-0435-z. Retrieved from: https://link.springer.com/article/10.1007/s10353-016-0435-z
MacFarlane B. (2018). Management of gastroesophageal reflux disease in adults: a pharmacist's perspective. Integrated pharmacy research & practice, 7 , 41–52. doi: 10.2147/IPRP.S142932. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5993040/
Poddar, U. (2019). Gastroesophageal reflux disease (GERD) in children. Paediatrics and international child health, 39 (1), 7-12. doi: 10.1080/20469047.2018.1489649. Retrieved from: https://www.tandfonline.com/doi/abs/10.1080/20469047.2018.1489649
Richter JE, Rubenstein JH. (2018). Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology;154 (2):267-276. doi: 10.1053/j.gastro.2017.07.045. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5797499/












