Here's what we'll cover
Here's what we'll cover
Before we dig deep into everything AMH, you might be wondering why you keep seeing those three letters pop up all over the Modern Fertility site — and increasingly, in women’s health articles and fertility conversations.
Anti-Mullerian hormone, or AMH, is one of the most important hormones related to fertility. So, we wanted to take a step back and compile all of the AMH info you need, all in one place.
Here’s a quick snapshot of what you’ll learn:
AMH is one of the most important hormones related to fertility because it serves as a proxy for your ovarian reserve (aka how many eggs you have).
Your AMH level will not tell you whether or not you’re fertile, but it can give you a better understanding of your reproductive health and help you plan ahead in many ways.
Your levels of AMH change over time, which is why tracking them is key.
Jump to any of the sections below
Overview of anti-Mullerian hormone (AMH)
Anti-Mullerian hormone (AMH) is one of the best indicators of the number of eggs in your ovaries, or your ovarian reserve. AMH is produced by granulosa cells in your ovarian follicles — meaning the tiny sacs in your ovaries that house and release eggs.
While your AMH level isn’t a crystal ball into your fertility future — meaning it is not a predictor of your ability to conceive today or at a certain time in the future — it does give you more info about your reproductive health: an understanding of your ovarian reserve, egg freezing or in-vitro fertilization (IVF) outcomes, menopause timing, and conditions like polycystic ovary syndrome (PCOS) and premature ovarian insufficiency (POI). Understanding your AMH level can help inform your timeline for getting pregnant and can fuel conversations with your doctor.
It bears repeating: No hormone test, including an AMH test, can guarantee pregnancy or confirm infertility. Think of it like a cholesterol test. While knowing your cholesterol level can’t tell you whether or not you’ll have a heart attack, it’s something you monitor over time and can be a catalyst for making small health or life changes. It can also help inform a convo with your doctor.
Additional reading:
Why AMH is a reliable marker of ovarian reserve — and what it can tell you
Studies have shown that AMH is the best and most reliable way to measure ovarian reserve, even for women who haven’t yet experienced infertility. Why? AMH is produced by the preantral and antral follicles in ovaries in women who are undergoing fertility treatments as well as women who aren’t. It’s just part of our biology, so it can tell us a lot about the female reproductive system. Preantral and antral follicles are the developing follicles in your ovaries — in other words, they correlate with the number of eggs available for ovulation.
Why does understanding our ovarian reserve matter? Women with lower levels of AMH for their age are likely to have a shorter reproductive window than women with normal levels of AMH for their age.
According to Prof. Scott Nelson, who’s considered one of the leading experts on AMH (and who’s also part of the Modern Fertility Medical Advisory Board), “It’s well-established in the medical community that women with a low ovarian reserve have a shorter reproductive life-span and earlier age of menopause. When women enter the menopause at an earlier age, it impacts their total fertility across their lifespan and potentially their ability to complete their desired family size.”
As couples delay starting a family, more and more women are trying to have kids just as their reproductive window is about to close. The average age of menopause is 51, but about 4-8 years before menopause — sometimes even up to 10 years before! — fertility starts to drop, making it harder to get pregnant. This is known as perimenopause. Understanding the importance of ovarian reserve and knowing your AMH can give you more information and help you make choices about your reproductive goals and timelines ahead of this.
It only takes one healthy egg (and one healthy sperm!) to make a baby, so low ovarian reserve doesn’t necessarily mean you won’t be able to get pregnant. But it is helpful to know how AMH impacts the female reproductive system, and why your reproductive years might be shorter than you realized.
AMH beyond ovarian reserve
Knowing your AMH level (usually measured in nanograms/milliliter or picomole/liter) is useful in many other ways. Here’s a summary of what AMH can help you understand:
If you may hit menopause earlier or later than average. Your mom's age at menopause onset used to be the gold standard for predicting when you may hit menopause. But AMH is proving to be useful as well — that’s because menopause is characterized by a near depletion of ovarian reserve, which AMH levels can indicate. (In fact, a recent 2020 study shows that AMH levels could one day help doctors predict your final period.)
Egg freezing or in-vitro fertilization (IVF) outcomes. AMH can help you understand how many eggs may be extracted during egg retrieval for egg freezing and IVF.
If you're at risk for polycystic ovary syndrome (PCOS). PCOS is very common and affects 1 in 10 women. It may be marked by high levels of AMH in your test results, which can mean that you have a high number of eggs but that you ovulate irregularly or infrequently (which can create challenges with conceiving).
If you're at risk for primary ovarian insufficiency (POI). POI is the loss of ovarian function before age 40, and impacts 1 in 100 women. It’s marked by extremely low or undetectable AMH levels in your test results.
We'll get into these a bit more in the sections below.
Why AMH is a hot topic in the medical community
Over the past decade, the medical community has been studying AMH. With every study, we get one step closer to better understanding the role that AMH plays in fertility and female reproductive health — but since the research is ongoing, the medical community’s opinion of AMH can shift.
For example, in 2015, the American Society for Reproductive Medicine (ASRM) came out with a statement saying, “There is mounting evidence to support the use of AMH as a screening test for poor ovarian response, but more data are needed." Four years later they updated their stance on AMH as a marker for ovarian reserve and outcomes in egg freezing and IVF: "The ability of AMH and antral follicle count to predict oocyte yield as well as poor and excessive ovarian responsiveness in IVF has been well demonstrated."
In early 2019, the American College of Obstetricians and Gynecologists (ACOG) released an opinion stating that while data supports using AMH tests with women experiencing infertility, it does not support women who are not infertile yet. The opinion does note that AMH is the most reliable marker for ovarian reserve.
We agree that there is not enough evidence that a single AMH measurement can predict time to pregnancy. There is no one test you can take to predict the ability to get pregnant right now, and to imply otherwise is misleading and irresponsible.
We believe that women want more than the answer to “can I get pregnant right now?” and can handle the nuances of what hormones can (and can’t) tell us about our fertility. Women are interested in understanding how their AMH level may reflect their ovarian reserve, menopause timing, potential success in egg freezing and IVF, and conditions like PCOS. Studies show that AMH is correlated with all of these factors. We’ll cite them throughout the rest of this guide.
Our healthcare system is generally set up to address infertility reactively. We believe all women deserve this information about their bodies at an affordable price. How we measure AMH has changed over time, and we believe more studies on the longitudinal decline of AMH and fertility outcomes (such as time to pregnancy, miscarriage, and live birth) in a presumed fertile population are needed. More research will certainly help address and resolve these differing viewpoints.
How anti-Mullerian hormone levels change over time
There are natural, small fluctuations in AMH throughout your cycle. Your level may be slightly higher right after your period (before ovulation), and slightly lower after ovulation (prior to your period, once an egg is released).
This isn’t unusual — many hormones fluctuate throughout your cycle. It’s worth noting that AMH has proven to be among one of the more consistent markers of ovarian reserve across the menstrual cycle, making it particularly useful. In fact, AMH fluctuates less than other reproductive hormones.
As you get older, AMH also declines (reflecting the decrease in ovarian reserve with age). Here’s what you should know about your AMH over the years:
We’re born with 1-2 million eggs — that’s enough to populate the entire city of Dallas, TX!
More than half our eggs disintegrate by the time we go through puberty (sounds alarming, but this is normal).
800-1,000 eggs undergo natural cell death each month — but only one makes it to the finish line (ovulation). If it’s fertilized, it may result in a pregnancy — if not, you’ll get a period. This happens every month, although if you’re on hormonal birth control (like the pill), you may not be ovulating or getting a period.
AMH generally peaks at age 25, and then AMH (and egg count) begin to gradually decline.
Around age 35 (ish — it’s different for every woman), our ovarian reserve decline becomes more rapid.
By menopause, egg count and AMH drop to undetectable levels.
If you’re into data like we are, here’s a chart that reflects the median AMH levels between the ages of 25 and 40, as reported in one study by Fertility and Sterility. This chart is meant to illustrate how AMH declines over time — everyone is unique and we all lose eggs at different rates, so your AMH may be higher or lower than these levels and can still be considered normal for your age.
What you can learn from your AMH levels
How Modern Fertility defines normal AMH
A normal AMH level is one that sits within range — it suggests that you have the expected number of eggs for your age. Below you can find a table that outlines the AMH level cutoffs for different age groups according to the Beckman Coulter Access AMH assay (in case you were wondering, an assay is just a laboratory technique to measure something of interest — in this case AMH).
The “Slightly Low” and “Normal” values below are both part of the normal range defined by the Beckman assay. Modern Fertility defines values below 1.3 ng/mL, but still within this normal range, as “Slightly Low.” (We use this clinical decision limit because values below 1.3 ng/mL are more likely to be associated with lower success rates during fertility treatments like egg freezing or IVF.)
Keep in mind that the "reference ranges" between labs can vary, because every lab uses different equipment. This means if your doctor were to re-test at a lab with different equipment, your reference range could be different. This is not to say that you can't compare two results from different labs, but rather that there is a range of what's considered "normal" for healthy people and this range can look different between labs.
AGE | SLIGHTLY LOW AMH (IN NG/ML) | NORMAL (IN NG/ML) |
|---|---|---|
18-25 | 1.02 to below 1.3 | Between 1.3 and 14.63 |
Even if you have normal levels of AMH, Dr. Nataki Douglas, the Chair of the Modern Fertility Medical Advisory Board, says that tracking AMH over time is still important. Dr. Douglas recommends testing once, then again in about 12 months. Beyond that, when you should consider retesting depends on your age, your AMH level, and how it is changing over time.
When looking at your AMH test results, it’s important to remember that even if it’s normal, it’s still possible to experience fertility issues because age, along with many other factors, still plays a big role. Aside from your ovarian reserve, your egg quality is the other big piece of the puzzle. Unfortunately there is no test for egg quality, so age is the best predictor we have.
The implications of having low or very low AMH levels
A low AMH level indicates a lower number of eggs than is expected for your age. Below you can find a table that outlines the AMH level cutoffs for different age groups according to the Beckman Coulter Access AMH assay. (Note that “Very Low” is a Modern Fertility designation assigned to levels that are below the detection limit of the Beckman assay.)
AGE | VERY LOW AMH (IN NG/ML) | LOW AMH (IN NG/ML) |
|---|---|---|
18-25 | Below 0.08 | Between 0.08 and 1.01 |
There are no somatic symptoms (aka symptoms experienced in the body) proven to be associated with low levels of AMH. In addition, most evidence does not show a link between low AMH and the length of time it takes to get pregnant. The biggest consideration of low AMH is a potentially shorter reproductive window (due to fewer eggs), and a lower chance of success in egg freezing and IVF, for people who choose (or need) to use these treatments.
If test results reveal that your AMH level is low and you’re on the younger side, this could be a sign of a diminished ovarian reserve. Tracking your level over time will help you get a handle on the rate at which your ovarian reserve is declining and, while it is very rare, whether premature depleted ovarian reserve could be a possibility for you).
Very low AMH, absent periods, and perimenopausal symptoms could be signs of primary ovarian insufficiency (POI). Dr. Shaun Samples, an OB-GYN in Nashville, defines POI as “the loss of eggs in the ovaries or abnormal function of the ovaries, so that periods and the entire menstrual cycle cease for large stretches of time or permanently before the age of 40.” Note that only 1 in 100 women will be diagnosed with POI — 25% of them may spontaneously ovulate, and 5% to 10% will conceive and deliver after being diagnosed with POI.
Can you increase AMH levels?
AMH levels will inevitably decrease as you get older, so low AMH at some point is expected and will happen to everyone with ovaries. But what if you have low AMH at a younger age?At the moment, there's no known “cure” for low AMH, but potential methods for increasing levels are being studied. One example: A study in the Journal of Human Reproductive Sciences found that moderate exercise was “associated with improved age-specific levels of ovarian reserve.”It's important to understand, however, that even if raising AMH levels was deemed possible, it wouldn't reverse egg loss — once an egg is gone, it's gone.
Additional reading:
The implications of having high levels of AMH
A high AMH level means that you have a higher number of eggs than is expected for your age or than is average for your age. Below you can find a table that outlines the AMH level cutoffs for different age groups.
AGE | HIGH AMH LEVEL (IN NG/ML) |
|---|---|
18-25 | Above 14.63 |
While high AMH could seem beneficial when it comes to egg retrieval for IVF, there are also some detriments:
PCOS: Polycystic ovary syndrome (PCOS) is a common endocrine disorder caused by an imbalance in hormones — one in ten women will be diagnosed with PCOS. Symptoms and observed signs include irregular or absent periods, excess hair growth, weight gain, many follicles that have stopped developing in the ovaries, and fertility issues due to irregular cycles which make it challenging to time intercourse with ovulation. Even though most people with PCOS have a higher number of follicles, they don’t all reach full development because of extra androgens in the body.
There are ongoing discussions about an AMH threshold for PCOS diagnosis in the medical community, but there hasn’t been agreement yet in the field. AMH is not part of the diagnostic criteria for PCOS, and high levels of AMH aren't always present in people with PCOS. So if you have PCOS, it’s important to talk to your doctor about any potential hormonal imbalances so that you can get on the right treatment regimen. Doctors can also trigger ovulation in people whose bodies aren’t doing it naturally with medications like Clomid (which blocks estrogen receptors, stimulates the release of follicle-stimulating hormone, and leads to ovulation), or Letrozole (which lowers your estrogen, increases production of FSH, and helps activate the ovulatory mechanism lying dormant in PCOS).
In addition to issues with fertility, PCOS can lead to pregnancy complications and increased risk of diabetes, cardiovascular disease and endometrial cancer, anxiety, and depression. Early diagnosis can help better treat PCOS and any related conditions. Birth control is often used to manage PCOS. This is because it keeps the ovaries at a hormonal standstill and produces cyclical bleeding, which protects against endometrial cancer, and is a form of contraception. Hormonal birth control can mask PCOS symptoms, but doesn’t resolve them. If you are on hormonal birth control, you may go off of it and not know you have PCOS until you are trying to conceive without the right expectations.
High AMH and ovarian hyperstimulation syndrome: Having high levels of AMH could also put you at risk for ovarian hyperstimulation syndrome (OHSS) if you’re taking fertility drugs during IVF. According to one study, AMH level is the best way to estimate the chances of OHSS — which can cause symptoms like nausea, cramping, and bloating — during ovarian stimulation cycles for egg freezing or IVF. In fact, AMH test results were shown to be a more effective predictor than age, BMI, or antral follicle count. If you’re considering egg freezing or IVF, testing your AMH level just once should be enough to individualize treatment to prep you for the procedure. Based on your AMH, your doctor may adjust doses of the medications used to stimulate follicular development to reduce the risk of OHSS. It’s worth mentioning that OHSS is vastly less common now since we better understand the cause of OHSS and how to prevent it.
Additional reading:
Lifestyle factors that may influence anti-Mullerian hormone
The research into the lifestyle factors that affect AMH most has yielded mixed results. When the American Journal of Obstetrics & Gynecology rounded up the data, they found that smoking and birth control were the only lifestyle factors proven by multiple studies to decrease AMH. (Though one study did discover that a diet low in vitamin D could also have a detrimental effect.)
While we’re on the topic of contraception, let’s break down exactly what effect it has on AMH levels. Studies have shown that hormonal contraception (including the pill, vaginal ring, hormonal IUD and Depo-Provera) may suppress AMH in some women — meaning your level on birth control could be somewhat lower than it would be naturally. Despite this, AMH is still considered the best way to measure ovarian reserve and it’s still an incredibly important fertility biomarker. If you are on hormonal birth control and your level is lower than expected for your age, your doctor might recommend going off your birth control for a few months before testing again.
A recent large, population-based study conducted by the Journal of Clinical Endocrinology & Metabolism also looked into the effects of body-fat percentage, alcohol consumption, and physical exercise on AMH level, but no significant association was demonstrated. (Even so, weight and high-intensity exercise can impact your fertility in other ways.)
Our research team is very interested in the lifestyle factors that influence AMH and we’re currently looking into how things like exercise levels, birth control, smoking, marijuana use, alcohol consumption, and caffeine all impact AMH.
Additional reading:
The relationship between AMH and conception
One single AMH measurement isn’t strongly linked to time to pregnancy, according to a 2017 study. This study has some shortcomings: it didn't track outcomes like miscarriage or live birth (only pregnancy), it only included a small number of women over 35 with low levels of AMH, it excludes women with fertility problems that ended participation in the study to pursue fertility treatments, and it measures a snapshot of AMH instead of tracking AMH over time.
Some studies *do* show that there’s an association between time to pregnancy and AMH in natural conception among women with very low levels of AMH. According to Prof. Nelson, “While we await clarity on the link between AMH and the chance of natural conception, it’s clear that for women having assisted conception, a low AMH is associated with a lower chance of success at all ages — and their desired family size may be unattainable.”
In general, more evidence and research is needed to better understand the connection (or lack thereof), between AMH decline over time and the impact on natural fertility.
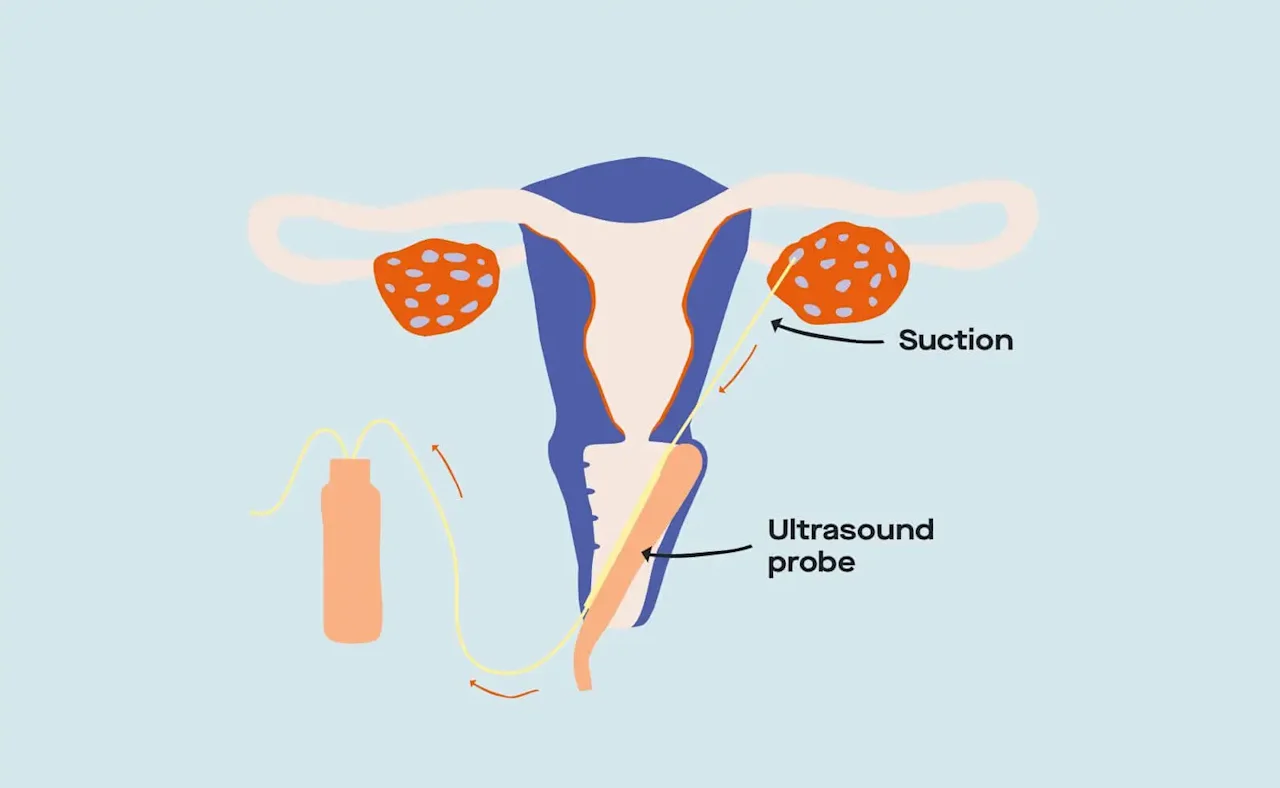
Illustration of the egg retrieval process.
How your AMH level affects the outcome of egg freezing and IVF
Your AMH level comes into play when thinking about an egg retrieval for egg freezing and IVF. This is because AMH is a strong predictor of how many eggs can be extracted, as shown in one 2009 study.
Egg freezing: Whether your level is high or low, it can give you more info to help you make the decision to freeze your eggs or not (based on predicted chances of success during egg retrieval procedures). Birth doula and writer English Taylor used her AMH level to think about proactively freezing her eggs. As she explains, “By freezing my eggs now (with higher AMH), I could be saving my future self some major dough.” Why’s that? Because AMH declines as we age, more harvesting rounds may be needed later in life to get viable eggs.
IVF: Ovarian stimulation, the first step of IVF, is impacted by your ovarian reserve. That’s because the number of eggs that can be retrieved is based on the number of eggs you have. If you have high levels of AMH, there’s a greater likelihood that you’ll get a high number of eggs through egg retrieval. That said, having more eggs doesn’t necessarily mean more embryos. Not all of the eggs we produce end up being viable or high quality enough for IVF.
If you have low AMH, that might mean that you have to do more than one IVF cycle before seeing success. Since fertility treatments are expensive, informing yourself about your AMH early on can be helpful with financial planning.
The relationship between AMH and miscarriage
A study authored by Dr. Brianna Lyttle Schumacher, Anne Marie Jukic, and Anne Steiner explored how higher or lower than average level of AMH impact live birth outcomes. In the study, the AMH levels of women who were trying to conceive naturally were measured. They had to take pregnancy tests every month and report back if they got pregnant, if they didn’t get pregnant, or if they miscarried. The results showed that, after adjusting for age, women with clinical pregnancy loss (pregnancies confirmed via ultrasound that didn’t continue through the 20-week mark) had the lowest levels of AMH.
If a participant’s level was less than or equal to 0.4 ng/mL (“significantly diminished ovarian reserve,” according to the authors), they had 2.2 times the risk for miscarriage. The study also showed that the women with the highest AMH were more likely to miscarry within four days of the first positive pregnancy test.
Bottom line? This study doesn’t say that lower (or higher) AMH causes miscarriage. The study suggests that there may be an association between AMH levels and risk of miscarriage. We can’t draw any firm conclusions on the link between AMH and miscarriage from this single study, and hope to see more research in this area soon.
Now to recap: Here are the main takeaways
Congrats! You made it all the way down to the end of the article. Let’s recap the main points, shall we?
When it comes to your reproductive career, AMH is key. This hormone is the best predictor we have for ovarian reserve, or the number of eggs you have… but that doesn’t mean it can tell you if you’re fertile or not.
There are many reasons why knowing your AMH level can be beneficial, but for an even better understanding, much more research into this hormone is needed. Most research is done on women at fertility clinics, which underrepresents the broad population of women who are trying to get pregnant. The more women who test, the more data we’ll have to show the world just how informative this hormone is. (More knowledge = more power!)
This guide was medically reviewed by multiple members of the Modern Fertility Medical Advisory Board.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
A. Iwase, et al. Anti-Müllerian hormone as a marker of ovarian reserve: What have we learned, and what should we know? Reproductive medicine and biology, 2015.
L.G. Nardo, et al. Anti-Müllerian hormone levels and antral follicle count in women enrolled in in vitro fertilization cycles: Relationship to lifestyle factors, chronological age and reproductive history . Gynecological Endocrinology, 2007.
J.V. Helden, et al. Performance of the two new fully automated anti-Müllerian hormone immunoassays compared with the clinical standard assay . Human Reproduction, 2015.
S.L. Broer, et al. Anti-Müllerian Hormone Predicts Menopause: A Long-Term Follow-Up Study in Normoovulatory Women . The Journal of Clinical Endocrinology & Metabolism, 2011.
M. Dólleman, et al. Anti-Müllerian hormone is a more accurate predictor of individual time to menopause than mother's age at menopause . Human Reproduction, 2014.
J.S. Finkelstein, et al. Anti-Mullerian Hormone and Impending Menopause in Late Reproductive Age: The Study of Women's Health Across the Nation . The Journal of clinical endocrinology and metabolism, 2020.
J.A. Visser, et al. Anti-Müllerian hormone: an ovarian reserve marker in primary ovarian insufficiency . Nature Reviews Endocrinology, 2012.
A. Fraissinet, et al. Use of the serum anti-Müllerian hormone assay as a surrogate for polycystic ovarian morphology: impact on diagnosis and phenotypic classification of polycystic ovary syndrome . Human Reproduction, 2017.
Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion . Fertility and Sterility, 2015.
O. Shebl, et al. Age-related distribution of basal serum AMH level in women of reproductive age and a presumably healthy cohort . Fertility and Sterility, 2011.
S. Torrealday, et al. Premature Ovarian Insufficiency - an update on recent advances in understanding and management . F1000Research, 2017.
M. Singh, et al. A prospective randomised controlled study of serum anti-mullerian hormone (AMH) as a predictive marker of ovarian hyperstimulation syndrome (OHSS) in IVF-ICSI cycles . Fertility and Sterility, 2013.
R. Tal, et al. Ovarian reserve testing: a user’s guide . American Journal of Obstetrics & Gynecology, 2017.
N.A. Dennis, et al. The level of serum anti-Müllerian hormone correlates with vitamin D status in men and women but not in boys . The Journal of Clinical Endocrinology & Metabolism, 2012.
S. Kallio, et al. Antimüllerian hormone levels decrease in women using combined contraception independently of administration route . Fertility and Sterility, 2013.
M. Dólleman, et al. Reproductive and Lifestyle Determinants of Anti-Müllerian Hormone in a Large Population-based Study . The Journal of Clinical Endocrinology & Metabolism, 2013.
O. Hakimi, et al. Effect of Exercise on Ovulation: A Systematic Review . Sports Medicine, 2016.
A.Z. Steiner, et al. Association Between Biomarkers of Ovarian Reserve and Infertility Among Older Women of Reproductive Age . JAMA, 2017.
H.S. Koo, et al. The likelihood of achieving pregnancy through timed coitus in young infertile women with decreased ovarian reserve . The Journal of Clinical Endocrinology & Metabolism, 2018.
S.M. Nelson, et al. Anti-Müllerian hormone-based approach to controlled ovarian stimulation for assisted conception . Human Reproduction, 2009.
B.M. Lyttle Schumacher, et al. Antimüllerian hormone as a risk factor for miscarriage in naturally conceived pregnancies . Fertility and Sterility, 2018.










