Here's what we'll cover
Here's what we'll cover
Most people don’t consider their lung health until a problem develops. It’s easy to forget about lung health because you typically breathe without needing to control it. Still, keeping your lungs healthy is important for your overall well-being. Keep reading to learn 8 ways to protect your lung function.
What is a healthy lung?
Keeping your lungs healthy is essential to your overall health and wellness. Healthy lungs help exchange oxygen and carbon dioxide, maintain acid-base balance in your body, and support your overall quality of life.
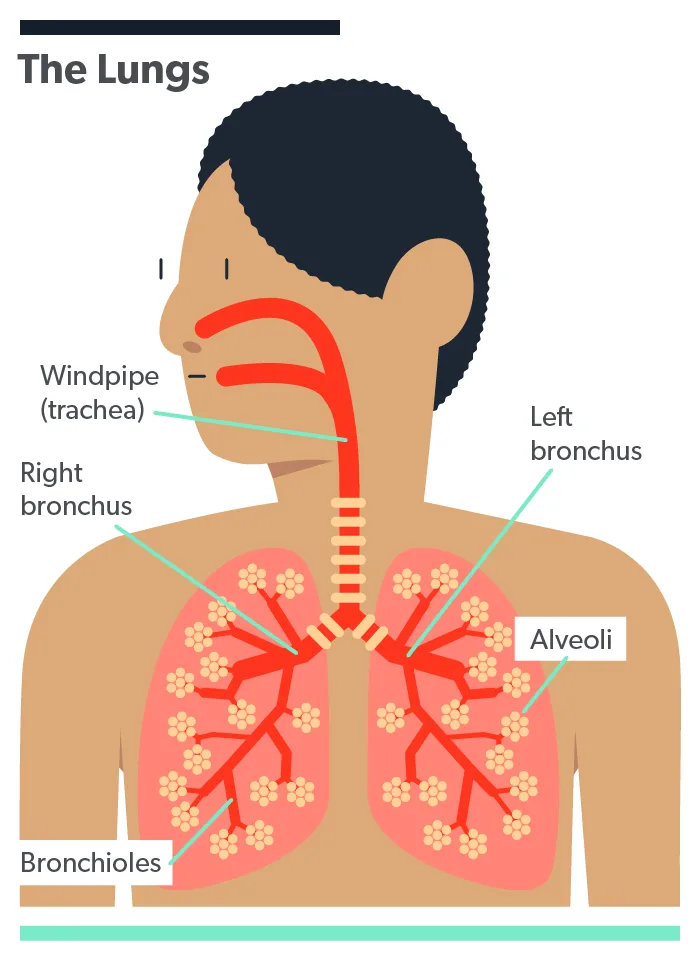
Lungs are a part of your body that functions without your control. Your abdominal muscles, and most importantly the diaphragm, are essential muscles that support your lung function. There are four main pathways that bring air into your lungs (Chaudhry, 2021):
Trachea: the largest tube connecting your upper airway (your nose and mouth) toward the lungs
Bronchi: the large airways branching off from the trachea to your lungs
Bronchioles: smaller airways that branch off from the bronchi inside the lungs
Alveoli: tiny air sacs connected to bronchioles where oxygen and carbon dioxide are exchanged in blood
Types of lung conditions
There are many different conditions and factors that impact your lung health. Here are some common types:
Asthma: a chronic condition causing inflammation and narrowing of the airways.
Chronic obstructive pulmonary disease (COPD): a group of lung diseases that block airflow and make it difficult to breathe
Emphysema: a type of COPD involving gradual damage to the alveoli, causing shortness of breath
Chronic bronchitis: a long-term inflammation of the bronchial tubes
Acute bronchitis: short term inflammation of the bronchi, typically caused by an infection
Allergies: allergens (like pollen, dust, mold, etc.) irritate the lungs leading to inflammation after being exposed to the allergen.
Lung cancer: occurs when a tumor forms in the lungs and could spread to other parts of the body over time
While not all lung conditions can be prevented, there are changes you can make to help support the health of your lungs and prevent disease.
1. Quit smoking and vaping
Both smoking and vaping increase your risk for chronic lung diseases and cancer (St Claire, 2020). The toxins found in these products inflame your airway and cause lung damage. They irritate tissue and lead to a high risk for COPD, lung cancer, and breathing problems.
Try to avoid smoking, vaping, and secondhand cigarette smoke. If you do smoke, stopping smoking prevents further damage from developing in lung tissue. Talk with your healthcare provider or consider joining a support group if you’re having trouble quitting.
2. Boost your indoor air quality
Consider adding an air filter and humidifier to your home or office.
An indoor air filter to your home or office helps remove dust, air pollution, and other irritants from the air (Vijayan, 2015). Remember to replace the filters regularly to help keep your air clean.
If you’re concerned about the air quality in your home, you may consider having testing done. Testing for chemicals and gases, like radon, helps ensure that you’re not being exposed to harmful particles. It’s also a good idea to have a carbon monoxide detector set up at all times in your home.
If you live in an area with colder weather with a furnace running, consider adding a humidifier. Dry air can irritate the lungs, so adding a humidifier may help reduce irritation.
3. Clean regularly
Cleaning your home regularly helps to reduce dust, mold, and other allergens that could impact your lungs. Pet dander, dust mites, insect dropping, and other particles can trigger allergy and asthma symptoms. Vacuuming, dusting, and disinfecting surfaces help reduce triggers for allergy and asthma symptoms and protect your lung health.
4. Practice breathing exercises
Deep breathing exercises can help strengthen the muscles that support healthy lungs, increase lung capacity, and even help decrease stress (Hamasaki, 2020). Typically, breathing exercises are performed while lying or sitting down. You can even do them at your work desk to help reduce stress.
Examples of deep breathing exercises include:
Diaphragmatic breathing focuses on breathing from the diaphragm and expanding the belly while you breathe.
Pursed lip breathing focuses on inhaling through the nose and exhaling slowly with your lips pursed (like when blowing out candles).
Pattern breathing focuses on the rhythm of your breath, such as inhaling for four seconds, holding your breath for seven seconds, and exhaling for eight seconds.
5. Add indoor plants
Placing a few plants inside your home may help improve your air quality. Research is mixed about the effectiveness of plants for removing pollutants. Still, some research shows indoor plants that may help remove harmful substances from the air (Susanto, 2020).
6. Prevent infection
Preventing respiratory illness helps keep your lungs healthy, both in the short and long term. Try these tips to help reduce your risk for infections and colds:
Wash your hands regularly with warm water and soap.
Limit touching your face and mouth.
Avoid indoor crowds during flu season.
If you’re sick, stay home from work or school until you feel better to prevent it from spreading.
Support your immune system by getting enough sleep and exercise and eating a balanced diet.
7. Exercise regularly
Staying active helps all areas of your health. Research shows exercise may even help manage the symptoms of chronic lung conditions (Lang, 2019). Try to include activities that increase your heart rate and breathing, like cardio training.
Here are some tips to add more physical activity into your day:
Go for walks.
Take the stairs.
Schedule workouts.
Dance.
Schedule walking meetings.
Do more chores around the house.
8. See your healthcare provider
Regular check-ups can help prevent or catch medical conditions earlier. Sometimes you may not notice the early signs of lung problems. Your healthcare provider listens to your lungs during routine check-ups, which may help detect early symptoms.
If you have any questions about your lungs or any other areas of health, these visits are also the perfect opportunity to get your questions answered by your healthcare provider.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Chaudhry, R. & Bordoni, B. (2021). Anatomy, thorax, lungs. [Updated Jul 31, 2021]. In: StatPearls [Internet]. Retrieved on Oct. 8, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK470197/
Hamasaki, H. (2020). Effects of diaphragmatic breathing on health: a narrative review. Medicines , 7 (10), 65. doi: 10.3390/medicines7100065. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7602530/
Lang, J. E. (2019). The impact of exercise on asthma. Current Opinion In Allergy And Clinical Immunology , 19 (2), 118–125. doi: 10.1097/ACI.0000000000000510. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30601152/
St Claire, S., Gouda, H., Schotte, K., Fayokun, R., Fu, D., Varghese, C., & Prasad, V. M. (2020). Lung health, tobacco, and related products: gaps, challenges, new threats, and suggested research. American Journal of Physiology , 318 (5), L1004–L1007. doi: 10.1152/ajplung.00101.2020. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7272734/
Susanto, A. D., Winardi, W., Hidayat, M., & Wirawan, A. (2020). The use of indoor plant as an alternative strategy to improve indoor air quality in Indonesia. Reviews on Environmental Health , 36 (1), 95–99. doi: 10.1515/reveh-2020-0062. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32920542/
Vijayan, V. K., Paramesh, H., Salvi, S. S., & Dalal, A. A. (2015). Enhancing indoor air quality -the air filter advantage. Lung India: Official Organ of Indian Chest Society , 32 (5), 473–479. doi: 10.4103/0970-2113.164174. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4587002/












