Here's what we'll cover
Here's what we'll cover
When you think of “birth control,” there’s a good chance you think of the pill, and that makes sense—after all, it’s the most common form of contraception used in the US (Cooper, 2021). But the pill isn’t the only option available if you’re trying to prevent pregnancy. An intrauterine device (IUD) is a safe and extremely effective form of birth control. These devices come with few side effects for most people and can last up to 12 years.
They and other long-acting contraceptives, such as implants, are widely used worldwide and are growing in popularity in the US, rising from 6% of birth control users in 2008 to 14% in 2014 (Kavanaugh, 2018).
However, many people still aren’t familiar with IUDs as a family planning option and may even be a little intimidated by them. Here we’ll explore what IUDs are, how effective they are, their side effects, what to expect when getting one, and some frequently asked questions.
What is an IUD?
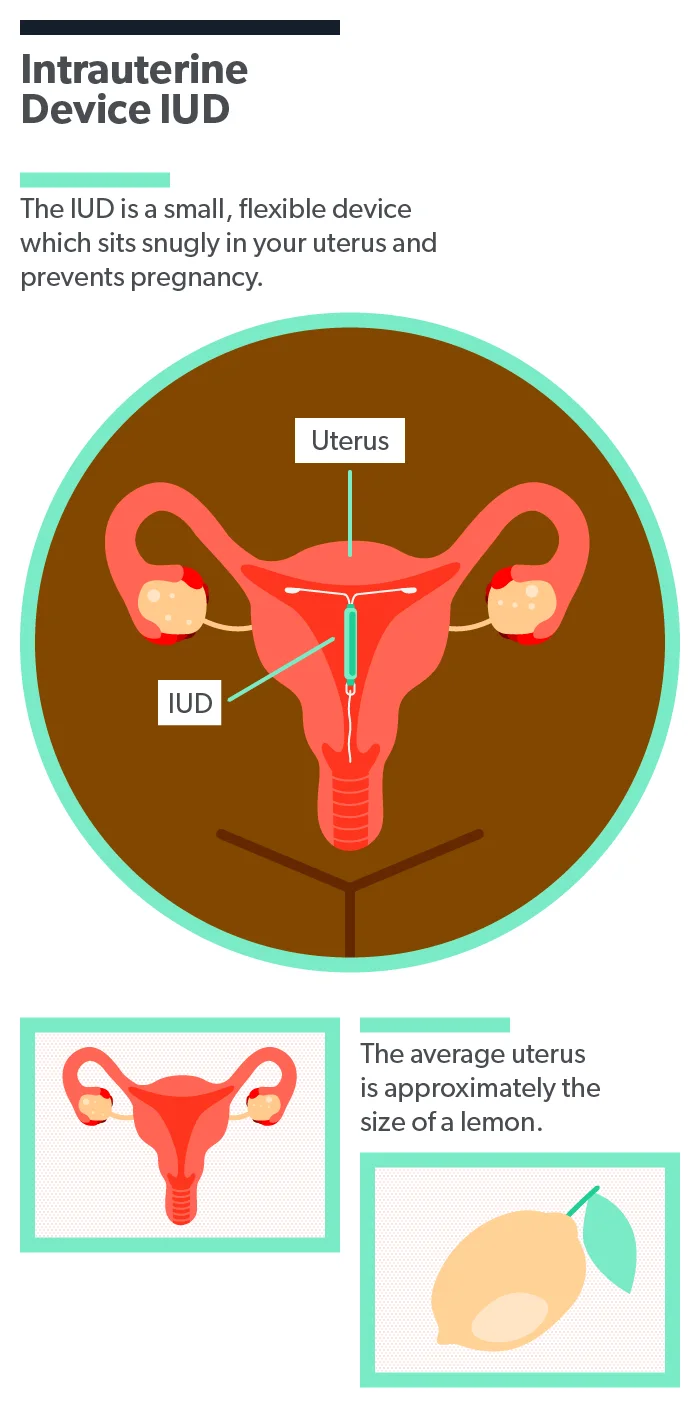
An IUD is a small, flexible, T-shaped contraceptive device that’s only about an inch long. It rests comfortably in your uterus—and no, you can’t feel it once it’s in! It protects you from pregnancy by interfering with the sperm’s ability to reach the egg. A medical provider inserts the IUD, and after that, it doesn’t require any maintenance at all.
How effective are IUDs?
IUDs are incredibly effective—over 99.9%. That’s on par with tubal ligation (commonly referred to as “tying your tubes”), except that IUDs are easily reversible for women who decide they want to try to get pregnant (Lanzola, 2021). It’s also one of the oldest and most highly-researched methods out there; modern IUDs were invented over 60 years ago (Xu, 2021). Furthermore, IUDs have very high user satisfaction rates (Cristobal, 2016; Sanders, 2018).
How long does an IUD last?
Depending on the type you choose, the IUD will protect you from pregnancy for anywhere between 3 to 12 years (Xu, 2021). But you don’t have to keep it in that long if you don’t want to—you can have it removed in a matter of seconds at any time by your medical provider.
It’s important to remember that your body might need an adjustment period, which is completely normal with any medication or contraceptive. Try to give your body about six months to adjust to your IUD before having it removed due to any side effects. If you have concerns, always follow up with your healthcare provider, but remember that many side effects will improve or resolve after a few months (Sanders, 2018; Zgliczynska, 2020).
Types of IUDs
There are two main types of IUD:
Non-hormonal copper IUDs (there is one brand: Paragard)
Hormonal IUDs (there are several brands: Mirena, Liletta, Skyla, and Kyleena)
Both of these types of IUDs are safe, effective, and appropriate for women of all body sizes. They individually have slightly different side effects and ways that they work, so choosing one depends on your individual preference, body, and fertility plans.
Copper IUD (Paragard)
The copper IUD is the only type of non-hormonal IUD available and is one of the most effective birth control methods on the market. It is also the only highly effective modern non-hormonal method. The brand of copper IUD available in the US is Paragard.
What is a copper IUD?
The copper IUD is made of safe, flexible plastic and a small amount of natural copper. It is completely hormone-free, which can be great news for people who are sensitive to hormonal side effects or who just want a non-hormonal birth control option. It also doesn’t interfere with your menstrual cycle, so your body will continue to have the normal rhythm of menstruation and hormones.
How does a copper IUD work?
The copper IUD works by releasing tiny amounts of copper into the area right around it. Sperm don’t like copper, making it difficult for them to swim properly and reach the egg. The amounts of copper released by the IUD are extremely small and nontoxic (in fact, copper is an essential nutrient) (Nelson, 2016; NIH, 2021).
How long does a copper IUD last?
You can use a copper IUD for up to 12 years. This means that it will remain highly effective for a full 12 years if you choose to leave it in for that long. However, you can still have it removed at any point earlier than that.
What are the possible side effects?
As with any birth control method, there are possible side effects with copper IUD. Fortunately, they are generally minor and tend to resolve within a few months (Sanders, 2018). Possible side effects include:
Heavier periods and/or cramping
Spotting in between periods
Despite the possibility of increased bleeding or cramps, a benefit of the copper IUD is that it does not carry any of the side effects associated with estrogen-containing hormonal methods, such as weight gain, mood changes, and increased risk of blood clots (Nelson, 2016).
Who shouldn’t use a copper IUD?
The copper IUD is a great choice for most women. In addition to being effective, long-lasting, and with relatively minor side effects, it also has an immediate return to fertility. That means you can get pregnant as soon as the IUD is removed; there is no “waiting period” for your body—unlike some other methods).
IUDs are rarely contraindicated because of a person’s medical history (Bansode, 2021). However, there are still some women who shouldn’t get one. Women should not get an IUD if they have (Curtis, 2016; Lanzola, 2021):
A very unusually shaped uterus (your provider will tell you if this is the case)
An active sexually transmitted infection (STI) or pelvic infection (but the IUD can be inserted after this has resolved)
Unexplained vaginal bleeding (once this has been addressed with your provider, you may still be able to get an IUD)
For the copper IUD specifically, women who have Wilson’s Disease or a copper allergy should consider other options (although such a reaction with a copper IUD has never actually been reported) (Madden, 2021).
Hormonal IUD (Mirena, Liletta, Skyla, Kyleena)
The hormonal IUD is the same size as the copper IUD, contains a small amount of hormones, and can protect you from pregnancy for 3–7 years, depending on the brand of IUD.
What is a hormonal IUD?
The hormonal IUD is made of safe, flexible plastic and contains a small amount of the hormone progestin, which mimics the body’s natural hormone progesterone (Edwards, 2021). But unlike other forms of hormonal birth control like the pill or injection, the hormones from the IUD are local, not systemic—meaning that they are released only in the space surrounding the IUD, not throughout your body. The IUD also doesn’t contain estrogen. Because of these differences, even though hormonal IUDs contain some hormones, they don’t have the side effects that often accompany other hormonal birth control methods—like weight gain, moodiness, increased risk of blood clots, and others.
There are four different types of hormonal IUD—Mirena, Liletta, Skyla, and Kyleena. They last for different amounts of time and are made by different companies, but they work in the same way.
How does a hormonal IUD work?
The hormonal IUDs protect you from pregnancy by making it more difficult for the sperm to reach the egg. The small amount of progestin they release causes your cervical mucus to become thicker, so the sperm can’t penetrate it. The hormonal IUD also prevents your uterus from building up its inner lining every month, as it typically would. This often causes women’s periods to become lighter; in many cases, menstrual periods may stop altogether. This is perfectly normal and safe—your period is not “building up” inside you. Indeed, reduced periods and PMS are frequent reasons women choose this type of IUD (Nelson, 2016).
How long does a hormonal IUD last?
Each hormonal IUD brand contains a different amount of progestin and lasts for a different amount of time:
Mirena: 7 years
Liletta: 6 years
Kyleena: 5 years
Skyla: 3 years
What are the possible side effects?
Again, as with any birth control method, some possible side effects exist for the hormonal IUD. These side effects include:
Irregular bleeding or absent periods
Spotting in between periods (this tends to go away after a few months)
It bears repeating that most women appreciate these particular side effects; a 2016 study found that, after one year of having a hormonal IUD, 94% of users found these effects on their periods improved their quality of life (Cristobal, 2016).
Who shouldn’t get a hormonal IUD?
Because the hormonal IUD often causes periods to become lighter or to stop altogether, it can be a great choice for those who experience heavy periods or severe PMS. Many women choose a hormonal IUD to help treat symptoms of PCOS, endometriosis, and approaching menopause (Dhamangaonkar, 2015; Xu, 2021).
All IUDs have been approved for women of all ages, regardless of whether or not they have had a baby before, but some women may still be worried about the size of their IUD. If this is the case, Skyla and Kyleena are slightly smaller devices, so some women may prefer them.
Finally, not all women can safely get a hormonal IUD. Women should not get hormonal IUDs if they have (Curtis 2016; Lanzola, 2021):
Breast cancer or other progestin-sensitive cancer
Liver tumors or disease
A very unusually shaped uterus (your provider will tell you if this is the case)
An active STI or pelvic infection (but the IUD can be inserted after this has resolved)
Unexplained vaginal bleeding (once this has been addressed with your provider, you may still be able to get an IUD)
IUD insertion and removal: what to expect
The idea of getting an IUD inserted or removed is understandably a little daunting. Fortunately, both procedures are quick, simple, and usually less uncomfortable than people expect.
Insertion
An IUD is inserted by a licensed medical provider (this can be a doctor, midwife, or nurse practitioner). It can be done wherever you get routine GYN care or at a freestanding reproductive health clinic, such as Planned Parenthood.
Insertion only takes a few minutes. You’ll be reclined on an exam table with your feet in stirrups, and the provider will insert a speculum—just like for a regular vaginal exam. Then he or she will use a tool to gently hold your cervix steady, insert a thin applicator like a straw, and place the IUD in your uterus. This all takes about five minutes in total.
The IUD has two very thin strings attached to it, which hang a little bit out of your cervix (the opening to your uterus). This is just so that the provider can check the IUD placement and remove the IUD later on. You won’t be able to feel them (unless you gently reach a finger up and look for them, which is fine to do). They become soft and flexible like dental floss, so male sexual partners generally can’t feel them either.
Most people feel a deep cramp or a little dizzy when the IUD is inserted, but this should subside after about a minute. You can rest on the table for a few minutes to relax, and then you are done and able to go about your day as usual. Afterward, you may continue to feel a little cramping or have some spotting, which is completely normal. If you are able, it can be nice to take a few hours afterward for some self-care and relaxation.
Here are some tips to make IUD insertion more comfortable:
An hour before insertion, take an NSAID, like naproxen or ibuprofen (Lopez, 2015).
During the procedure, focus on taking long, slow, deep breaths through your belly. This helps your pelvic muscles relax and prevents you from tensing up too much.
Gently cough during the actual IUD insertion (you can ask your provider to tell you when to do it). This helps your pelvic muscles soften and open even more and can be a helpful distraction.
Removal
IUD removal is even easier than IUD insertion. It is done by your healthcare provider, who will again have you recline on the exam table with your feet in the stirrups. The provider will grasp the IUD strings and gently pull—and that’s it! The IUD is flexible and collapsible and should slide right out—this takes only seconds and should cause you barely any discomfort.
You can have your IUD removed at any time, too—you don’t need to wait for the full lifespan of the device to be up. If at any time you decide the IUD isn’t right for you, you can decide to have it removed.
Common questions about IUDs
There is a lot of information available online about birth control, but many people still have questions about IUDs. Here are the answers to some frequently asked questions:
What are the benefits of an IUD?
IUDs are a great contraceptive method for many reasons:
They’re incredibly safe and effective.
They don’t interrupt the heat of the moment—you don’t need to worry about timing, caps, sprays, condoms, rings, or pulling out to prevent pregnancy.
Your partner can ejaculate inside of you.
Hormonal IUD use reduces your lifetime risk of endometrial and ovarian cancer (Zgliczynska, 2020).
You can set it and forget it—once you have an IUD, there is nothing you ever need to remember to do to prevent pregnancy.
They’re very private—nobody needs to know you have an IUD.
You never need to go to a pharmacy, remember to take a pill, or pay for a prescription.
Are IUDs safe?
Yes, they are one of the safest and most reliable methods of birth control available (Lanzola, 2021; Zgliczynska, 2020). Both the copper IUD and the hormonal IUD are also safe to use while breastfeeding (Curtis, 2016).
Many women still feel concerned about having an IUD. It can be difficult for people to wrap their heads around having a device resting inside their bodies, even if it is small and safe. This is partially because, for a long time in the US, IUDs suffered from a reputation problem. In the 1970s and 80s, a defective early model of the IUD, the Dalkon Shield, caused a number of lawsuits and was taken off the market. This controversy made many Americans suspicious of IUDs in general. In the interest of safety, the FDA required subsequent IUDs and medical devices to be subjected to extreme caution with testing and development. The copper and hormonal versions developed after that have had excellent safety profiles for decades across the globe (Nelson, 2016).
It can be helpful to remember that many other small medical devices are widely accepted and routinely used in healthcare and wellness, such as dental crowns and implants, contact lenses, cochlear implants, cardiac stents, and pacemakers.
What are the risks of IUDs?
As with any medication or medical device, there are some small possible risks with an IUD.
There is a very small risk of injury to the uterus, or perforation, at the time when the IUD is inserted. A 2017 systematic review assessed the experiences of over 90,000 women and found that this risk was between 0.0% and 0.1% for women of all ages (Jatlaoui, 2017).
There is also a small risk of pelvic infection (including if a person has an undiagnosed STI). This typically appears in the first 20 days after IUD insertion. The first step is to simply treat the infection; there is no need to remove the IUD unless the infection treatment doesn’t work (Bansode, 2021).
Will I be able to feel an IUD inside of me?
No. The IUD is small, flexible, and cannot be felt inside of you (no matter how you bend or twist your body). You may be able to feel your IUD strings if you reach a finger into your vagina and gently sweep it along your cervix. This is normal and is helpful for the healthcare provider who will later check or remove your IUD. Your partner should not be able to feel your IUD unless they also insert a finger and feel for the strings.
Can my partner finish inside of me if I have an IUD?
Yes, and this is something many people appreciate about the IUD—your partner can ejaculate inside of you with no increased risk of pregnancy.
Does it hurt to get an IUD?
For some people, yes, getting an IUD is a little painful. Usually, this is felt as a sharp or deep cramp right when the IUD is inserted, but this will generally go away after a minute or two. Afterward, you may feel some cramping, but this will also subside within hours or days.
Can the IUD fall out or travel inside my body?
The uterus is only about the size of a lime, so the IUD fits snugly and comfortably without “floating around” anywhere. It can’t travel around your body or get lost.
There is a small chance of IUD expulsion, where the IUD may come partially out of the uterus, into the vagina. If this happens, it usually occurs within the first three months. Some evidence (though it is inconsistent) suggests that younger IUD users may be slightly more at risk of this than older users. This is generally not a medical risk, as it tends to be obvious to the user and easily addressed by a healthcare provider (who will simply remove the IUD and place a new one if necessary). However, if ignored, it can lead to injury or unintended pregnancy (Jatlaoui, 2017).
Can you get an IUD if you’ve never had a baby?
Yes. All types of IUD are just as safe and effective, whether or not you have had a baby before (Curtis, 2016).
Will an IUD make me gain weight?
No. There is no evidence that either the hormonal or the copper IUD will cause you to gain weight (Zgliczynska, 2020).
Can I get an STI if I have an IUD?
Yes, you can. The IUD does not protect against STIs or STDs. Unless both you and your partner have been tested and are monogamous, you should continue to use condoms to protect yourself from sexually transmitted infections (Curtis 2016).
How much does an IUD cost?
Thanks to the Affordable Care Act, most women with health insurance can get an IUD for free. For those without insurance, community clinics such as Planned Parenthood have sliding scales for services, enabling you to get an IUD at a price you can afford (and even for free). If you pay for it fully out of pocket, it can cost several hundred dollars, but this is a one-time cost; over the lifetime of the device, the monthly cost would average out to only a few dollars per month.
The IUD is gaining popularity worldwide, and for good reasons. If you are interested in getting one, are wondering if it’s right for you, or if you want more information, reach out to your healthcare provider to discuss the IUD.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Bansode, O. M., Sarao, M. S., & Cooper, D. B. (2021). Contraception. [Updated Jul 26, 2021]. In: StatPearls [Internet]. Retrieved on Jan. 20, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK536949/
Cooper, D. B. & Mahdy, H. (2021). Oral contraceptive pills. [Updated Dec 16, 2021]. In: StatPearls [Internet]. Retrieved on Jan. 20, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK430882/
Cristobal, I., Lete, L.I., Viuda, E., Perulero, N., Arbat, A., Canals, I. (2016). One year quality of life measured with SEC-QoL in levonorgestrel 52 mg IUS users. Contraception, 93 (4):367-371. doi: 10.1016/j.contraception.2015.12.014. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26764120/
Curtis, K. M., Tepper, N. K., Jatlaoui, T. C., Berry-Bibee, E., Horton, L. G., Zapata, L. B., et al. (2016). U.S. Medical Eligibility Criteria for Contraceptive Use, 2016 (65, Report No. RR-3). MMWR Recommendations and Reports 2016. doi: http://dx.doi.org/10.15585/mmwr.rr6503a1. Retrieved from https://www.cdc.gov/mmwr/volumes/65/rr/pdfs/rr6503.pdf
Dhamangaonkar, P. C., Anuradha, K., & Saxena, A. (2015). Levonorgestrel intrauterine system (Mirena): An emerging tool for conservative treatment of abnormal uterine bleeding. Journal of Mid-life Health , 6 (1), 26–30. doi: 10.4103/0976-7800.153615. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4389381/
Edwards, M. & Can, J. (2021). Progestin. [Updated Sep 22, 2021]. In: StatPearls [Internet]. Retrieved on Jan. 20, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK563211/
Jatlaoui, T. C., Riley, H. E. M., & Curtis, K. M. (2017). The safety of intrauterine devices among young women: a systematic review. Contraception, 95 (1):17-39. doi: 10.1016/j.contraception.2016.10.006. Retrieved from https://pubmed.ncbi.nlm.nih.gov/27771475/
Kavanaugh, M. L. & Jerman, J. (2018), Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception, 97 (1):14-21. doi: 10.1016/j.contraception.2017.10.003. Retrieved from https://www.sciencedirect.com/science/article/pii/S001078241730478X
Lanzola, E. L. & Ketvertis, K. (2021). Intrauterine Device. [Updated Jul 31, 2021]. In: StatPearls [Internet]. Retrieved on Jan. 20, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK557403/
Lopez, L. M., Bernholc, A., Zeng, Y., Allen, R. H., Bartz, D., O'Brien, P. A., & Hubacher, D. (2015). Interventions for pain with intrauterine device insertion. Cochrane Database Systematic Review, 29 (7):CD007373. doi: 10.1002/14651858.CD007373.pub3. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26222246/
Madden, T. (2021). Intrauterine contraception: Candidates and device selection. In Schreiber, C. & Eckler, K. (Ed.), UpToDate . Retrieved on Jan. 12, 2021 from https://www.uptodate.com/contents/intrauterine-contraception-candidates-and-device-selection
Nelson, A. L. & Massoudi, N. (2016). New developments in intrauterine device use: focus on the US. Open Access Journal of Contraception , 7 , 127–141. doi: 10.2147/OAJC.S85755. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5683151/
NIH Office of Dietary Supplements. (2021). Copper [Fact sheet]. U.S. Department of Health and Human Services . Retrieved from https://ods.od.nih.gov/factsheets/Copper-HealthProfessional/
Sanders, J. N., Adkins, D. E., Kaur, S., Storck, K., Gawron, L. M., & Turok, D. K. (2018). Bleeding, cramping, and satisfaction among new copper IUD users: A prospective study. PloS One , 13 (11), e0199724. doi: 10.1371/journal.pone.0199724. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6221252/
Xu, X., Ruan, X., & Rabe, T. (2021). Intrauterine contraception and menstrual bleeding. Global Health Journal, 5 (2), 66-69. doi: 10.1016/j.glohj.2021.05.002. Retrieved from https://www.sciencedirect.com/science/article/pii/S2414644721000427#bib0007
Zgliczynska, M., Kocaj, K., Szymusik, I., Dutsch-Wicherek, M. M., Ciebiera, M., & Kosinska-Kaczynska, K. (2020). Levonorgestrel-releasing intrauterine system as a contraceptive method in nulliparous women: a systematic review. Journal of Clinical Medicine , 9 (7), 2101. doi: 10.3390/jcm9072101. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7408997/











