Here's what we'll cover
Here's what we'll cover
Folate, better known as vitamin B9, is an essential vitamin for many basic bodily functions. Folate is necessary to manufacture red blood cells and repair and make new DNA (Merrell, 2020). Folate is also known to lower the risk of neural tube defects (NTDs), which are malformations of the brain and spine that develop before birth.
Low folate levels can lead to dangerous conditions, such as megaloblastic anemia, a condition in which red blood cells become oversized and malformed.
Folate is turned into many different compounds in our bodies, each of which has its own function. Converting folate into these compounds is a complicated process involving many eleven-syllable words, so we won't go into each and every detail. But one important form of folate is levomefolic acid, also known as l-methylfolate.
Technically, the full name of l-methylfolate is 5-methyltetrahydrofolate. Only nine syllables, but we'll stick to "methylfolate" for this article. This compound is available as a supplement on its own. Since it is an active form of folate, it requires less processing in our bodies.
In addition to finding supplements labeled “methylfolate,” you may see it on packaging abbreviated as “5-MTHF” as well. To make matters more confusing, you might also find L-5-MTHF and (6S)-5-MTHF. As a consumer, there's no difference between these, just two more ways of scientifically naming the same thing.
Methylfolate does many things in the body. One of the most important is converting homocysteine to methionine. Methionine is a vital amino acid for building and repairing blood vessels. It breaks down into homocysteine as we use it. Methylfolate "recycles" it back into its original form, and the cycle repeats. Too much homocysteine can raise the risks of cardiovascular disease, Alzheimer's disease, and vision or hearing loss (Kim, 2018).
Methylfolate can cross the blood-brain barrier. Methylfolate regulates the synthesis of serotonin, norepinephrine, and dopamine, three vital neurotransmitters in the brain. Low folate levels have been linked to neuropsychiatric conditions, including depression (Stahl, 2008).
All this to say, we need methylfolate for many reasons. But how do we get it, and do some of us need more than others?
Sources of methylfolate
In simple terms, we take in folate through natural foods or supplements (as folic acid), which we then break down into methylfolate.
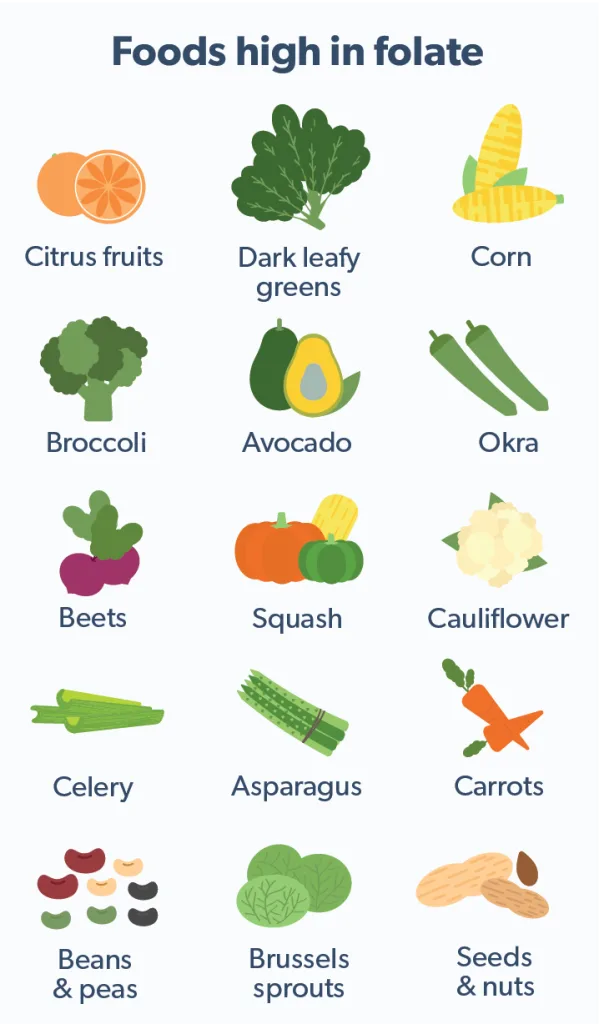
The most common way to get folate is, as you might expect, from food. Organ meats, especially poultry livers, are among the best sources. There are excellent plant sources of folates for vegetarians or those who aren't fans of offal. Legumes, beans, seeds, and nuts are all high in natural folate. Leafy green vegetables, spinach, asparagus, and avocado will all boost your folate as well (USDA, n.d.).
Another common way to get folate is through folic acid. Folic acid is the form in which folate appears in most dietary supplements.
Even if you don't take a multivitamin or folic acid supplement, you're likely getting folic acid through other sources. Since 1998, the US government has mandated that enriched cereal grains have folic acid. Enrichment is a process by which manufacturers re-add nutrients lost during processing. Fortification is enrichment above and beyond the original amounts or with nutrients that were never in the original grains. Because of the mandate, the terms "enriched" and "fortified" are virtually synonymous in the United States in terms of folic acid content.
This mandate was enacted to prevent NTDs and is considered enormously successful. Researchers estimate that over 1300 NTDs are avoided in the US every year due to fortification (Williams, 2015). Over 80 countries now mandate folic acid fortification (Wald, 2018).
Because of potential adverse health effects from too much folic acid, the Institute of Medicine at the National Institutes of Health (NIH) set a tolerable upper intake level (UL) for folic acid of 1 milligram, which is 1,000 micrograms, per day (Field, 2018).
Folic acid requires more processing than naturally occurring folate, and our bodies can only process so much per day. Most people in the US consume more folic acid than they can use. One study of over 2,000 randomly selected blood serum samples found over 95% had unmetabolized folic acid (Pfeiffer, 2015). Unmetabolized folic acid is useless and perhaps even harmful at high levels (Morris, 2010).
Instead of folic acid, some healthcare providers may recommend methylfolate supplements for folate-deficient patients. These differ from folic acid in that methylfolate is already in its active form. Unlike folic acid, the NIH has established no upper intake level for methylfolate.
Methylfolate for mental health
About one-third of patients with major depression are estimated to have low folate levels. This deficiency might reduce the body's response to traditional antidepressants, such as selective serotonin reuptake inhibitors (SSRIs). Augmenting SSRI treatment with folate has been shown to help many patients who have not responded to SSRIs alone (Miller, 2008).
In one small trial, depressed patients who did not respond to antidepressants took a daily dose of 15mg methylfolate in addition to their medications. 38% fully recovered, and 51% experienced at least some relief from their depressive symptoms (Zajecka, 2016). Another trial found supplementing antidepressants with methylfolate at the start of treatment led to better outcomes and faster recovery time (Ginsberg, 2011).
The outlook isn’t so rosy when it comes to using methylfolate on its own for depression. A large meta-analysis found no hard evidence in clinical trials for the effectiveness of methylfolate as a monotherapy. But like the studies noted above, this one did note the success of using folate or methylfolate in conjunction with antidepressants (Roberts, 2018).
Who needs extra methylfolate?
The NIH recommends a daily DFE of 400 micrograms for typical adults. DFE stands for dietary folate equivalency. Folic acid, the version used in supplements or fortification, is handled by the body differently than folate naturally occurring in foods. 200 mcg of folic acid attached to fortified pasta or in a pill is not the same as 200 mcg of folate naturally occurring in a salad. To address this, you’ll see that nutrition labels on supplements and fortified foods always list both folic acid and DFE.
The average person doesn't need folate supplementation. If one's diet is erratic, most multivitamins will round up any day-to-day deficiencies to the recommended amount while staying below the upper intake level. But there are some people for whom healthcare providers might recommend an extra folate boost. Usually, this would come in the form of folic acid.
For example, women who are pregnant or breastfeeding have a higher level of recommended folate intake. To ensure that they meet this requirement, many healthcare providers will recommend they take a supplement.
Some people have a genetic condition that hinders the body's ability to get methylfolate. We all have a gene called (take a deep breath) 5,10-methylenetetrahydrofolate, conveniently (and to some, amusingly) abbreviated as MTHFR. The MTHFR gene produces an enzyme that plays a crucial role in converting folic acid's raw material into the methylfolate we can use.
A significant number of people have an MTHFR gene mutation that keeps them from converting as much methylfolate as they need. Folic acid supplements can raise the levels some. Methylfolate supplements effectively bypass the process, giving folate in a form we can already easily use (Vidmar Golja, 2020).
Another enzyme necessary for folate metabolism is dihydrofolate reductase (DHFR). It works at a different point in the process than MTHFR but is just as essential. Some medications work by inhibiting DHFR. One example is methotrexate, an anticancer drug that’s also prescribed for immune disorders, including psoriasis. Other drugs in this class are listed below. Taking folate or methylfolate may impact the effectiveness of such medications, so be sure to speak with your healthcare provider before taking any supplement (Nazarian, 2016).
Some medical conditions can cause a folate deficiency by reducing the body's ability to absorb or process it, or by increasing the body's need for it. Some of these conditions include (Maron, 2009):
Crohn's disease
Inflammatory bowel syndrome (IBS)
Diabetes
Celiac disease
Cancer
Alcoholism
Sickle cell disease
Liver disease
Tuberculosis
Folate needs may also increase after specific medical procedures. These include stomach or bowel surgeries and dialysis (Maron, 2009).
Methylfolate precautions and side effects
Though folate is a vitamin, it can interact with some medications in negative ways. These include (DailyMed, 2015):
Dihydrofolate Reductase Inhibitors, such as methotrexate, aminopterin, pyrimethamine, triamterene, and trimethoprim
Antiepileptic medications, such as phenytoin, carbamazepine, primidone, valproic acid, phenobarbital, and lamotrigine
Sulfasalazine
Fluoxetine (brand name Prozac)
Capecitabine
Isotretinoin
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Oral contraceptives
Methylprednisolone
Pancreatic Enzymes
Pentamidine
Metformin
Warfarin
Many researchers believe that large doses of folates could "mask" a vitamin B12 deficiency (Strickland, 2013). Healthcare providers often detect a vitamin B12 deficiency by recognizing a certain type of anemia it causes. Excess folate could potentially fix the anemia, allowing the B12 deficiency to go unrecognized, while other damage low B12 causes would continue undetected.
High folate levels may also increase the risk of certain cancers. Studies have found an increased risk for colorectal tumors (Kim, 2007) and prostate cancer (Figueiredo, 2009). While these studies focused on folic acid, research is still ongoing.
While methylfolate is a vitamin and available over the counter, there are potential adverse effects from overuse. Talk to a healthcare provider before beginning any supplement regimen, to find out what makes the most sense for your health.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
DailyMed - L-METHYLFOLATE CALCIUM- levomefolate calcium tablet, coated. Retrieved February 10, 2021 from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=76386336-417d-4f90-8171-1f745198ded2
Field, M. S., & Stover, P. J. (2018). Safety of folic acid. Annals of the New York Academy of Sciences, 1414 (1), 59–71. doi: 10.1111/nyas.13499 Retrieved from https://pubmed.ncbi.nlm.nih.gov/29155442/
Figueiredo, J. C., Grau, M. V., Haile, R. W., Sandler, R. S., Summers, R. W., Bresalier, R. S., et al. (2009). Folic acid and risk of prostate cancer: Results from a randomized clinical trial. Journal of the National Cancer Institute, 101 (6), 432–435. doi: 10.1093/jnci/djp019 Retrieved from https://pubmed.ncbi.nlm.nih.gov/19276452/
Ginsberg, L. D., Oubre, A. Y., & Daoud, Y. A. (2011). L-methylfolate plus ssri or snri from treatment initiation compared to ssri or snri monotherapy in a major depressive episode. Innovations in Clinical Neuroscience, 8 (1), 19–28. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21311704/
Kim, J., Kim, H., Roh, H., & Kwon, Y. (2018). Causes of hyperhomocysteinemia and its pathological significance. Archives of Pharmacal Research, 41 (4), 372–383. doi: 10.1007/s12272-018-1016-4 Retrieved from https://pubmed.ncbi.nlm.nih.gov/29552692/
Kim, Y.I. (2007). Folate and colorectal cancer: An evidence-based critical review. Molecular Nutrition & Food Research, 51 (3), 267–292. doi: 10.1002/mnfr.200600191 Retrieved from https://pubmed.ncbi.nlm.nih.gov/17295418/
Maron, B. A., & Loscalzo, J. (2009). The treatment of hyperhomocysteinemia. Annual Review of Medicine, 60, 39–54. doi: 10.1146/annurev.med.60.041807.123308 Retrieved from https://pubmed.ncbi.nlm.nih.gov/18729731/
Merrell, B. J., & McMurry, J. P. (2020). Folic acid. In StatPearls. StatPearls Publishing. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32119374/
Miller, A. L. (2008). The methylation, neurotransmitter, and antioxidant connections between folate and depression. Alternative Medicine Review: A Journal of Clinical Therapeutic, 13 (3), 216–226. Retrieved from https://pubmed.ncbi.nlm.nih.gov/18950248/
Morris, M. S., Jacques, P. F., Rosenberg, I. H., & Selhub, J. (2010). Circulating unmetabolized folic acid and 5-methyltetrahydrofolate in relation to anemia, macrocytosis, and cognitive test performance in American seniors. The American Journal of Clinical Nutrition, 91 (6), 1733–1744. doi: 10.3945/ajcn.2009.28671 Retrieved from https://pubmed.ncbi.nlm.nih.gov/20357042
National Institutes of Health Office of Dietary Supplements (n.d.). Folate. Retrieved February 6, 2021, from https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
Nazarian, R. S., & Lamb, A. J. (2017). Psoriatic flare after the concomitant administration of L-methylfolate and methotrexate. JAAD Case Reports, 3 (1), 13–15. doi: 10.1016/j.jdcr.2016.10.001 Retrieved from https://pubmed.ncbi.nlm.nih.gov/28050589/
Pfeiffer, C. M., Sternberg, M. R., Fazili, Z., Yetley, E. A., Lacher, D. A., Bailey, R. L., & Johnson, C. L. (2015). Unmetabolized folic acid is detected in nearly all serum samples from US children, adolescents, and adults. The Journal of Nutrition, 145 (3), 520–531. doi: 10.3945/jn.114.201210 Retrieved from https://pubmed.ncbi.nlm.nih.gov/25733468/
Roberts, E., Carter, B., & Young, A. H. (2018). Caveat emptor: Folate in unipolar depressive illness, a systematic review and meta-analysis. Journal of Psychopharmacology (Oxford, England), 32 (4), 377–384. doi: 10.1177/0269881118756060 Retrieved from https://pubmed.ncbi.nlm.nih.gov/29442609/
Stahl, S. M. (2008). L-methylfolate: A vitamin for your monoamines. The Journal of Clinical Psychiatry, 69 (9), 1352–1353. doi: 10.4088/jcp.v69n0901 Retrieved from https://pubmed.ncbi.nlm.nih.gov/19193337/
Stolzenberg-Solomon, R. Z., Chang, S.-C., Leitzmann, M. F., Johnson, K. A., Johnson, C., Buys, S. S., Hoover, R. N., & Ziegler, R. G. (2006). Folate intake, alcohol use, and postmenopausal breast cancer risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. The American Journal of Clinical Nutrition, 83 (4), 895–904. doi: 10.1093/ajcn/83.4.895 Retrieved from https://pubmed.ncbi.nlm.nih.gov/16600944/
Strickland, K. C., Krupenko, N. I., & Krupenko, S. A. (2013). Molecular mechanisms underlying the potentially adverse effects of folate. Clinical Chemistry and Laboratory Medicine, 51 (3), 607–616. doi: 10.1515/cclm-2012-0561 Retrieved from https://pubmed.ncbi.nlm.nih.gov/23241610/
U.S. Department of Agriculture (n.d.). FoodData Central. Generated interactively: Retrieved February 6, 2021, from https://fdc.nal.usda.gov/fdc-app.html#/?component=1187
Vidmar Golja, M., Šmid, A., Karas Kuželički, N., Trontelj, J., Geršak, K., & Mlinarič-Raščan, I. (2020). Folate insufficiency due to mthfr deficiency is bypassed by 5-methyltetrahydrofolate. Journal of Clinical Medicine, 9 (9). doi: 10.3390/jcm9092836 Retrieved from https://pubmed.ncbi.nlm.nih.gov/32887268/
Wald, N. J., Morris, J. K., & Blakemore, C. (2018). Public health failure in the prevention of neural tube defects: Time to abandon the tolerable upper intake level of folate. Public Health Reviews, 39,
doi: 10.1186/s40985-018-0079-6 Retrieved from https://pubmed.ncbi.nlm.nih.gov/29450103/
Williams, J., Mai, C. T., Mulinare, J., Isenburg, J., Flood, T. J., Ethen, M., et al & Centers for Disease Control and Prevention. (2015). Updated estimates of neural tube defects prevented by mandatory folic Acid fortification—United States, 1995-2011. MMWR. Morbidity and Mortality Weekly Report, 64 (1), 1–5. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25590678/
Zajecka, J. M., Fava, M., Shelton, R. C., Barrentine, L. W., Young, P., & Papakostas, G. I. (2016). Long-term efficacy, safety, and tolerability of L-methylfolate calcium 15 mg as adjunctive therapy with selective serotonin reuptake inhibitors: A 12-month, open-label study following a placebo-controlled acute study. The Journal of Clinical Psychiatry, 77 (5), 654–660. doi: 10.4088/JCP.15m10181 Retrieved from https://pubmed.ncbi.nlm.nih.gov/27035404/












