As a doctor, I wouldn’t blame patients for putting off care for something less than life-threatening at some point over the past year. After all, visiting the doctor’s office could expose them to the Coronavirus — a potentially much more serious threat to their health.
The problem is, it’s not likely that all of those patients who did put off care — 36% of U.S. adults according to research — will ever get the care they need. Patients delaying care isn’t new, it was an epidemic in its own right prior to COVID-19 — and without changes to our healthcare system will stick around long after.
It’s not hard to understand why different patients delay their care. Lower income patients, may be price sensitive, younger adults, may not have a primary care doctor, rural populations may not have access to in-person care, and patients of color may be more likely to be uninsured. But, we also know what happens when they do:
Delaying care can have serious consequences not only for patients’ personal health but their lives, their families and loved ones, and the healthcare system at large.
Fortunately, the COVID-19 pandemic helped reveal several ways to address the strongest factors leading patients to delay or forgo care.
Our healthcare system’s reliance on patients visiting brick-and-mortar locations has historically left too many patients on the outside looking in. That’s why, patients’ accelerated use and trust in telemedicine is a bright spot in the pandemic — but limitations persist, as you cannot administer a vaccine or conduct imaging remotely.
We’ve learned that a hybrid healthcare system, bringing together the strengths of virtual and in-person care, can better serve a diverse U.S. patient population with even more diverse health needs.
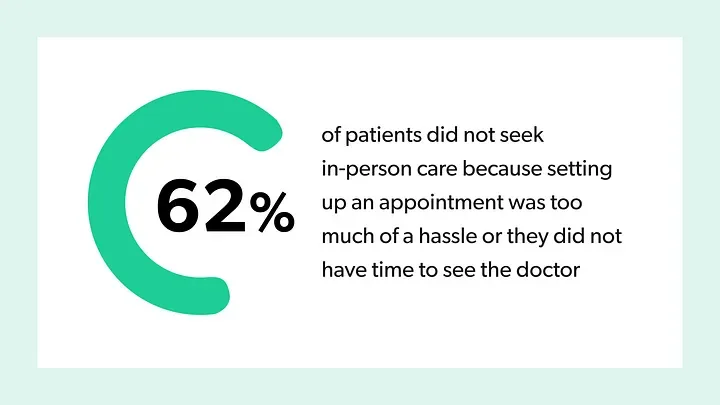
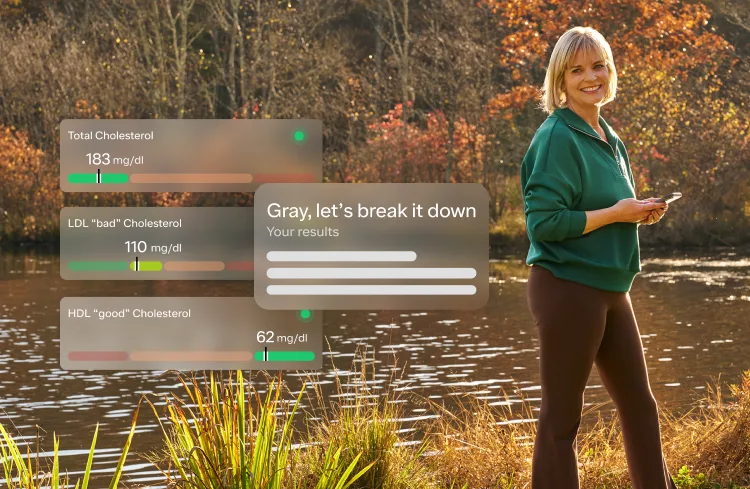
Data from Ro’s Patient Experience Report
Telemedicine can help a patient get an off-hours or same-day visit, avoid a cross-town drive, or limit their potential exposure to COVID-19. It can also serve as a tool for in-person providers. A primary care physician may use it to continuously check-in with an existing patient, in a way that’s more affordable and convenient than expecting them to take off work or pay for childcare to accommodate regular trips to the office. Together, telemedicine in tandem with in-person care can create a more seamless healthcare experience for patients that makes it easier for them to get the care they need — virtually or in-person.
During the pandemic, many faced tougher or unpredictable financial situations. High costs, whether for their daily blood pressure medication or a COVID-19 test, were enough for patients for patients to leave prescriptions unfilled or say, “it’s not that urgent,” about an undiagnosed sickness. Cost concerns not only affect tens of millions of uninsured Americans, but also the many more who are underinsured and even those with increasingly costly employer-sponsored insurance.
It’s clear that cash-pay healthcare can offer improved access to care, more price transparency, less complex billing, and greater affordability.
Uninsured patients can have greater confidence entering the healthcare system with cash-pay options and, despite their reputation, cash prices can save patients money. For instance, research has shown that 28% of the time a commercially insured patient’s generic drug copay is more than the cash price they’d pay. And, when prices are disclosed, patients can actually search based on price rather than navigating a health plan’s archaic website or wondering how many zeros will be on their bill. Cash-pay healthcare can give patients the knowledge of costs and the power of choice.
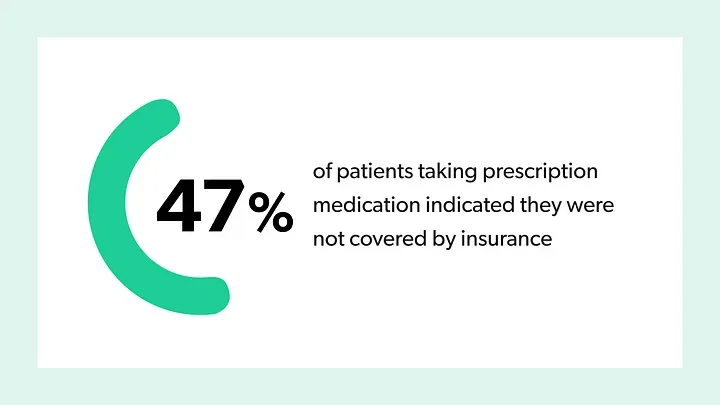
Data from Ro’s Patient Experience Report
The pandemic has revealed the true depth that Social Determinants of Health (SDOH) play in patients’ health — driving home the importance of care that meets patients’ clinical needs, and accounts for other parts of their life that affect their health.
This is clear in the rate of COVID-19 infection, hospitalization, and deaths across income levels and demographics. This tragic data though can help us learn lessons to improve healthcare equity — connecting the dots on factors like food insecurity, where patients may choose a meal over medicine, or employment opportunities, where they may prefer money in their pocket to seeing a doctor in the clinic.
Retail pharmacies have begun investing in affordable housing and health systems have been offering free transportation through ride-sharing. Looking ahead, in-home care can remove time-oriented, mobility, and transportation barriers for patients, while giving providers greater insight into their patients’ lives. Further, asynchronous telehealth, securely messaging with a provider, may help patients who don’t have reliable access to broadband internet or are too concerned about discrimination or stigma to seek care — granting them greater privacy. The reason patients delay care may not be directly related to their health, but that doesn’t mean the healthcare system is powerless to help.
For all of its destruction, the COVID-19 pandemic helped reveal solutions to another epidemic that’s been going on for much longer. Consider that, in 2019, 33% of households reported delaying care — due to costs alone. With lessons learned, it’s now up to us to remove those barriers that prevent patients from getting the care they need when they need it.