Here's what we'll cover
Here's what we'll cover
Americans feel the high costs of prescription drugs every day. Nearly 30% of adults say they haven’t taken their medication as prescribed in the last year due to cost and two-thirds of adults labeled lowering drug costs an immediate, high priority for the President.
Despite this, it looks as though the ongoing efforts to address these costs in Washington will stall, yet again. After more than a decade of trying to improve the pharmacy experience for patients, I’ve learned that, in the absence of an unlikely industry overhaul, these are the industry secrets that patients should know to avoid sticker shock at the pharmacy.
Secret #1:
The pharmacy business is all about markups; patients should use price comparison tools or shop across local, mail-order, and cash-pay pharmacies to avoid them.
Common generics make up the vast majority of drugs prescribed, and most of these have become increasingly affordable over the past several years. Despite this, the pharmaceutical supply chain has evolved to include so many stakeholders that it fails to pass along all of the cost savings to patients.
Rosuvastatin (Crestor), a common generic medication for high cholesterol, can cost a pharmacy about $0.03 per pill. But pharmacies aren’t just adding a nominal markup when setting a price — it’s far more complicated. Pharmacies consider not only what patients can afford but what they are incentivized to charge based on agreements with Pharmacy Benefit Managers (PBMs). As a result, pharmacies sometimes raise their cash prices to negotiate higher rates from PBMs.
But this isn’t where the price hikes end. PBMs themselves also want to make money, which they do by marking up their price for insurance plans and employers again. The result is that the rosuvastatin that costs the pharmacy $0.03 per pill can be billed to an insurer at up to $2.00 dollars per pill — which is then passed along to patients in rising copays, deductibles, and premiums.
Thankfully, patients can price shop for their prescription drugs (a rare opportunity in healthcare). They may be able to save by using cash-pay, mail-order pharmacies, like Ro Pharmacy, by checking online price comparison tools, or by contacting their local pharmacies to compare prescription options. This process could be the difference between paying $55 or just $15 for a 90 day supply of rosuvastatin.
Secret #2:
Insurance doesn’t always make drugs more affordable; patients should ask about the cash-pay price because paying out-of-pocket can offer savings.
While insurance coverage from an employer can be a valuable benefit, 28% of the time a patient’s copay is more expensive than the cash pay price for a generic drug. How is it possible that even “well-insured” patients are overpaying?
The middlemen in this equation, the PBMs, often obscure the fact that patients might be better off paying cash rather than their copay. PBMs pay pharmacies for their drugs at different rates. But instead of showing patients this menu of prices, they simply make a patient’s copay the same for all pharmacies. For something as affordable as rosuvastatin, this means it’s not uncommon for a copay to be the costlier option. A good rule of thumb for patients is to always compare or ask about the cash-pay price before paying at the pharmacy.
Secret #3:
Insurance plans, not doctors, typically limit prescription supplies to 90 days; patients should look for extended supply options to save money and time.
Patients assume frequent trips to the pharmacy for refills are simply part of their healthcare experience. Yet, in most cases, the practice of limiting drug supplies to 90 days per fill is largely decided by insurance companies’ policies designed to reduce potentially wasted costs on greater supplies of medications. Shorter supply is advantageous to pharmacies too, as it means more transactions and profit per customer, plus greater foot traffic to purchase other items in their stores.
On the other hand, the vast majority of medical professionals believe that extended supply prescriptions, which offer 6 or 12-month supplies of medication per refill, are more convenient and could save patients money. For example, a doctor may decide that an immunocompromised patient, someone living with chronic conditions, or a student away at college is better suited by a 6-month drug supply than the typical 90-day one.
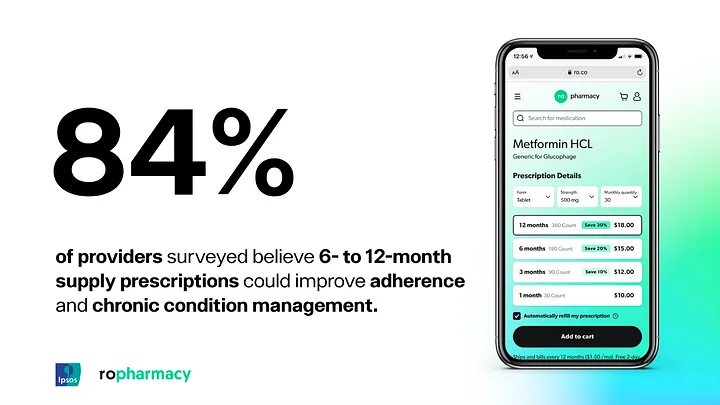
Findings from Ro Pharmacy’s survey with Ipsos.
Buying more of a product often leads to savings per unit, medications are no exception. Patients can save themselves time and money by asking their doctor or pharmacist about extended supply prescriptions. Research shows that doctors and pharmacists are comfortable prescribing them, and many believe that these prescriptions could help patients better stick with and manage their treatment.If patients can understand how these three industry secrets affect their drug costs, and try some of these best practices, they can, hopefully, avoid difficult choices between maintaining their health or making ends meet.