Key takeaways
The hallmark symptoms of genital herpes are inflamed, painful genital or anal lesions.
Genital herpes can look and feel different depending on whether it’s your first infection, or the beginning of an outbreak.
Herpes is not curable, but it is manageable with medications, and you can still have a normal, fulfilling sex life with herpes.
Here's what we'll cover
Here's what we'll cover
Key takeaways
The hallmark symptoms of genital herpes are inflamed, painful genital or anal lesions.
Genital herpes can look and feel different depending on whether it’s your first infection, or the beginning of an outbreak.
Herpes is not curable, but it is manageable with medications, and you can still have a normal, fulfilling sex life with herpes.
Genital herpes is one of the most common sexually transmitted infections (STIs). According to the Centers for Disease Control and Prevention (CDC), 11.9 % of people aged 14 to 49 years have genital herpes. But, since it presents differently in different people and can lie dormant between outbreaks, herpes remains misunderstood by many. In fact, some experts estimate that as many as 90% of infections are undiagnosed.
So, what does genital herpes look like? How do you know if what you’re seeing is genital herpes, or simply a rash? Read on for answers to these questions and more.
What does genital herpes look like?
There are two types of herpes: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). Generally, HSV-1 describes oral herpes (i.e. cold sores) while HSV-2 describes genital herpes, but either HSV-1 or HSV-2 can cause genital herpes, as long as infectious fluids come into contact with your genitals.
Genital herpes is primarily transmitted through sex, including oral sex, as the viral cells enter small breaks or ruptures in the skin. Pregnant women who have genital herpes can also pass herpes on to their child during delivery. The virus lasts not long outside the body and will die within days, even if left on a moist surface.
Genital herpes can create various symptoms for different people, and it can look and feel different depending on whether it’s your first infection, or the beginning of an outbreak. Herpes is characterized by alternating periods where the person is actively shedding the virus through their fluids for 2–3 weeks, called an outbreak, and periods where the infection is dormant. The time between these periods can vary from person to person.
People are most at risk of contracting herpes when a partner is having an active outbreak with symptoms. However, you can still get herpes when a partner is asymptomatic, which is why it’s important to take precautions when you have herpes, such as by wearing condoms and informing your sex partners.
What does the beginning of genital herpes look like?
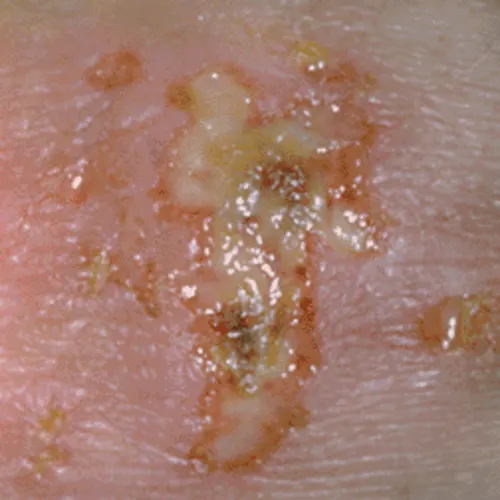
The hallmark symptoms of genital herpes are inflamed, painful genital or anal lesions. These lesions may start as bumps before developing into pus- or fluid-filled sacs and are usually clustered together in a reddish area. Genital herpes may appear anywhere on the genitals and the surrounding area, including the buttocks, upper thighs, and perineum (the skin between your anus and your vulva or scrotum).
Here are a few examples of what the beginning of genital herpes looks like (warning, some may find the images graphic):
The lesions develop about 4–7 days after sexual contact with an infected person, before progressing to blisters, sores, or ulcers, and can last for up to 3 weeks. Hours to days before the lesions appear, you may notice tingling, itching, or burning sensations around your genitals. Additional symptoms of genital herpes may include:
Painful or difficult urination
Swollen lymph nodes that are painful or sore to touch
Flu-like symptoms, such as fever, headache, muscle aches, or fatigue
Swelling of the vulva (in women)
Pelvic pain, pus-like vaginal discharge, or bleeding after sex or between periods due to cervicitis, an inflammation of the cervix (in women)
Rectal pain, bleeding, or discharge due to proctitis, an inflammation of the rectum (in men)
Almost everyone who has a symptomatic outbreak of genital herpes due to HSV-2 will experience active outbreaks again, which are known as recurrences. How frequently these occur, and the symptoms they cause, can vary from person to person. Stress, trauma, fever, UV light, and surgery can all trigger a recurrence of genital herpes.
The first outbreak of genital herpes is typically the most intense. Subsequent episodes are usually less severe, shorter, and can become less frequent with time. Many people may begin to recognize their “prodromal” symptoms, early warning signs of an outbreak that appear hours to days before the genital lesions, which can include burning sensations around the genitals.
What does genital herpes look like when it’s healing?
The symptoms of an active herpes outbreak can last up to three weeks before progressing to the healing stage. Once the sores start to split and crust over, that’s a sign that the genital herpes outbreak is coming to an end. As the outbreak ends, the sores will begin to heal like cuts do.
While a primary genital herpes outbreak may take several weeks to resolve, subsequent outbreaks may heal in 1–2 weeks. Here is another example of herpes in the healing stage.
How can I tell if it’s genital herpes?
Genital herpes can be confused with several other conditions, including:
Fungal or bacterial infection
Rash
Sexual trauma
Pimples
Hemorrhoids
Because of this, the only way to know if you have genital herpes is to have a licensed health professional take a look at it. During your appointment, they might diagnose genital herpes by just looking at any sores that are present. They can also decide to take a swab of your genital lesions and test for herpes, as this can determine which actions you should take moving forward. Your healthcare provider may also recommend urine or blood testing to rule out other STIs, including gonorrhea, chlamydia, and HIV.
If you think you are experiencing a genital herpes outbreak, make an appointment with your healthcare provider as soon as possible. The sooner you are diagnosed, the sooner you can get treatment, and you might be able to shorten an outbreak if you’re acting fast.
Some people have an increased risk of contracting genital herpes. Women, for example, are twice as likely to get genital herpes. Other risk factors for genital herpes include:
Having more sex partners
Participating in oral sex
Having another sexually transmitted infection
Using hormonal contraceptives
Because the currently available tests have a high rate of false-positive results when a person is asymptomatic, the U.S. Preventive Services Task Force does not currently recommend screening for genital herpes.
What treatments are there for genital herpes?
Herpes is not curable, but it is manageable with medications. You can still have a normal, fulfilling sex life with herpes; you just need to take a few precautions to prevent transmitting it to your sex partners.
Generally, the first outbreak will go away within three weeks, even without treatment. However, treatment can relieve the pain and other symptoms, as well as reduce your likelihood of transmitting the infection to others in the future and experiencing subsequent outbreaks. The main treatments for genital herpes include the antiviral medications acyclovir, famciclovir, and valacyclovir. Health providers will recommend different dosage schedules depending on whether it is your first outbreak and the severity of your symptoms.
If you think you might have herpes, the sooner you can make an appointment with a health provider, the better. Early diagnosis is essential for symptom relief and reducing your risk of transmitting herpes to others. Having genital herpes increases your risk of contracting other STIs, including HIV, which is another reason why it’s important to get diagnosed and receive treatment as soon as possible.
To prevent future outbreaks, follow your treatment regimen as prescribed by your healthcare provider. Avoid having sex when you are experiencing an outbreak. To prevent passing herpes to others, inform your sex partners and wear condoms.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Cole, S. (2020). Herpes Simplex Virus: Epidemiology, Diagnosis, and Treatment. The Nursing Clinics of North America, 55(3), 337–345. doi:10.1016/j.cnur.2020.05.004. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0029646520300323?via%3Dihub
Groves, M. J. (2016). Genital Herpes: A Review. American Family Physician, 93(11), 928–934. Retrieved from https://www.aafp.org/pubs/afp/issues/2016/0601/p928.html
Heslop, R., Roberts, H., Flower, D., et al. (2016). Interventions for men and women with their first episode of genital herpes. The Cochrane Database of Systematic Reviews, 2016(8), CD010684. doi:10.1002/14651858.CD010684.pub2. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8502075/
Johnston, C. (2022). Diagnosis and Management of Genital Herpes: Key Questions and Review of the Evidence for the 2021 Centers for Disease Control and Prevention Sexually Transmitted Infections Treatment Guidelines. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, 74(Suppl_2), S134–S143. doi:10.1093/cid/ciab1056. Retrieved from https://academic.oup.com/cid/article/74/Supplement_2/S134/6567958?login=false
Mathew, Jr., J. & Sapra, A. (2023). Herpes Simplex Type 2. StatPearls. Retrieved Oct. 25, 2023 from https://www.ncbi.nlm.nih.gov/books/NBK554427/
McQuillan, G. (2018). Prevalence of herpes simplex virus type 1 and type 2 in persons aged 14–49: United States, 2015–2016. NCHS Data Brief, no 304. Hyattsville, MD: National Center for Health Statistics. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db304.htm
Saleh, D., Yarrarapu, S. N. S., & Sharma, S. (2023). Herpes Simplex Type 1. StatPearls. Retrieved Oct. 25, 2023 from https://www.ncbi.nlm.nih.gov/books/NBK482197/
Sauerbrei, A. (2016). Herpes Genitalis: Diagnosis, Treatment and Prevention. Geburtshilfe und Frauenheilkunde, 76(12), 1310–1317. doi:10.1055/s-0042-116494. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5177552/
US Preventive Services Task Force, Mangione, C. M., Barry, M. J., et al. (2023). Serologic Screening for Genital Herpes Infection: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA, 329(6), 502–507. doi:10.1001/jama.2023.0057. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2801311
Zhu, S. & Viejo-Borbolla, A. (2021). Pathogenesis and virulence of herpes simplex virus. Virulence, 12(1), 2670–2702. doi:10.1080/21505594.2021.1982373. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8923070/










