Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
What is erectile dysfunction and what causes it?
Erectile dysfunction is when you can't develop or maintain a firm erection long enough for satisfying sex. People with ED often deal with embarrassment or stigma around the condition, but it's one of the most common sexual issues. An estimated 52% of American men between ages 40 and 70 deal with ED, although it’s difficult to know the exact numbers (many people are reluctant to talk about ED) (Sooriyamoorthy, 2021).
There are many causes of erectile dysfunction, ranging from physical and mental diseases to drug side effects. One of the leading underlying causes of ED in men of 50 is hardening and narrowing of the arteries, called atherosclerosis. When the blood vessels that supply the penis cannot dilate properly because of atherosclerosis, the penis cannot fill with blood.
That's an obvious downer since erections rely on your ability to pump blood swiftly and reliably to your penis when you need it (Schwartz, 2011). But getting and maintaining an erection involves more than blood vessels, of course. Muscles and nerves are integral to an erection, and they respond to your emotions and hormones. Underlying diseases can cause stress or anxiety that add to erectile problems.
Is there a connection between autoimmune diseases and ED?
The short answer is yes. But the longer answer involves science that's still evolving amid emerging research on the details.
Autoimmune diseases are caused by the immune system attacking your body's organs, tissues, and cells, rather than just defending against infections or injuries. There are dozens of autoimmune diseases, some of which can be challenging to diagnose, many of whose causes remain mysterious. (National Institutes of Health, 2021).
Here's where things get interesting: Atherosclerosis, the chief enemy of erections, is not considered an autoimmune disease, but it shares some of the same root causes with autoimmune diseases (Matsuura, 2014). Further mashing all these concepts together, atherosclerosis is typically caused by some other diagnosable condition, including some autoimmune disorders (Sanjadi, 2018).
Studies point to both direct and indirect connections between autoimmune diseases and erectile dysfunction. Several of the more than 100 known autoimmune diseases are also known causes of ED, either through direct effects on the penis or their other physical and mental impacts:
Type 1 diabetes: ED is common among men with type 1 diabetes, even when young (Maiorino, 2017). It can be caused by damaged nerves or blood vessels or poor blood-sugar control.
Rheumatoid arthritis: Chronic inflammation and pain can affect all aspects of sexual function (Tristano, 2014). In one study, erectile dysfunction was the most commonly reported sexual dysfunction among men with rheumatoid arthritis (El Miedany, 2011).
Multiple sclerosis: This debilitating nervous-system disorder can cause erection problems and other sexual dysfunction through any of a number of means, from fatigue and muscle weakness to worries over incontinence or other psychological effects (Guo, 2012).
Inflammatory bowel disease: In one study, most men with either type of Inflammatory bowel disease (ulcerative colitis or Crohn's disease) suffered erectile dysfunction (Shmidt, 2019).
Lupus: Also called systemic lupus erythematosus, lupus can cause pain and inflammation of the skin, joints, and organs, has only recently been recognized as contributing to significant erectile dysfunction (Campos-Guzmán, 2018).
The physical effects of any of these autoimmune diseases can cause anxiety and stress that can affect your approach and response to sex, worsening any direct physical issues that might make an erection difficult (Mayo Clinic, 2021).
Mysteries surround autoimmunity and possible effects on ED
Understanding autoimmunity and its effects on other conditions and aspects of life, including ED, all have a long way to go.
Increasingly, research suggests that autoimmunity plays a role in Parkinson's disease, which is known to be linked to ED (Lindestam, 2020). Other lesser-known autoimmune diseases, or conditions at least partly related to autoimmunity, can make it difficult to have an erection. Among them:
Transverse myelitis, an inflammation around the spinal cord (Mayo Clinic, n.d.)
Autonomic neuropathy, which damages nerves that control involuntary body functions (Mayo Clinic, n.d.).
There are other diseases that involve less direct connections between autoimmune disorders and erectile dysfunction. For example, having an autoimmune disorder like lupus is one of several risk factors for Peyronie's disease, in which scar tissue develops on the penis, causing painful erections and erectile dysfunction (Tunuguntla, 2001; Cleveland Clinic, 2020).
Meanwhile, the problem of autoimmunity appears to be increasing in the United States, based on a study of more than 14,000 people 12 and older starting in the late 1980s up through 2012.
Increases were most pronounced in men, men and women 50 and older, non-Hispanic white people, and, most especially and alarmingly, adolescents. The research does not indicate why, but the scientists suspect changes in the environment or lifestyles are at work (Dinse, 2020).
Treatment of ED in association with autoimmune disease
If erectile dysfunction has got you down, and you suspect you have an autoimmune disorder or some other medical condition, seek medical advice on any possible connection. ED is often underrecognized and undertreated when it's part and parcel with another potentially serious disease like an autoimmune disorder.
Even if you don’t suspect that you have an autoimmune disease, it's wise to consult with a healthcare provider to make sure there isn't some underlying condition for your ED you're just not aware of yet.
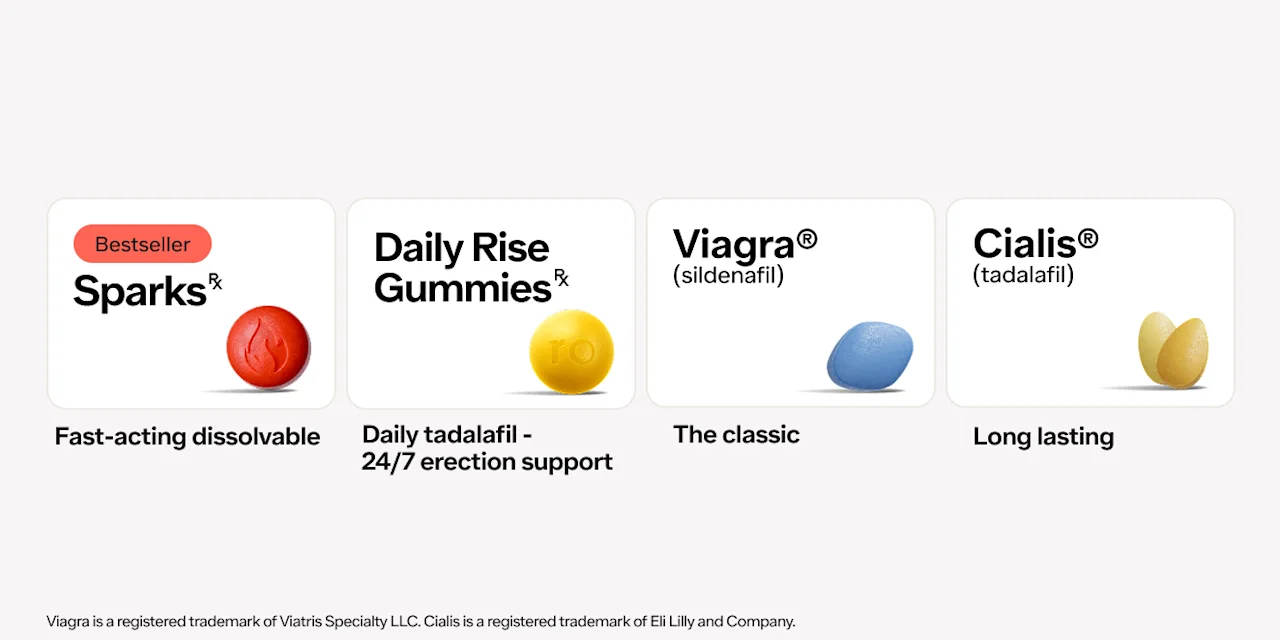
Oral prescription medications for ED are highly effective. Several are available, including Viagra (sildenafil), Cialis (tadalafil), and Levitra (vardenafil). These pills are part of a family of drugs called phosphodiesterase type 5 (PDE5) inhibitors that help get stronger and longer lasting erections. Whether you seek a prescription or not, you might also try some tried and true ED remedies that don't require any medical intervention (Maiorino, 2015):
Engage in more physical activity.
Eat more whole-grain foods, legumes, and vegetables, and fruits.
Avoid alcohol and smoking.
Any of these lifestyle changes can make you healthier overall and help battle disease, and they just might improve your sex life in more ways than one, from righting your erections to giving you more energy and stamina to make use of them.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
American Autoimmune Related Diseases Association (n.d.) Autoimmune Disease List https://autoimmune.org/disease-information/
Campos-Guzmán J, Barrera-Vargas A, Gómez-Martín D, Alcocer-Varela J, Govea-Peláez S, Gómez-Sámano MA, Cuevas-Ramos D, Padilla-Ortíz DM, Merayo-Chalico J. Men and Sexual Function: An Overlooked Issue in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 10). Retrieved from https://acrabstracts.org/abstract/men-and-sexual-function-an-overlooked-issue-in-systemic-lupus-erythematosus/
Cleveland Clinic (2018) Erectile Dysfunction https://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/endocrinology/erectile-dysfunction/
Cleveland Clinic (2020) Peyronie's Disease https://my.clevelandclinic.org/health/diseases/10044-peyronies-disease
Dinse GE, Parks CG, Weinberg CR, Co CA, Wilkerson J, Zeldin DC, Chan EKL, Miller FW. Increasing Prevalence of Antinuclear Antibodies in the United States. Arthritis Rheumatol. 2020 Jun;72(6):1026-1035. doi: 10.1002/art.41214. Epub 2020 Apr 30. PMID: 32266792; PMCID: PMC7255943. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32266792/
El Miedany Y, El Gaafary M, El Aroussy N, Youssef S, Ahmed I. Sexual dysfunction in rheumatoid arthritis patients: arthritis and beyond. Clin Rheumatol. 2012 Apr;31(4):601-6. doi: 10.1007/s10067-011-1891-2. Epub 2011 Nov 24. PMID: 22108779. Retrieved from https://pubmed.ncbi.nlm.nih.gov/22108779/
Guo ZN, He SY, Zhang HL, Wu J, Yang Y. Multiple sclerosis and sexual dysfunction. Asian J Androl. 2012;14(4):530-535. doi:10.1038/aja.2011.110. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3720075/
Lindau, S. T., Schumm, L. P., Laumann, E. O., Levinson, W., Omuircheartaigh, C. A., & Waite, L. J. (2007). A Study of Sexuality and Health among Older Adults in the United States. New England Journal of Medicine, 357(8), 762–774. doi: 10.1056/nejmoa067423, https://www.ncbi.nlm.nih.gov/pubmed/17715410
Lindestam Arlehamn, C.S., Dhanwani, R., Pham, J. et al. α-Synuclein-specific T cell reactivity is associated with preclinical and early Parkinson’s disease. Nat Commun 11, 1875 (2020). https://doi.org/10.1038/s41467-020-15626-w. Retrieved from https://www.nature.com/articles/s41467-020-15626-w
Maiorino, M., Bellastella, G., Della Volpe, E. et al. Erectile dysfunction in young men with type 1 diabetes. Int J Impot Res 29, 17–22 (2017). https://doi.org/10.1038/ijir.2016.38. Retrieved from https://www.nature.com/articles/ijir201638
Maiorino MI, Bellastella G, Esposito K. Lifestyle modifications and erectile dysfunction: what can be expected?. Asian J Androl. 2015;17(1):5-10. doi:10.4103/1008-682X.137687. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4291878/
Matsuura E, Atzeni F, Sarzi-Puttini P, Turiel M, Lopez LR, Nurmohamed MT. Is atherosclerosis an autoimmune disease?. BMC Med. 2014;12:47. Published 2014 Mar 18. doi:10.1186/1741-7015-12-47. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3984678
Mayo Clinic (2021) Erectile dysfunction https://www.mayoclinic.org/diseases-conditions/erectile-dysfunction/symptoms-causes/syc-20355776
Mayo Clinic (2021) Erectile dysfunction and diabetes https://www.mayoclinic.org/diseases-conditions/erectile-dysfunction/in-depth/erectile-dysfunction/art-20043927
Mayo Clinic (n.d.) Autonomic neuropathy https://www.mayoclinic.org/diseases-conditions/autonomic-neuropathy/symptoms-causes/syc-20369829
Mayo Clinic (n.d.) Transverse myelitis https://www.mayoclinic.org/diseases-conditions/transverse-myelitis/symptoms-causes/syc-20354726
National Institutes of Health (2021) Autoimmune Diseases https://www.niehs.nih.gov/health/topics/conditions/autoimmune/index.cfm
Sanjadi, M., Rezvanie Sichanie, Z., Totonchi, H., Karami, J., Rezaei, R., & Aslani, S. (2018). Atherosclerosis and autoimmunity: a growing relationship. International journal of rheumatic diseases, 21(5), 908–921. Doi: 10.1111/1756-185X.13309. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/29671956/
Schwartz, B. G., & Kloner, R. A. (2011). Cardiology patient page: cardiovascular implications of erectile dysfunction. Circulation, 123(21), e609–e611. Doi: 10.1161/CIRCULATIONAHA.110.01768. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/21632512/
Shmidt E, Suárez-Fariñas M, Mallette M, Moniz H, Bright R, Shah SA, Merrick M, Shapiro J, Xu F, Saha S, Sands BE. Erectile Dysfunction Is Highly Prevalent in Men With Newly Diagnosed Inflammatory Bowel Disease. Inflamm Bowel Dis. 2019 Jul 17;25(8):1408-1416. doi: 10.1093/ibd/izy401. PMID: 30861068. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30861068/
Sooriyamoorthy T, Leslie SW. (2021). Erectile Dysfunction. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK562253/
Tristano AG. Impact of rheumatoid arthritis on sexual function. World J Orthop. 2014;5(2):107-111. Published 2014 Apr 18. doi:10.5312/wjo.v5.i2.107. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017303/
Tunuguntla H. S. (2001). Management of Peyronie's disease - a review. World journal of urology, 19(4), 244–250. Doi: 10.1007/s003450100209. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/28386796/