Here's what we'll cover
Here's what we'll cover
No one wants to hear the c-word—cancer. However, the reality is that prostate cancer is a common occurrence. One thing you’ll hear after a diagnosis is the prostate cancer stage and grade. But what do those terms mean, and what they mean for your treatment options and prognosis? Read on to learn more.
What is prostate cancer?
Prostate cancer (the technical term is prostate adenocarcinoma) is the most common non-skin cancer affecting men in the United States. It is estimated that 11% of men will be diagnosed with prostate cancer at some point in their lives and 2.5% will die from it (Jain, 2021).
The prostate gland is about the size of a walnut, and sits at the base of the bladder in front of the rectum. Its main job is to make prostatic fluid that helps keep your sperm healthy.
In prostate cancer, abnormal cells begin slowly growing in the peripheral zone of the prostate gland (that’s the part that runs along the back and side of the gland). If undetected, cancer may grow and spread beyond the prostate gland via three potential routes:
Growing into adjacent tissues (invasion)
Spreading through the lymph nodes into the lymph system
Traveling in the bloodstream to distant tissues, like bone, lung or liver (metastasis)
If your healthcare provider suspects prostate cancer, you will need a prostate biopsy. During this procedure, a small sample of prostate cells from the tumor is removed and evaluated under a microscope. This biopsy, along with other tests like ultrasound, CT, MRI, etc. will help establish the grade and stage of your cancer to determine the best course of treatment.
Prostate cancer stages
Prostate cancer stage refers to the size of the tumor and whether or not the cancer has spread. It helps not only guide treatment, but also helps you and your healthcare provider have more complete discussions about survival rates.
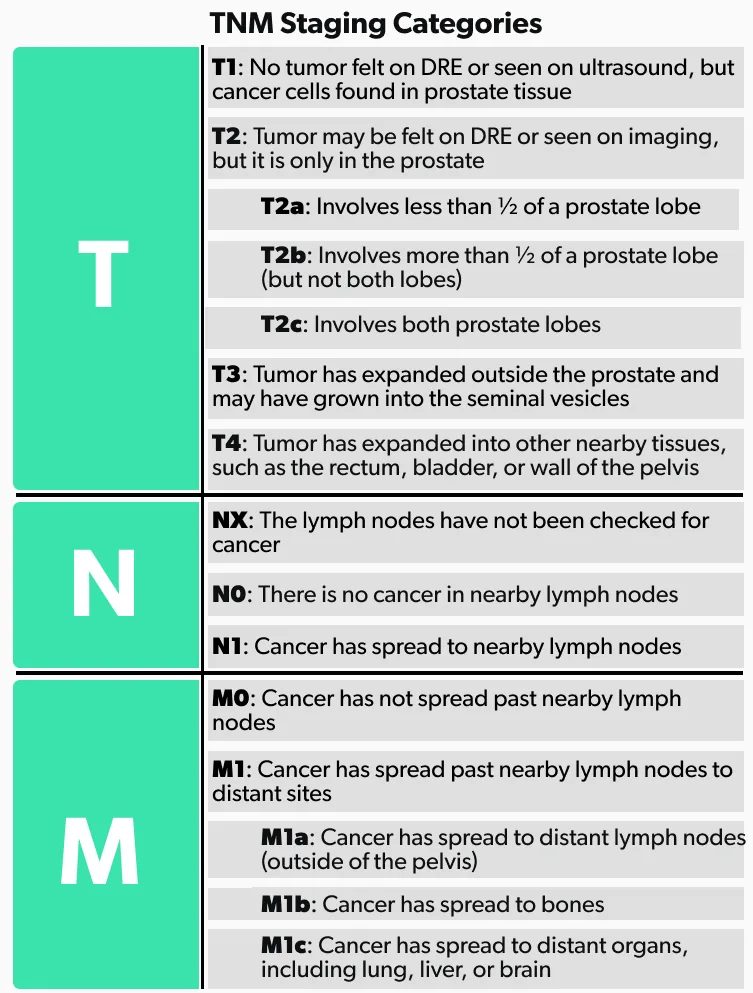
The most common staging system for prostate cancer is the one used by the American Joint Committee of Cancer (AJCC), also known as the TNM system. There are five data points used to come up with the overall stage (Rosen, 2021):
Tumor size (T category—T for tumor)
If the cancer has spread to lymph nodes (N category—N for nodes)
If the cancer has spread or metastasized to other parts of the body (M category—M for metastasis)
The PSA level at the time of diagnosis
The Gleason score or Grade Group
Let’s take a closer look at the different components that go into prostate cancer staging.
TNM staging categories
The TNM staging system is used to determine the cancer stage for most solid tumors. It is based on the tumor size (T), lymph node involvement (N), and spread to other tissues or metastasis (M). Here is a breakdown of the TNM stages in prostate cancer.
PSA levels
Prostate cancer screening typically involves a blood test that measure your prostate-specific antigen (PSA) levels. PSA is a protein made by cells in the prostate gland. Anything that causes a problem in the prostate can release more PSA into the blood stream. Also, as you age, your body releases more PSA naturally (David, 2021).
For this reason, the “normal” range of PSA levels varies based on age; it is lower in people in their 40s and highest once you hit your 70s. High PSA levels do not necessarily mean you have cancer, but they are taken into consideration when it comes to staging prostate cancer (David, 2021).
If you have a PSA level greater than 4.0 ng/ml, your healthcare provider will likely recommend more testing, like a digital rectal exam (DRE) and imaging tests (like MRI, ultrasound, etc.) to look for potential prostate cancer. It’s important to know that you can have an elevated PSA and not have prostate cancer, and you can have a PSA level less than 4.0 ng/ml and have cancer. This is why PSA levels alone are not enough for diagnosing or staging prostate cancer (David, 2021).
Prostate cancer Gleason score or grade
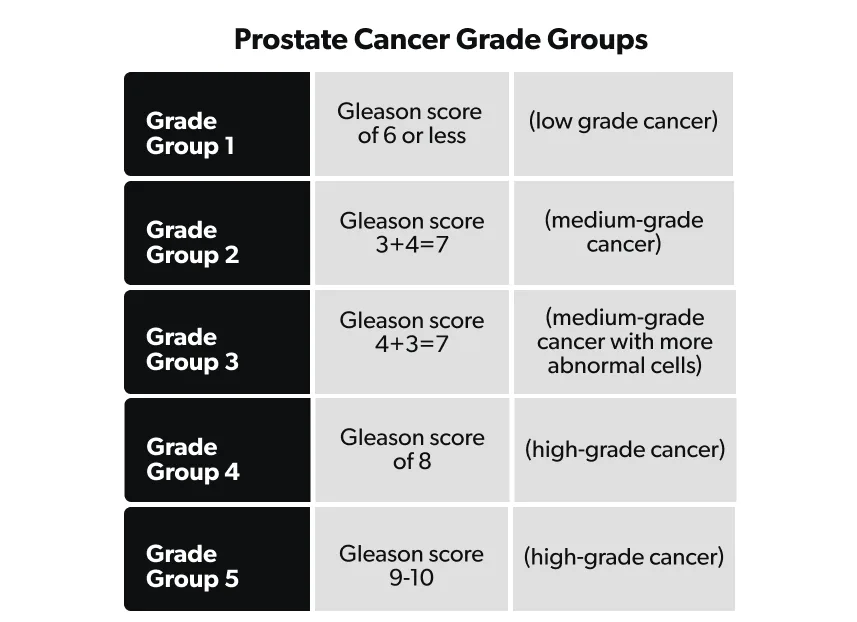
Prostate cancer grading is based on the appearance of the tumor cells (obtained from a needle biopsy of the prostate) under the microscope. Low-grade cancer cells look more like healthy cells than do high-grade cells. The two methods used to measure prostate cancer grade are the Gleason score or Grade Group.
While examining the tumor cells, the pathologist looks at the two most common tumor cell patterns, referred to as the primary (the most common) and secondary (the second most common) patterns. Each of these patterns is then graded based on how closely they resemble normal prostate tissue (Leslie, 2021).
Grade 1 cells look like normal prostate cells. Grade 5 cells are very abnormal appearing cells. Grades 2–4 are in between; the higher the number, the less the cells look like normal prostate tissue. Almost all prostate cancers have grade 3 cells or higher.
Once the pathologist has assigned a grade to the primary and secondary cell patterns, these two numbers are added together to get a total Gleason score. The higher the Gleason score, the more likely the tumor is going to grow or spread to other parts of the body.
Since the lowest grade a cancer cell can have is grade 3 (grades 1 and 2 are rarely used when describing cancerous tissue), the lowest Gleason score for a cancer is grade 6 (total of the primary and secondary scores) and is considered low-grade prostate cancer.
Many experts use the Gleason score to categorize prostate cancers into “Grade Groups”—these are also assigned a number, ranging from 1 to 5, with 1 being the least likely to grow and 5 being the most likely to grow. For example, if your primary Gleason score is 3 and your secondary score is 4, then you are a Grade Group 2. Alternatively, if the primary pattern is a Gleason score 4 (higher grade cancer cell) and the secondary pattern is a 3, then you are Grade Group 3 (an overall higher cancer grade) (Epstein, 2016).
What’s the difference between cancer grading and staging?
Cancer (or tumor) grade refers to how quickly it may grow or spread. Cancer stage refers to the size of the tumor and whether or not it has already spread to other parts of the body. For the most part, the lower the grade, the slower the growth of the tumor. In contrast, stages mean different things for different types of cancer, but usually the higher the number, the more advanced the cancer (Rosen, 2021).
Now, let’s put all of this information together and talk about the different stages of prostate cancer.
Stage 1 prostate cancer
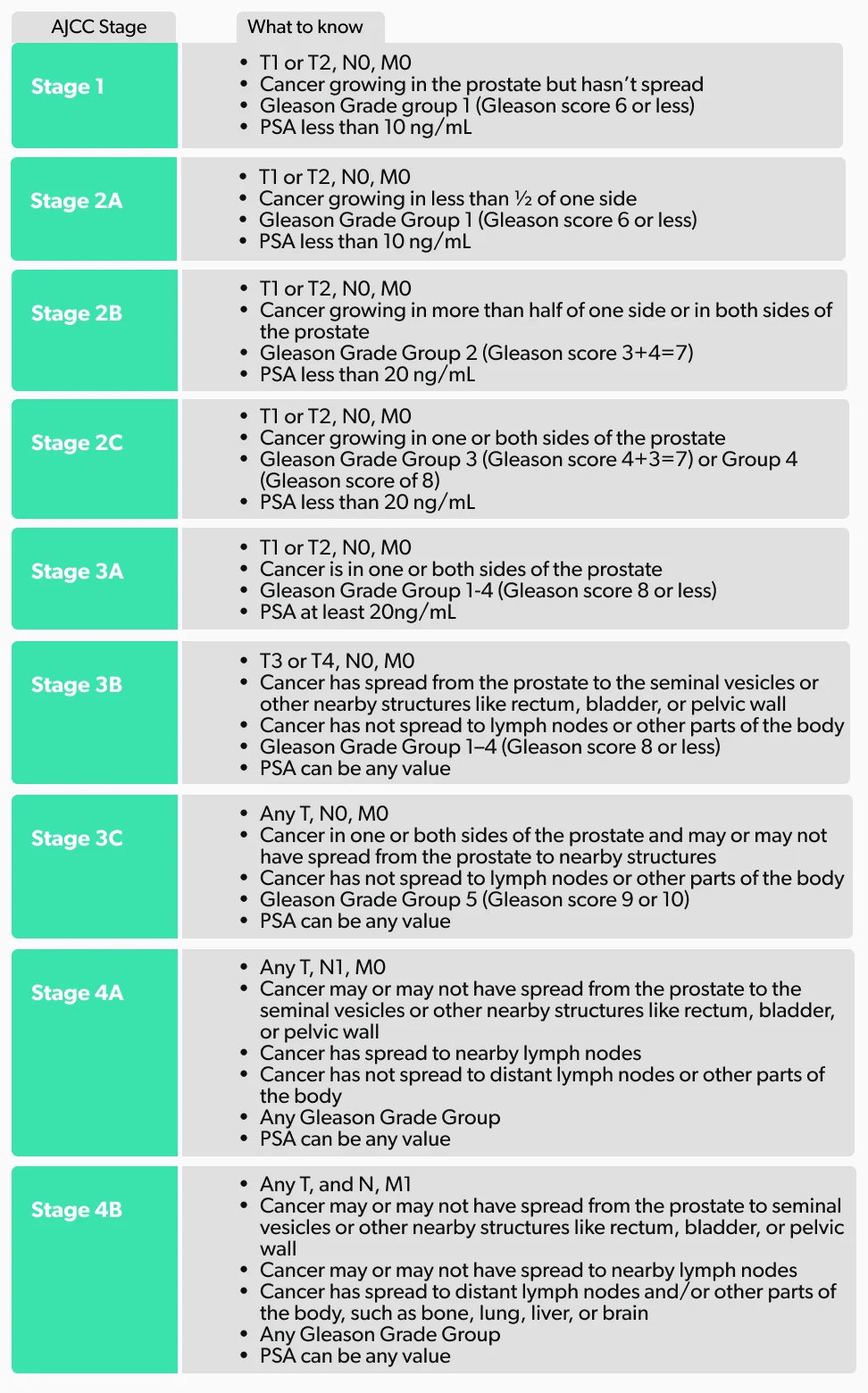
Stage 1 is early-stage prostate cancer and means that the cancer is small, only in the prostate, and contains low grade cancer cells. It’s also called localized prostate cancer. By the TNM system, it is T1 (or T2), N0, M0 and the Gleason group grade 1. Typically, it will have a PSA level of less than 10 ng/ml (Xiao, 2017).
According to the American Cancer Society, the survival rate of localized prostate cancer is excellent, with almost 100% of people still alive five years after their diagnosis (ACS, 2021).
Treatment
Prostate cancer treatments come with side effects, and you will need to talk to your healthcare provider about the risks and benefits to decide on the best treatment for you. Many factors come into play when deciding on treatment, include your age, health, cancer stage, and risks of therapy. Treatment options for stage 1 prostate cancer include (Rosario, 2021):
Active surveillance—Your provider follows you over time with regular physical exams, PSA tests, MRIs, and/or repeat prostate biopsies. You would only undergo treatment if there are signs that your prostate cancer is progressing.
Watchful waiting—If you are elderly and have no symptoms, then your stage 1 prostate cancer is not likely to cause problems in your lifetime. The goal with watchful waiting is to keep an eye out for any concerning symptoms and address them as they arise.
Surgery: In some cases, surgery is recommended. During surgery, also called a radical prostatectomy, your surgeon removes the entire prostate gland, plus some of the tissue around it.
Radiation therapy—External beam and brachytherapy radioactive seed placement are two different types of radiation therapy that can treat prostate cancer.
Focal therapy—These treatment options act to treat the tumor directly without affecting the surrounding tissues. Focal therapy includes cryotherapy (freezing the cancer), laser therapy, and high-intensity focal ultrasound (HIFU).
Stage 2 prostate cancer
Stage 2 prostate cancer is when the cancer is growing entirely within the prostate; T1 or T2, N0, M0. Even though the cancer cells in this stage are higher grade than the ones in Stage 1, it is still considered localized prostate cancer. This stage 2 is further divided into three subgroups based on the characteristics of the cancer cells found on biopsy (Gleason grade group) and PSA levels (Xiao, 2017):
Stage 2A—Cancer cells take up less than half of one side of the prostate (T2a); Gleason grade group 1 (Gleason score 6 or less); PSA less than 10 ng/ml
Stage 2B—Cancer cells present in more than half of one side or in both sides of the prostate (T2b); Gleason grade group 2 (Gleason score 7 [3+4]); PSA is less than 20 ng/ml
Stage 2C—Cancer cells present in one or both sides of the prostate (T2c); Gleason grade group 3 or 4 (Glease score 7 [4+3] or 8); PSA is less than 20 ng/ml
Treatment
Since stage 2 is considered localized prostate cancer, the treatment options are similar to stage 1 and include (Rosario, 2021):
Active surveillance
Watchful waiting
Surgery
Radiation therapy
Focused therapy
Stage 3 prostate cancer
Stage 3 prostate cancer is an advanced stage that is still localized to the area of the prostate. It does not involve the lymph nodes (N0) and has not metastasized to distant sites (M0). People with Gleason scores of 8 or more have a lower 15-year survival rate than those with lower cancer grades. Stage 3 is further divided into subgroups based on the extent and grade of the cancer (Xiao, 2017):
Stage 3A—Cancer is in one or both sides of the prostate (T1 or T2); Gleason grade group 1–4 (Gleason score 8 or less); PSA levels at least 20 ng/ml
Stage 3B—Cancer has spread from the prostate to the seminal vesicles or other nearby structures like the rectum, bladder, or pelvic wall (T3 or T4); Gleason grade group 1–4; any PSA level
Stage 3C—Cancer is in one or both sides of the prostate and may or may not have spread to nearby structures; Gleason grade group 5 (Gleason score 9–10), meaning the cells look very abnormal; any PSA level
Treatment
The treatment options for stage 3 overlap with lower stages, and it is important to discuss the risks and benefits of treatments with your healthcare provider. Options may be combined, and include (Leslie, 2021):
Active surveillance
Watchful waiting
Hormone therapy—This treatment lowers the level of male hormones (androgens) in the body so they can’t encourage prostate cancer growth. Another name for this treatment is androgen deprivation therapy (ADT). Hormone therapy is often combined with radiation therapy for better results.
Radiation therapy
Surgery
Stage 4 prostate cancer
Stage 4 prostate cancer is the most advanced stage and means that the cancer has spread from the prostate to lymph nodes and/or distant sites like bones, lungs, liver, or brain. Prostate cancers with distant metastases have an overall survival rate of about 30%. Stage 4 is further divided into subgroups based on how far away the cancer has spread (Leslie, 2021):
Stage 4A—Cancer has infiltrated the nearby (not distant) lymph nodes (N1); it has not spread to distant sites (M0) and the cancer cells are any Gleason grade group; any PSA level
Stage 4B—Cancer has infiltrated the distant lymph nodes and/or sites like the bones, lungs, or brain (M1); cancer cells are any Gleason grade group; any PSA level
Treatment
Since this is the most advanced stage of prostate cancer with the poorest prognosis, treatment will vary depending on several factors like your age, health, and the side effects of the treatments. Active surveillance and watchful waiting are certainly options for people who do not wish to pursue active treatment of the cancer. Other options include (Leslie, 2021):
Hormone therapy
Chemotherapy—This is a prostate cancer treatment that uses anti-cancer drugs to stop the growth of cancer cells. Your provider may recommend chemotherapy alone, or in combination with other treatments.
Radiation therapy
Surgery
What do staging and grading mean for you?
You may be wondering why you need all of this information and whether this “alphabet soup” is really necessary.
It’s important to understand the staging and grading of your (or your loved one’s) cancer, as these help you and all of your healthcare providers choose which treatment path is best for your particular situation. However, staging is not the only information your healthcare providers need. Your symptoms, age, life expectancy, and personal preferences should be taken into consideration when deciding on treatment.
Deciding on treatment necessarily involves a discussion between you and your healthcare provider, but it also includes the input of multiple specialists. Depending on your stage, a medical oncologist (cancer specialist), a radiation oncologist (also a cancer specialist), and a urologist (urinary and male reproductive system specialist) may be involved in the decision-making process.
Here’s a recap:
How do prostate cancer stages & grades affect survival rates?
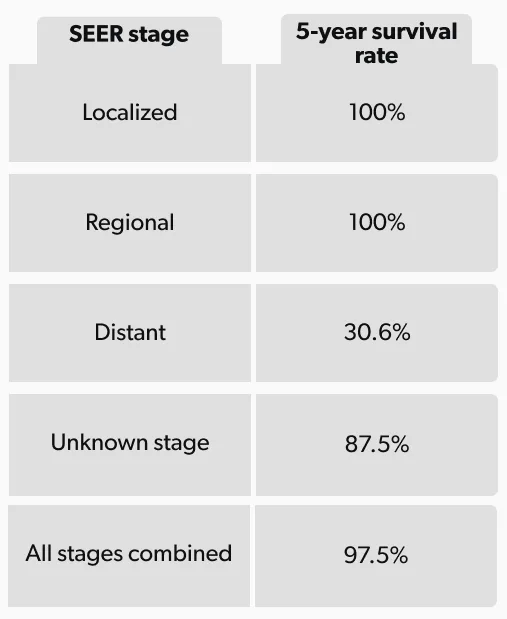
Overall, the prostate cancer survival rate is 97.5%—most men will not die of prostate cancer, even if they have it until the end of life. However, if you look at survival rates by stage, it has been shown that the more advanced forms of prostate cancer have a lower survival rate (NCI, n.d.).
The National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results Program (SEER), which is the database that compiles the incidence and survival rates, sorts prostate cancer into localized, regional, and distant rather than using the TNM system (NCI, n.d.):
Localized—Cancer has not spread outside of the prostate (Stage 1, 2, and some stage 3 cancers)
Regional—Cancer has spread outside of the prostate to adjacent structures and lymph nodes (Stage 3B and 4A cancers)
Distant—Cancer has spread to remote parts of the body, such as bones, liver, or lungs (Stage 4B cancers)
Here are the 5-year relative survival rates for men with prostate cancer based on the SEER database information (NCI, n.d.):
Being diagnosed with cancer can be difficult for both you and your loved ones. There is a great deal of information available about staging, survival rates, treatments, etc. Talking to your healthcare providers about your cancer can help you translate the “alphabet soup” into an actionable plan.
It is important to remember that cancer affects each person differently; doctors have guidelines to follow, but no single treatment plan works best for everyone. Work as a team with your healthcare provider to come up with the best strategy for you to manage your prostate cancer.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
American Cancer Society(ACS). (2021).Survival rates for prostate cancer. Retrieved on Nov. 10, 2021 from https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/survival-rates.html
David, M. K. & Leslie, S. W. (2021). Prostate-specific antigen. [Updated May 9, 2021]. In: StatPearls [Internet]. Retrieved on Nov. 10, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK557495/
Epstein, J. I., Egevad, L., Amin, M. B., Delahunt, B., Srigley, J. R., Humphrey, P. A., & Grading Committee. (2016). The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. The American Journal of Surgical Pathology , 40(2), 244–252. doi: 10.1097/pas.0000000000000530. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26492179/
Jain, M. A. & Sapra, A. (2021). Prostate cancer screening. [Updated Oct. 9, 2021]. In: StatPearls [Internet]. Retrieved on Nov. 10, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK556081/
Leslie, S. W., Soon-Sutton, T. L., Sajjad, H., et al. (2021). Prostate cancer. [Updated Sept. 17, 2021]. In: StatPearls [Internet]. Retrieved on Nov. 10, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK470550/
National Cancer Institute - Surveillance, Epidemiology, and End Results Program. (n.d.). Cancer Stat Facts: Prostate Cancer. Retrieved on Nov. 10, 2021 from https://seer.cancer.gov/statfacts/html/prost.html
Rosario, E. & Rosario, D. J. (2021). Localized prostate cancer. [Updated Oct. 1, 2021]. In: StatPearls [Internet]. Retrieved on Nov. 10, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK563248/
Rosen, R. D. & Sapra, A. (2021). TNM Classification. [Updated Feb. 23, 2021]. In: StatPearls [Internet]. Retrieved on Nov. 10, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK553187/
Xiao, W. J., Zhu, Y., Dai, B., & Ye, D. W. (2017). Evaluation of the major changes in eighth edition of the American Joint Committee on Cancer pathological staging for prostate cancer treated with prostatectomy. PloS One , 12(11), e0187887. doi: 10.1371/journal.pone.0187887. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5679543/












