Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Few things can have such a strong immediate and long-term impact on your overall wellness as trouble sleeping.
Missing just one good night’s sleep can leave you exhausted the next day and begin a slew of bad habits that cause a further lack of sleep. If you routinely wake up at night, toss and turn, struggle to get back to sleep, or otherwise just can’t seem to get enough sleep, you may have a common sleep problem.
Fortunately, sleep problems can often be traced to lifestyle habits or treatable sleep disorders such as chronic insomnia, sleep apnea, or a range of other medical conditions and mental health issues.
Read on to learn about several well-researched strategies for improving sleep habits to increase the hours of sleep you get and improve the quality of your sleep––without the risks and side effects of sleep medicine.
How much sleep do you need?
Sleep needs change with age and vary by person. Still, most adults need at least seven hours of shut-eye each night to best support physical and mental well-being, according to the American Academy of Sleep Medicine and the Sleep Research Society (Watson, 2015).
Sleep is vital to organize thoughts and consolidate memories, according to theory. In short, the things we experience during the day are thought to get encoded in the brain. During sleep, those experiences seem to be reactivated and integrated into long-term memory (Rasch, 2013).
Some important trash disposal happens while we sleep, too. While we snooze, a web of blood vessels around the brain, called the glymphatic system, is thought to collect a protein called amyloid-beta and other garbage of the noggin. If left to build up, these substances can clog the brain and reduce its efficiency (Shokri-Kojori, 2018).
Research going back several decades has demonstrated that poor sleep raises the risk of several serious physical and mental health problems, including depression, high blood pressure, heart attack, stroke, and diabetes (Colten, 2006).
A study of 2,500 adults found that those who had trouble falling asleep were at higher risk 14 years later for cognitive impairment, including issues with language, memory, and overall thinking ability (Zaheed, 2021).
Yet many people, young and old, struggle to get a good night’s sleep. Here’s how many Americans regularly don’t get enough sleep (United States Department of Health and Human Services-a, 2021):
Children: 34.1% (HHS-b, 2021)
High schoolers: 74.6% (HHS-c, 2021)
Adults: 32.5% (HHS-d, 2021)
Common sleep problems
Sleep is governed by our internal biological clock, known as the circadian rhythm. Through eons of evolution, the clock helps us sleep at night and be alert during the day.
When it’s all properly set, darkness triggers the body’s release of the hormone melatonin, which makes us sleepy, and bright daylight suppresses melatonin (National Center for Complementary and Integrative Health, 2021).
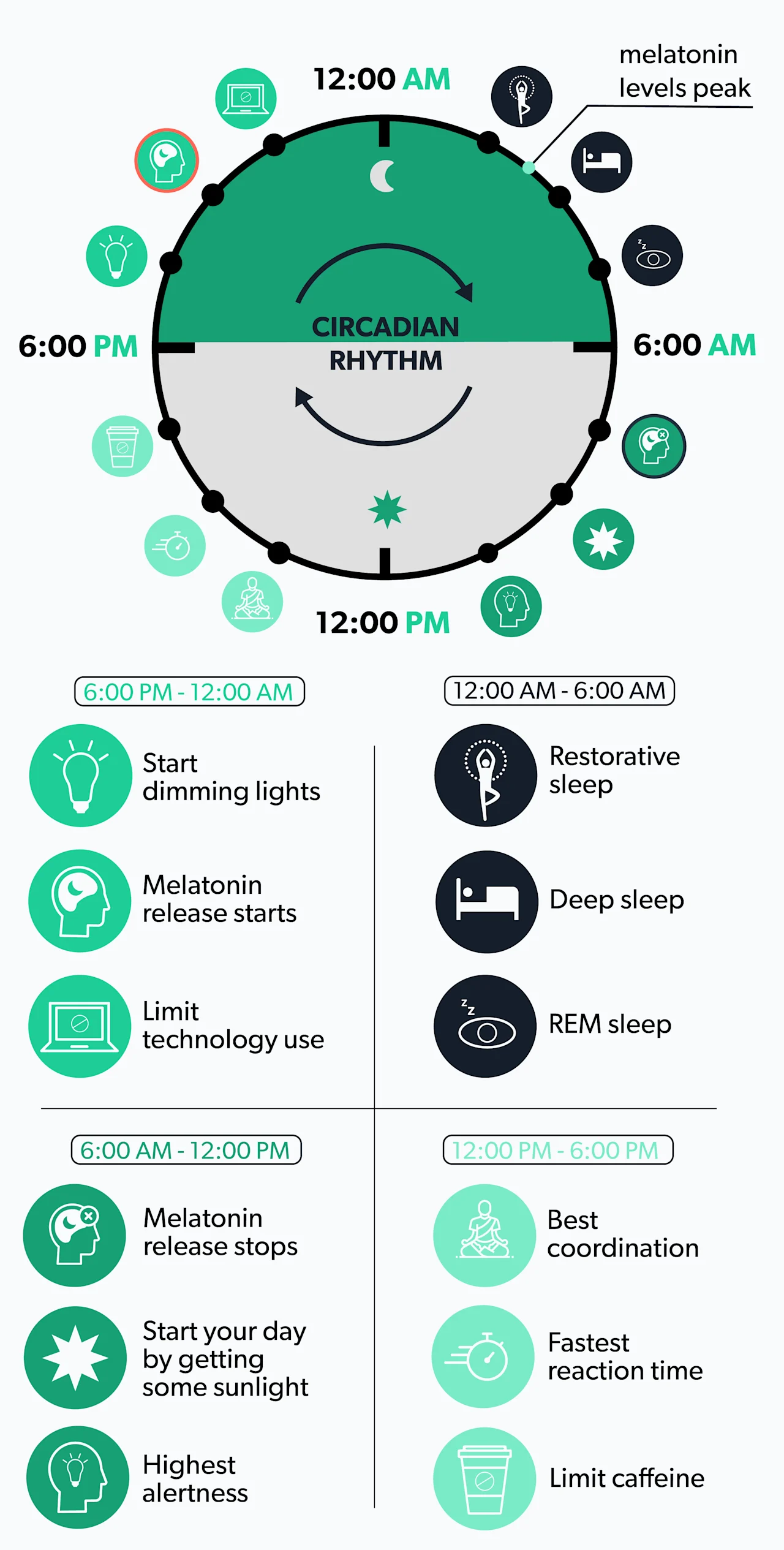
But many things can interfere with our circadian rhythms, including the lack of broad daylight many people experience in modern life (Killgore, 2020). No surprise, then, that people who get more daylight during the day sleep better at night (Figueiro, 2017).
If you spend ample time outside, your trouble sleeping might instead be due to anxiety and stress, alcohol in excess, tobacco, caffeine, and certain medications (Winkelman, 2021).
Persistent sleep problems can leave you tired during the day, which can lead to compensating with unhealthy habits, like sugary snacks, too much coffee, and lack of exercise––all of which can hamper sleep, creating a vicious cycle.
Sleep disorders
You might be surprised to learn there are 60 distinct sleep disorders, as determined by the American Academy of Sleep Medicine's International Classification of Sleep Disorders publication. They fall into several categories (UpToDate, 2021):
Insomnia (which can be short-term or chronic)
Sleep-related breathing disorders (including sleep apnea)
Central disorders of hypersomnolence (such as daytime sleepiness, narcolepsy)
Circadian rhythm sleep-wake disorders (often related to shift work or frequent jet lag)
Parasomnias (persistent, undesirable actions like sleep talking, sleepwalking, or sleep terrors)
Sleep-related movement (restless legs syndrome and other movements or cramps)
People who work night shifts or otherwise toil well outside a 9–5 schedule can suffer shift work sleep disorder (SWSD), in which their natural circadian rhythm is disrupted. Much research has shown that night-shift workers are at greater risk for sleeping problems, weakened immune systems, and a range of ensuing diseases (Jehan, 2017).
Sleep disorders can be diagnosed when the problem is persistent, and some of these common symptoms dog you frequently and affect your quality of life :
Feeling sleepy, irritable, or emotional during the day
Struggling to stay awake when still, such as while reading or watching TV
Feeling tired or fall asleep while driving
Struggling to concentrate or are slow to react
Feeling like napping every day
Relying on caffeine to keep you going
Other people often saying you look tired
Helpful remedies and tips for better sleep
Physical activity during the day (not just before bedtime) is one of the best ways to foster good sleep at night, which can positively affect the desire to exercise (Dolezal, 2017).
A healthy diet can also improve sleep, though the findings on this front are complex and scattered so much as to make specific recommendations similarly complex (Frank, 2017).
And there are several other proven ways to help solve many common sleep problems with proper sleep hygiene (Irish, 2015):
Set a regular sleep schedule and stick to it.
Limit consumption of alcohol, nicotine, and caffeine.
Make your bedroom a cool, quiet, and dark place (earplugs or a white-noise app can help).
Create a relaxing routine, perhaps with soothing music or a good book.
Avoid stressful activities in the evening, including social media and work stuff.
Turn off screens at least an hour before bedtime.
Avoid naps.
A hot bath an hour or so before bedtime, around 104–109 degrees, helps people fall asleep faster and sleep better (Haghayegh, 2019).
Be wary of sleep medicines
When needed for sleep disorders, there are helpful sleep medications that can be a vital part of treatment if prescribed by doctors after a diagnosis (American Academy of Sleep Medicine, n.d.).
But if you dream of a magical over-the-counter sleeping pill or liquid that will leave you refreshed after a night of great sleep, consider these warnings (Culpepper, 2015):
Ironically, sleep medications can leave you drowsy and confused the next day. Depending on the type of medication, other side effects can include dry mouth, blurred vision, and dizziness.
According to a review of randomized controlled studies, over-the-counter sleep medications “lack robust clinical evidence supporting efficacy and safety.”
Sleep aids can be helpful if you’re recovering from a medical procedure, just traveled across time zones, or for other specific, short-term situations. Still, they cannot cure insomnia and can worsen your sleep problems if taken over the long term.
Also, some sleep aids can potentially interact negatively with other medications, conditions, or lifestyle factors. It’s best to see a doctor before taking any of them. And among the many sleep medications––including benzodiazepines, antidepressants, antihistamines, and anxiolytics––there’s a risk of cognitive impairment and dependence or addiction (Xie, 2017).
What about melatonin supplements?
When used as directed, melatonin supplements are among the few sleep aids that some researchers consider potentially effective with few side effects.
A melatonin supplement can help reset the circadian rhythm and improve the onset, duration, and quality of sleep. This can be especially helpful after middle age since melatonin levels tend to decrease in older adults. Melatonin is approved in Europe for managing insomnia in people over age 55 (Xie, 2017).
A review of clinical trials concluded that while more research is needed, melatonin supplements can also effectively treat sleep problems in various other groups, including shift workers, children with autism spectrum disorders, children with attention-deficit/hyperactivity disorder, and adolescents with depression (Xie, 2017).
But the American Academy of Sleep Medicine advises caution on melatonin. While it may be helpful for shift workers or people with jet lag, it should not be used to treat chronic insomnia, the group says (American Academy of Sleep Medicine, 2021).
There’s also the problem of not knowing what you’re getting with a supplement, which is not regulated in the manner of FDA-approved medicines. In examining 30 commercial melatonin supplements, more than 70% of them had more than 10% inaccurate ingredients compared to what the labels stated (Erland, 2017).
“Melatonin isn’t a ‘one-size-fits-all solution to nightly sleep trouble,” said Jennifer Martin, Ph.D., a professor of medicine at UCLA and a member of the AASM board of directors.
“People who have difficulty sleeping should try making changes in their bedtime routine and environment first, and if that doesn’t help, or their insomnia becomes chronic, they should work with their medical provider to find the best treatment option” (American Academy of Sleep Medicine, 2021).
When to see a healthcare provider
If self-help sleep strategies don’t solve your sleep problem, it may be time to visit a family doctor or sleep specialist.
Several different tests can help diagnose sleep disorders, and there are sleep labs around the country that aim to match patient needs with research efforts. For some conditions, like sleep apnea, surgery or continuous positive airway pressure (CPAP) therapy may be recommended (American Academy of Sleep Medicine, n.d.).
Remedies that a healthcare professional might suggest include medications, but also therapies typically directed by a trained therapist but which aim to give people tools to continue self-introspection and problem solving on their own:
Cognitive-behavioral therapy (CBT)
CBT teaches you to recognize and develop a clear view of your own thoughts, attitudes, and expectations, then form strategies to change your behaviors (National Center for Biotechnology Information, 2016).
The European Sleep Research Society and the American Academy of Sleep Medicine consider cognitive-behavioral therapy a front-line nonpharmacological treatment for insomnia. The benefits are well-established by decades of research (Anderson, 2018).
Sleep hypnosis
Hypnosis is done while a person is awake but taken into a state of consciousness involving focused attention and a corresponding openness to suggestion.
A review of the limited available research on hypnosis for sleep problems found some benefits but notes that some studies show no benefit. The technique comes with few adverse effects, the researchers noted (Chamine, 2018).
Mindfulness-based therapy
Mindfulness and mindfulness meditation therapies involve relaxation techniques that teach how to be present, calm the mind, and create better self-awareness of the self––all to reduce stress or anxiety or solve other mental-health challenges.
Preliminary research has indicated it may help people who have trouble sleeping (Behan, 2020). A review of existing research concluded that mindfulness meditation may effectively treat some aspects of sleep disturbance, but more research is needed (Rusch, 2019).
If you have trouble sleeping, the critical first step toward relief is recognizing that you have a common problem with a range of proven possible solutions, many of which include choices about nixing unhelpful habits and adopting good sleep hygiene practices.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Anderson KN. (2018). Insomnia and cognitive behavioural therapy-how to assess your patient and why it should be a standard part of care. Journal of Thoracic Disease; 10 (Suppl 1):S94-S102. doi: 10.21037/jtd.2018.01.35. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803038/
American Academy of Sleep Medicine (2021) Missing the mark with melatonin: Finding the best treatment for insomnia. Retrieved from https://aasm.org/missing-the-mark-melatonin-finding-best-treatment-insomnia/
American Academy of Sleep Medicine (n.d.) Sleep education: Patients. Retrieved from https://sleepeducation.org/patients/
Behan C. (2020). The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Irish Journal of Psychological Medicine; 37 (4):256-258. doi: 10.1017/ipm.2020.38. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7287297/
Chamine I, Atchley R, Oken BS. (2018). Hypnosis intervention effects on sleep outcomes: A systematic review. Journal of Clinical Sleep Medicine; 14 (2):271-283. doi: 10.5664/jcsm.6952. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786848/
Colton HR, Altevogt BM. (2006). Sleep disorders and sleep deprivation: An unmet public health problem. Washington (DC): National Academies Press (US); 2006. 3, Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK19961/
Culpepper L, Wingertzahn MA. (2015). Over-the-counter agents for the treatment of occasional disturbed sleep or transient insomnia: A systematic review of efficacy and safety. Primary Care Companion CNS Disorders; 17 (6):10.4088/PCC.15r01798. doi: 10.4088/PCC.15r01798. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4805417/
Dolezal BA, Neufeld EV, Boland DM, Martin JL, Cooper CB. (2017). Interrelationship between sleep and exercise: A systematic review. Advanced Preventative Medicine; 2017:
doi: 10.1155/2017/1364387. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5385214/
Erland LA, Saxena PK. (2017). Melatonin natural health products and supplements: Presence of serotonin and significant variability of melatonin content. Journal of Clinical Sleep Medicine; 13 (2):275-281. doi: 10.5664/jcsm.6462. Retrieved from h ttps://jcsm.aasm.org/doi/10.5664/jcsm.6462
Figueiro MG, Steverson B, Heerwagen J, Kampschroer K, Hunter CM, Gonzales K, et al. (2017). The impact of daytime light exposures on sleep and mood in office workers. Sleep Health; 3 (3):204-215. doi: 10.1016/j.sleh.2017.03.005. Retrieved from https://www.sleephealthjournal.org/article/S2352-7218(17)30041-4/fulltext
Frank S, Gonzalez K, Lee-Ang L, Young MC, Tamez M, Mattei J. (2017). Diet and sleep physiology: Public health and clinical implications. Frontiers in Neurology; 8:
doi: 10.3389/fneur.2017.00393. Retrieved from https://www.frontiersin.org/articles/10.3389/fneur.2017.00393/full
Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. (2019). Before-bedtime passive body heating by warm shower or bath to improve sleep: A systematic review and meta-analysis. Sleep Medicine Review; 46: 124-135. doi: 10.1016/j.smrv.2019.04.008. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31102877/
Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J., & Hall, M. H. (2015). The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews, 22, 23–36. doi: 10.1016/j.smrv.2014.10.001. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4400203/
Jehan S, Zizi F, Pandi-Perumal SR, et al. (2017). Shift work and sleep: Medical implications and management. Sleep Medicine Disorders; 1 (2):00008. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5836745/
Killgore WDS, Vanuk JR, Shane BR, Weber M, Bajaj S. (2020). A randomized, double-blind, placebo-controlled trial of blue wavelength light exposure on sleep and recovery of brain structure, function, and cognition following mild traumatic brain injury. Neurobiological Diseases; 134:
doi: 10.1016/j.nbd.2019.104679. Retrieved from https://www.sciencedirect.com/science/article/pii/S0969996119303547
National Center for Biotechnology Information. (2016). Cognitive-behavioral therapy. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279297/
National Center for Complementary and Integrative Health. (2021). Melatonin: What you need to know. Retrieved from https://www.nccih.nih.gov/health/melatonin-what-you-need-to-know
Perini F, Wong KF, Lin J, Hassirim Z, Ong JL, Lo J, et al. (2021). Mindfulness-based therapy for insomnia for older adults with sleep difficulties: a randomized clinical trial. Psychological Medicine, 1-11. doi: 10.1017/S0033291721002476. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34193328/
Rasch B, Born J. (2013). About sleep's role in memory. Physiological Reviews; 93 (2):681-766. doi: 10.1152/physrev.00032.2012. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3768102/
Reichner CA. (2015). Insomnia and sleep deficiency in pregnancy. Obstetric Medicine; 8 (4):168-171. doi: 10.1177/1753495X15600572. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4935047/
Rusch HL, Rosario M, Levison LM, et al. (2019). The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences; 1445 (1):5-16. doi: 10.1111/nyas.13996. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6557693/
Shokri-Kojori E, Wang GJ, Wiers CE, Demiral SB, Guo M, Kim SW, et al. (2018). β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proceedings of the National Academy of Sciences of the United States of America; 115 (17):4483-4488. doi: 10.1073/pnas.1721694115. Retrieved from https://www.pnas.org/content/115/17/4483.full
UpToDate. (2021). Approach to the patient with excessive daytime sleepiness. Retrieved from https://www.uptodate.com/contents/approach-to-the-patient-with-excessive-daytime-sleepiness
UpToDate. (2021). Classification of sleep disorders. Retrieved from https://www.uptodate.com/contents/classification-of-sleep-disorders
UpToDate. (2021). Overview of the treatment of insomnia in adults. Retrieved from https://www.uptodate.com/contents/classification-of-sleep-disorders
U.S. Department of Health and Human Services-a. (n.d.). Healthy People 2030. Retrieved from https://health.gov/healthypeople
U.S. Department of Health and Human Services-b. (n.d.). Healthy People 2030. Retrieved from https://health.gov/healthypeople/objectives-and-data/browse-objectives/children/increase-proportion-children-who-get-sufficient-sleep-emc-03
U.S. Department of Health and Human Services-c. (n.d.). Healthy People 2030. Retrieved from https://health.gov/healthypeople/objectives-and-data/browse-objectives/sleep/increase-proportion-high-school-students-who-get-enough-sleep-sh-04
U.S. Department of Health and Human Services-d. (n.d.). Healthy People 2030. Retrieved from https://health.gov/healthypeople/objectives-and-data/browse-objectives/sleep/increase-proportion-adults-who-get-enough-sleep-sh-03/data
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep; 38 (6):843-4. doi: 10.5665/sleep.4716. Retrieved from https://aasm.org/resources/pdf/pressroom/adult-sleep-duration-consensus.pdf
Winkelman J, Benca R. (2021). Overview of the treatment of insomnia in adults. In: UpToDate. Retrieved from https://www.uptodate.com/contents/overview-of-the-treatment-of-insomnia-in-adults
Xie Z, Chen F, Li WA, Geng X, Li C, Meng X, et al. (2017). A review of sleep disorders and melatonin. Neurological Research; 39 (6):559-565. doi: 10.1080/01616412.2017.1315864. Retrieved from https://www.tandfonline.com/doi/full/10.1080/01616412.2017.1315864
Zaheed A, Spira A, Chervin R, Zahodne L. (2021). 537 insomnia symptoms and subsequent cognitive performance in older adults: Are depressive symptoms and vascular disease mediators?, Sleep, 44 (Supplement_2): A212. doi10.1093/sleep/zsab072.535. Retrieved from https://academic.oup.com/sleep/article-abstract/44/Supplement_2/A212/6260400