Key takeaways
Ozempic is an FDA-approved GLP-1 receptor agonist medication used to treat type 2 diabetes. It’s also used off-label for weight loss.
Ozempic mimics a natural hormone in your body and works by improving blood sugar control and reducing hunger.
Although side effects can occur, Ozempic has a good safety profile. Serious adverse events are rare.
The most common side effects are nausea, vomiting, diarrhea, abdominal pain, and constipation. Your healthcare provider can give you tips to help manage side effects.
Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Key takeaways
Ozempic is an FDA-approved GLP-1 receptor agonist medication used to treat type 2 diabetes. It’s also used off-label for weight loss.
Ozempic mimics a natural hormone in your body and works by improving blood sugar control and reducing hunger.
Although side effects can occur, Ozempic has a good safety profile. Serious adverse events are rare.
The most common side effects are nausea, vomiting, diarrhea, abdominal pain, and constipation. Your healthcare provider can give you tips to help manage side effects.
You’ve probably heard the buzz about Ozempic—the “blockbuster” weight loss drug has dominated headlines and celebrity news for years. But what is Ozempic, how does it work, and is it safe?
If you’re curious about Ozempic but still have questions about how safe and effective it is, talk to a knowledgeable healthcare provider. They can help you understand the benefits, risks, and whether you might be a good candidate for this type of medication.
In the meantime, read on to learn how Ozempic works, how it promotes weight loss, its safety and side effects, considerations for weight management, and more.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
What is Ozempic and how does it work?
Ozempic is an injectable prescription drug that was approved by the Food and Drug Administration (FDA) to treat type 2 diabetes but is sometimes used off-label for weight loss.
The active ingredient in Ozempic is semaglutide.
Ozempic comes in a pre-filled, self-injectable pen that you take once a week, on the same day each week. It comes in four dose strengths: 0.25 mg, 0.5 mg, 1 mg, and 2 mg. Your provider will most likely start you on the lowest dose and then gradually increase that over time, depending on how well you tolerate the medication.
Although it’s intended to help regulate blood sugar and reduce heart-related health risks in people with type 2 diabetes, Ozempic may also promote significant weight loss when combined with certain diet and exercise modifications.
Ozempic is in a class of medications called glucagon-like peptide-1 receptor agonists (GLP-1). GLP-1 medications mimic the GLP-1 incretin hormone that the body produces. Incretin hormones are peptides the intestine releases into the bloodstream when we eat.
GLP-1 has several functions, including:
Helps with glucose (blood sugar) regulation and improves insulin sensitivity
Alters the hunger and fullness signals the brain receives
Slows the rate of food moving from the stomach to the small intestine
Other injectable medications in this class that are indicated to treat type 2 diabetes or obesity include liraglutide (Saxenda)and tirzepatide (Zepbound, Mounjaro). Semaglutide is also available under the brand name Wegovy, which is FDA-approved for people with obesity and people with overweight who have a weight-related health condition, such as high blood pressure or type 2 diabetes. It is also indicated to reduce the risk of heart attack and stroke in adults who have cardiovascular disease and have obesity or overweight.
Saxenda Important Safety Information: Read more about serious warnings and safety info.
Zepbound Important Safety Information: Read more about serious warnings and safety info.
Mounjaro Important Safety Information: Read more about serious warnings and safety info.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
Key takeaways
If you have type 2 diabetes, Ozempic can help you manage your blood sugar, which can also boost overall health and help with weight management.
Ozempic also helps increase feelings of fullness and satisfaction from the foods you eat. This can lead to consuming fewer calories, which can help with weight loss.
How Ozempic works for type 2 diabetes
If you have type 2 diabetes, your body may secrete less GLP-1 hormone. Ozempic acts like GLP-1, producing some of the benefits of this hormone, including better blood sugar control.
When you eat, glucose rises in the bloodstream. Your pancreas handles producing and releasing insulin in response to a glucose rise. Insulin is a hormone that aids in transporting glucose into cells to be used for energy.
People with type 2 diabetes have insulin resistance, meaning that cells no longer respond as well to insulin. Therefore, blood sugar levels continue to be high. Beta cells in the pancreas respond by producing even more insulin, but eventually, they can’t produce enough to keep up with the high glucose levels. As a result, blood sugar continues to increase.
The GLP-1 hormone helps your pancreas produce more insulin. By mimicking this hormone, Ozempic functions in a similar fashion. The increased insulin production can help lower high blood sugar, aiding in the treatment of type 2 diabetes.
A note about Ozempic and FDA-approved indications
The FDA approved Ozempic to treat type 2 diabetes in 2017. Doctors sometimes prescribe the medication off-label for weight management in people with obesity or overweight. “Off-label” use means prescribing a drug for a purpose other than its intended indication.
The FDA also approved semaglutide under the brand name Wegovy for people with obesity and overweight who have at least one weight-related condition, such as high blood pressure, high cholesterol, or Type 2 diabetes.
How does Ozempic work for weight loss?
People who have obesity or overweight may also experience reduced GLP-1 secretion. The GLP-1 hormone that Ozempic mimics helps to slow gastric emptying (the rate at which food moves out of your stomach and into the lower intestine). Slower gastric emptying can make you feel fuller faster when eating and help you feel satisfied longer.
Ozempic activates the GLP-1 receptors in the brain, resulting in the activation of certain neurons and the inactivation of others. Through these processes, Ozempic helps regulate appetite and quiet “food noise.” Food noise is a collective term to describe having persistent and intrusive thoughts about food, and it may be associated with leptin resistance.
Leptin is a hormone that fat tissue produces. It tells your brain you’re full. However, with obesity and overweight, the brain can become resistant to leptin’s signal.
“We have GLP receptors throughout our body, including in our gastrointestinal system (stomach, liver, and pancreas), as well as in the brain,” says Sarah Stombaugh, MD, a family medicine physician and diplomat of the American Board of Obesity Medicine.
“Stimulating GLP has multiple effects which impact weight, including decreased insulin resistance, slower gastrointestinal transit time, and decreased hunger and cravings.”
By reducing appetite and silencing food noise, Ozempic can help you eat less, feel more satisfied at meals, and focus on optimal nutrition.
Ozempic side effects for weight loss
As with any medication, Ozempic does have some potential side effects. The side effects are generally the same whether you take Ozempic for type 2 diabetes or weight loss.
“While generally well-tolerated, Ozempic can cause mostly gastrointestinal side effects,” adds Resham Uttamchandani, MD, founder of Doctor U who is double-board certified in family medicine and obesity medicine.
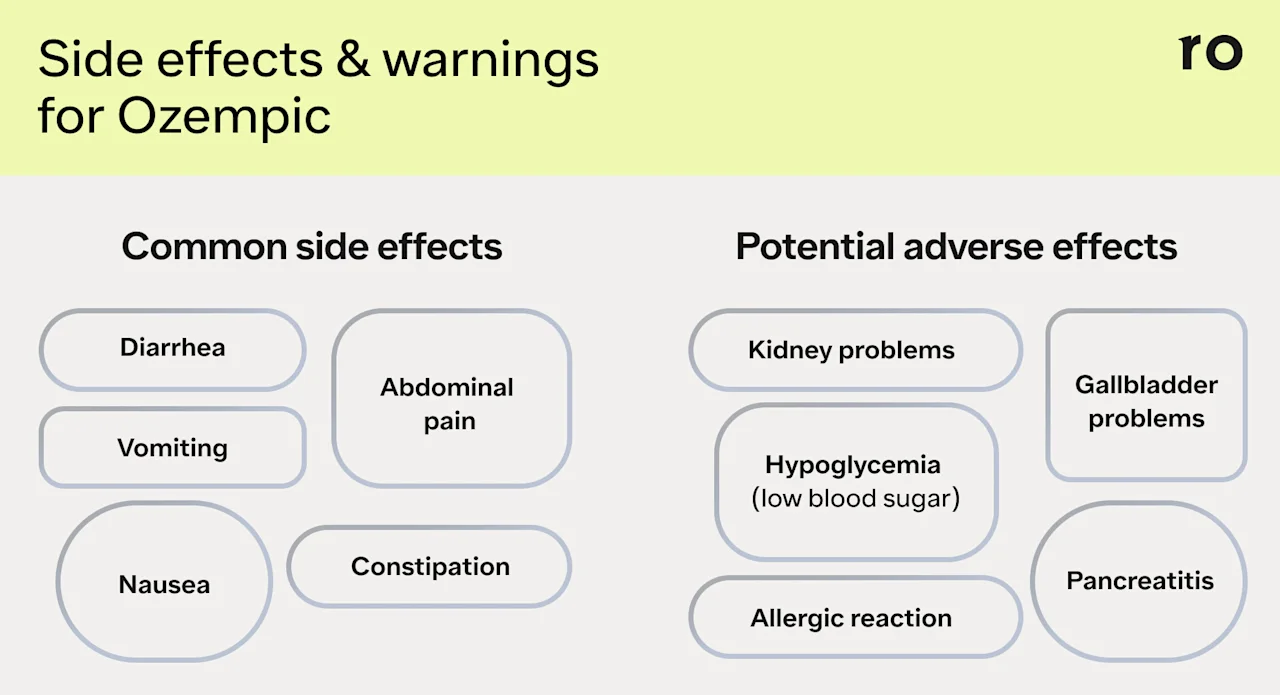
Common side effects
The most common reported side effects include:
Abdominal pain
Constipation
Diarrhea
Nausea
Vomiting
Tips for managing common side effects of Ozempic
Common GI side effects tend to be mild and go away as your body adjusts to the medication. But that doesn’t mean you have to power through discomfort while taking Ozempic. Talk to your provider about ways to manage and minimize common side effects.
The following strategies may help you manage or reduce common side effects:
Start at the lowest dose and slowly increase it over time. Research shows that side effects tend to be most intense when a person first starts Ozempic or when they move up to the next dose strength.
Don’t skip doses. Starting at higher doses or jumping dose strengths increases your risk for more severe side effects.
Drink plenty of water. Some common side effects can lead to dehydration, so make sure you’re taking in enough fluids each day.
Eat smaller, more frequent meals. This may help to curb nausea and other GI discomfort as your body adjusts.
Ask your doctor about anti-nausea meds. Your provider may recommend a prescription or over-the-counter medication to help with nausea and vomiting.
Warnings and precautions for Ozempic
Adverse events may also occur with Ozempic, though these are rare.
“Semaglutide is a safe medication when used under the supervision of a provider who is experienced with GLP medications,” Dr. Stombaugh says. “While mild side effects, such as nausea and constipation, are common from this medication, serious side effects, like bowel obstruction or gastroparesis, are rare and may be avoidable with close monitoring.”
Stop using Ozempic and talk to your doctor right away if you experience any of the following:
Allergic reactions. Symptoms may include facial or throat swelling, difficulty breathing or swallowing, itching or rash, fainting or feeling dizzy, or rapid heartbeat.
Inflammation of your pancreas (pancreatitis). Symptoms may include severe abdominal pain that doesn’t go away and sometimes back pain.
Gallbladder problems. Symptoms may include pain in your upper abdomen, fever, yellowing of the skin or eyes, or clay-colored stools.
Kidney problems (kidney failure). People with existing kidney problems may experience a worsening of their symptoms if they experience dehydration. Kidney injury may also occur in those without kidney disease, according to some reports. Kidney injury may require hemodialysis.
Low blood sugar (hypoglycemia). Symptoms may include dizziness or lightheadedness, blurred vision, mood changes, sweating, slurred speech, hunger, confusion, drowsiness, shakiness, weakness, headache, rapid heartbeat, or feeling jittery.
Vision changes. Symptoms may include blurred vision, floaters, or spots. For people with type 2 diabetes who also have a history of diabetic retinopathy (a condition that can cause blood vessel damage in the retina), Ozempic may worsen symptoms. People with a known history of diabetic retinopathy should be closely monitored while taking this medication.
Gastroparesis or bowel obstruction. Some research has found that semaglutide is associated with gastroparesis (stomach paralysis) and bowel obstruction.
“There is a boxed warning for the potential risk of thyroid C-cell tumors, including medullary thyroid carcinoma and this needs to be screened for before initiating any medications,” Dr. Uttamchandani says.
Tell your doctor if you experience a lump or swelling in your neck, trouble swallowing, shortness of breath, or hoarseness, as these may be signs of a thyroid tumor.
People who have a personal or family history of thyroid tumors may not be good candidates for Ozempic or other GLP-1 medications.
Drug interactions for Ozempic
Ozempic may interact with other medications, so it’s important to tell your doctor about all the prescription or over-the-counter medications, supplements, and herbs you’re taking.
Here are some considerations and potential drug interactions for Ozempic:
Oral medications. If you take any medications by mouth, such as oral birth control (the pill), Ozempic may affect how well you absorb them. This is because Ozempic can delay gastric emptying. In clinical trials, however, Ozempic did not have a major impact on oral medication absorption.
Blood-sugar lowering medications. If you take other medications to control your blood sugar, you may have a higher risk of experiencing low blood sugar while taking Ozempic, which can be dangerous.
Insulin and sulfonylureas. You may also be at a higher risk of experiencing low blood sugar while taking Ozempic if you take insulin or a sulfonylurea (a class of medications that stimulates insulin secretion).
Blood pressure medications. Medications that lower your blood pressure can make it more difficult to notice if your blood sugar is low.
GLP-1s. Ozempic should not be taken with other GLP-1 medications, as this could lead to more severe side effects.
Diuretics. Loop and thiazide diuretics help remove excess fluid from the body. These medications, which are used to treat heart conditions, may decrease the beneficial effects of Ozempic.
Who should not use Ozempic?
Some people should avoid Ozempic. Do not use Ozempic if you’re under 18, or if you’re allergic to any ingredients in the medication.
Do not use Ozempic if you are pregnant, breastfeeding, or about to become pregnant. You should stop using Ozempic at least two months before conceiving.
You should not take Ozempic if you or a family member have ever had medullary thyroid carcinoma (a type of thyroid cancer) or multiple endocrine neoplasia type 2 (a condition that affects the endocrine system).
If you have a personal or family history of kidney problems, pancreatitis, or diabetic retinopathy, talk to your doctor about these issues. Ozempic may not be suitable for you.
Is Ozempic effective for weight loss?
While Ozempic is indicated for type 2 diabetes, research on semaglutide has shown that it can lead to significant weight loss.
“Medications like Ozempic can be a helpful tool when used as part of a comprehensive approach that includes lifestyle modifications,” Dr. Uttamchandani says. “The most effective strategy is personalized and may evolve over time.”
Semaglutide weight loss results
It’s important to note that most (but not all) clinical trials reporting weight loss outcomes studied participants taking 2.4 mg of semaglutide, which is the maximum dose for Wegovy (Ozempic’s maximum dose strength is 2 mg).
Weight loss results will be different for each person who uses semaglutide, whether they are taking Wegovy or have been prescribed Ozempic off-label. Still, we can also look at results from Wegovy clinical trials for weight loss to get a sense of how effective this drug might be for weight management.
In one Phase 3 clinical trial (called SUSTAIN 1), people with type 2 diabetes, who hadn’t previously received treatment aside from lifestyle changes, received either 0.5 mg or 1.0 mg of semaglutide or a dose-matched placebo as a once-weekly injection for 30 weeks (about 7.5 months). Participants taking 0.5 mg of semaglutide lost, on average, about 8 pounds, and those taking 1.0 mg lost an average of 10 pounds at the end of the study.
In another Phase 3 clinical trial, participants with obesity or overweight who combined a once-weekly injection of 2.4 mg of semaglutide with a reduced-calorie diet and regular exercise lost an average of 15% of their weight over the study, which lasted 68 weeks (or 1.3 years).
In long-term results, research shows that 2.4 mg of semaglutide is associated with, on average, a 10% reduction in weight at 208 weeks (about four years).
It’s important to note that this level of weight loss isn’t the result of medication alone. In the trials for 2.4 mig of semaglutide, the treatment group combined medication with a reduced-calorie diet (consuming about 500 fewer calories per day) and 150 minutes of exercise per week.
Ozempic and other injectable GLP-1 medications are designed to be used in combination with diet and exercise to see more significant and sustainable results.
“If someone has struggled with health consequences of their weight and has found diet and exercise alone have not been enough to support their weight goals, medications like semaglutide may be a good option to support their health and weight goals,” Dr. Stombaugh says.
Long-term use and rebound weight gain
To see sustained weight loss results, you have to take Ozempic for a long time— typically for a year or longer. Your healthcare provider can offer guidance on how long you’ll need to take Ozempic, factoring in things like your weight loss goals, your overall health, and how well you tolerate any side effects.
Research shows that stopping semaglutide too soon may lead to regaining the weight you lost while taking the medication.
Studies haven’t looked at rebound weight gain for the maximum dose of Ozempic. However,in one randomized controlled trial of 2.4 mg of semaglutide (the maximum Wegovy dose), participants regained about two-thirds of the weight they lost after discontinuing semaglutide and stopping lifestyle changes for a full year. This rebound weight gain occurred after participants had been on the medication for 1.3 years and made lifestyle changes, including diet and exercise, during that time.
If you are interested in taking Ozempic for weight loss, you will need to be on it long-term to sustain the weight management benefits of the medication.
Lifestyle changes and Ozempic
Taken as a whole, research results for semaglutide illustrate the need for making certain lifestyle changes while taking Ozempic—and maintaining them even after stopping the medication.
“Patients who combine GLP medications like semaglutide with intensive lifestyle modification including nutrition, movement, sleep, and stress management have better long-term weight loss compared to patients who use GLP medications or lifestyle modification alone,” Dr. Stombaugh says.
When considering changes to physical activity, weight training may be especially important if you use Ozempic. Research shows that some weight loss from the medication involves muscle loss rather than fat loss. Muscle loss over time can have negative effects on overall health. But you can maintain muscle mass through resistance exercise and other strategies.
The bottom line: Consult with a knowledgeable healthcare provider before using Ozempic. They can help you decide if the medication is right for you and can provide useful tips and guidance for sustainable approaches to weight loss and blood sugar control.
Ozempic vs. Wegovy and other injectable GLP-1s
Ozempic and Wegovy are two brand names for the injectable medication semaglutide. While both medications are FDA-approved, they have different indications and come in different doses.
Other injectable medications in this class that are indicated to treat type 2 diabetes or obesity include liraglutide (Saxenda)and tirzepatide (Zepbound, Mounjaro).
Here’s a quick breakdown of each medication, its indications, some common side effects, dosages, and costs.
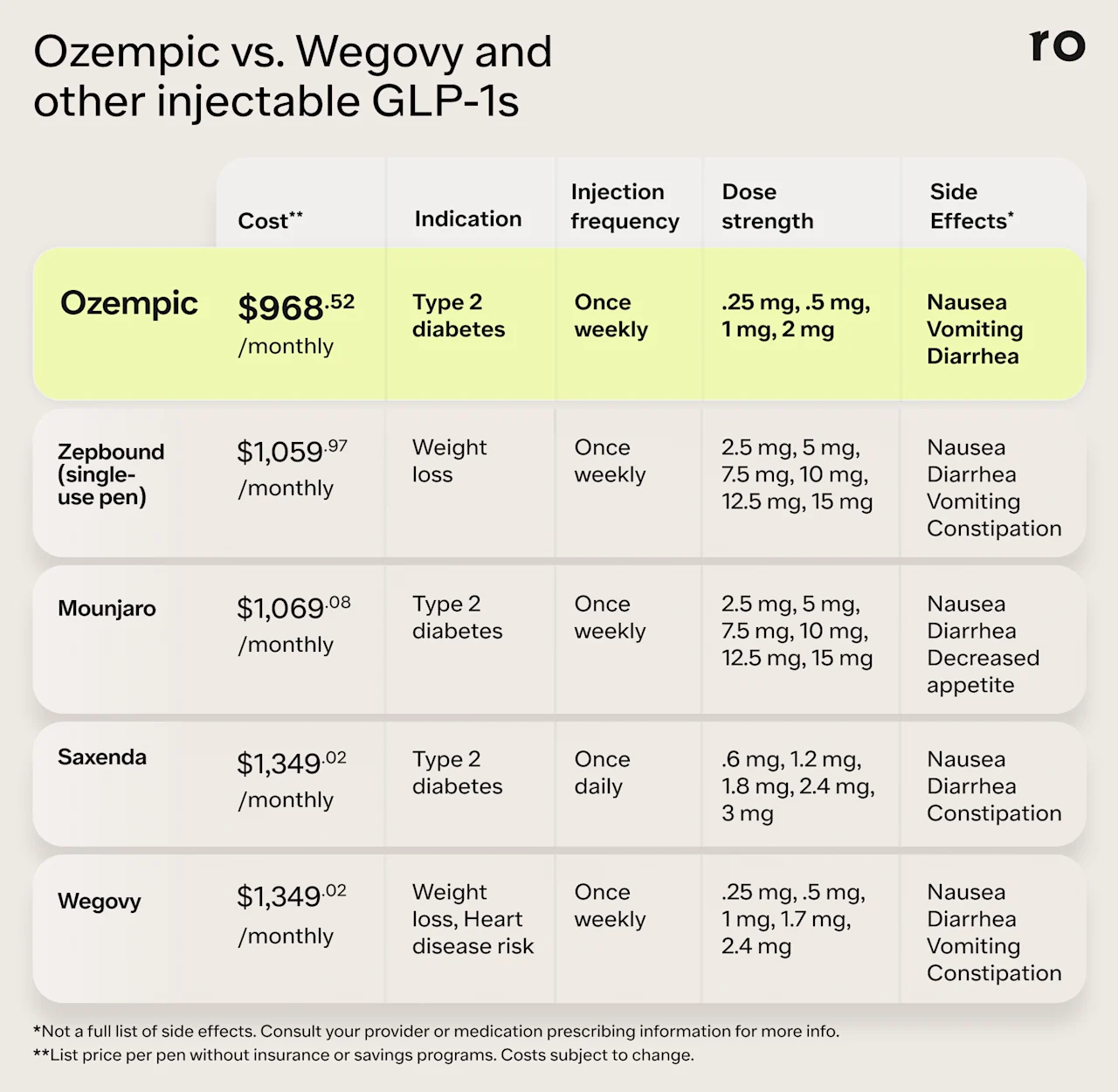
This table can give you a high-level look at these medications but is not an exhaustive list of all medication information side effects, or warnings. Always talk to an experienced and knowledgeable healthcare provider before trying a new medication.
Your provider can help you figure out if you’re a good candidate, and give more information on the potential benefits and risks. They’ll consider your health goals, personal and family health history, current health status, any medications or supplements you’re taking, and other health-related factors to determine if GLP-1 medications are a safe and appropriate option for you.
Bottom line
Ozempic is a GLP-1 medication used to treat type 2 diabetes and may be used off-label for weight loss. It works by helping with blood sugar management and reducing hunger.
Ozempic has been studied for safety and efficacy and is generally considered safe.
Common GI side effects like nausea, diarrhea, and abdominal pain tend to be mild and manageable. More serious adverse effects are rare.
Working with a knowledgeable healthcare provider can help manage mild side effects and minimize your risk for any health complications.
Some people should not take Ozempic due to a higher risk of adverse effects or drug interactions. Always talk to a knowledgeable healthcare provider before taking a new medication.
Frequently asked questions (FAQ)
Is Ozempic safe for weight loss?
Yes. Ozempic is FDA-approved, which means that it has gone through rigorous clinical trials to determine its safety and effectiveness. As with any medication, Ozempic may cause side effects, though these are generally mild and manageable and include GI issues like nausea, diarrhea, and constipation.
That said, Ozempic may not be the best option for everyone. People with a personal or family history of thyroid tumors, pancreatitis, or kidney problems may be at higher risk for health complications with Ozempic. Working with an experienced clinician can help you determine if Ozempic is safe for you.
Are there long-term safety risks with Ozempic?
Ozempic and other injectable GLP-1 medications are meant to be taken long term to sustain weight loss and blood sugar control, and have a good safety profile.
Clinical trials typically followed participants taking semaglutide over one to two years and did not show a significant increase in either common side effects or adverse events over that time. That said, some people—including those with a personal or family history of thyroid tumors, pancreatitis, or kidney problems—may not be good candidates for Ozempic and may be at higher risk for serious health complications.
More research is needed on the impacts of long-term use (beyond two years) of Ozempic to fully understand the potential risks and benefits. In the meantime, your provider can help determine how long you’ll need to take Ozempic to see and maintain its health benefits.
What are the benefits of taking Ozempic?
Ozempic has benefits for blood sugar management, which can help with type 2 diabetes and aid weight loss. Ozempic also helps regulate appetite, which can help you lose weight.
What are the cons of taking Ozempic?
As with any medication, Ozempic may cause side effects. While the most common side effects are generally mild and manageable, they can be unpleasant.
Ozempic may lead to weight loss, but some of the weight you lose may be muscle mass, which can impact your overall health.
Ozempic is a long-term medication, and most people need to take Ozempic for more than a year to maintain weight loss results.
Lastly, Ozempic can be expensive, costing nearly $1,000 per month. Insurance and savings programs can help reduce the cost of Ozempic, but keep in mind that some insurance plans will not cover medications that are used off-label.
What about “Ozempic face?”
“Ozempic face” is a term coined on social media that describes possible changes to a person’s appearance after using a weight loss drug. That might include a loss of volume in the face, a “sunken” look in the cheeks, sagging skin, and signs of premature aging.
While there are anecdotal reports of people’s facial appearance changing after using weight loss medication, it’s unclear if these changes are due to the medications themselves or simply an outcome of significant weight loss. More research is needed to understand if or how medications like semaglutide might impact facial volume.
As always, discuss any questions or concerns you might have about Ozempic with your provider.
What happens if you take Ozempic without diabetes?
Ozempic helps people with type 2 diabetes have better blood sugar control. Having better blood sugar control also benefits people with prediabetes or other conditions like insulin resistance or polycystic ovarian syndrome (PCOS). Better blood sugar control can also help with weight management.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Baggio, L. L. & Drucker, D. J. (2014). Glucagon-like peptide-1 receptors in the brain: controlling food intake and body weight. The Journal of Clinical Investigation, 124(10), 4223. doi: 10.1172/JCI78371. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4191040/
Calanna, S., Christensen, M., Holst, J. J., et al. (2013). Secretion of glucagon-like peptide-1 in patients with type 2 diabetes mellitus: systematic review and meta-analyses of clinical studies. Diabetologia, 56(5), 965. doi: 10.1007/s00125-013-2841-0. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3687347
Hayashi, D., Edwards, C., Emond, J. A., et al. (2023). What is food noise? A conceptual model of food cue reactivity. Nutrients, 15(22), 4809. doi: 10.3390/nu15224809. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10674813/
Ida, S., Kaneko, R., Imataka, K., et al. (2021). Effects of antidiabetic drugs on muscle mass in type 2 diabetes mellitus. Current Diabetes Reviews, 17(3), 293-303. doi: 10.2174/1573399816666200705210006. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32628589/
Jensterle, M., Ferjan, S., Ležaič, L., et al. (2023). Semaglutide delays 4-hour gastric emptying in women with polycystic ovary syndrome and obesity. Diabetes, Obesity, and Metabolism, 25(4), 975-984. doi: 10.1111/dom.14944. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36511825/
Knudsen, L. B. & Lau, J. (2019). The discovery and development of liraglutide and semaglutide. Frontiers in Endocrinology (Lausanne), 10, 155. doi: 10.3389/fendo.2019.00155. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31031702/
Kommu, S. & Whitfield, P. (2024). Semaglutide. StatPearls. Retrieved Nov. 12, 2024 from https://www.ncbi.nlm.nih.gov/books/NBK603723/
Liu, J., Yang, X., Yu, S., & Zheng, R. (2018). The leptin resistance. Advances in Experimental Medicine and Biology, 1090, 145-163. doi: 10.1007/978-981-13-1286-1_8. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30390289/
Montecinos, K., Kania, B., & Goldberg, D. J. (2024). Semaglutide “Ozempic” Face and Implications in Cosmetic Dermatology. Dermatological Reviews, 5(5), e70003. https://doi.org/10.1002/der2.70003. Retrieved from https://onlinelibrary.wiley.com/doi/epdf/10.1002/der2.70003
Müller, T. D., Finan, B., Bloom, S. R., et al. (2019). Glucagon-like peptide 1 (GLP-1). Molecular Metabolism, 30, 72-130. doi: 10.1016/j.molmet.2019.09.010. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31767182/
Novo Nordisk. (2017). Ozempic® (semaglutide) approved in the US. Retrieved from https://www.novonordisk.com/content/nncorp/global/en/news-and-media/news-and-ir-materials/news-details.html?id=712
Popoviciu, M. S., Păduraru, L., Yahya, G., et al. (2023). Emerging role of glp-1 agonists in obesity: a comprehensive review of randomised controlled trials. International Journal of Molecular Sciences, 24(13), 10449. doi: 10.3390/ijms241310449. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10341852/
Ryan, D. H., Lingvay, I., Deanfield, J., et al. (2024). Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial. Nature Medicine, 30(7), 2049-2057. doi: 10.1038/s41591-024-02996-7. Retrieved from https://www.nature.com/articles/s41591-024-02996-7
Sodhi, M., Rezaeianzadeh, R., Kezouh, A., et al. (2023). Risk of gastrointestinal adverse events associated with glucagon-like peptide-1 receptor agonists for weight loss. JAMA, 330(18), 1795. doi: 10.1001/jama.2023.19574. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10557026/
U.S. Food and Drug Administration (FDA). (2018). Understanding unapproved use of approved drugs “off label”. Retrieved from https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label
Wadden, T. A., Chao, A. M., Moore, M., et al. (2023). The role of lifestyle modification with second-generation anti-obesity medications: comparisons, questions, and clinical opportunities. Current Obesity Reports, 12(4), 453. doi: 10.1007/s13679-023-00534-z. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10748770/
Wilding, J. P. H, Batterham, R. L., Calanna, S., et al. (2021). Once-weekly semaglutide in adults with overweight or obesity. New England Journal of Medicine, 384(11), 989-1002. doi: 10.1056/NEJMoa2032183. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa2032183