Key takeaways
Semaglutide (Wegovy, Ozempic, Rybelsus) can cause constipation.
You can get relief from semaglutide constipation by drinking enough water, eating more fiber, exercising, and taking OTC laxatives or stool softeners.
Speak with your healthcare provider if you have vomiting, severe abdominal pain or swelling, or if you can’t pass gas.
Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Key takeaways
Semaglutide (Wegovy, Ozempic, Rybelsus) can cause constipation.
You can get relief from semaglutide constipation by drinking enough water, eating more fiber, exercising, and taking OTC laxatives or stool softeners.
Speak with your healthcare provider if you have vomiting, severe abdominal pain or swelling, or if you can’t pass gas.
If you’re here, you’re likely dealing with semaglutide constipation. It’s a common side effect, but there are ways to find relief, even while continuing to take the medication.
6 ways to get rid of semaglutide constipation
Gastrointestinal (GI) problems are no picnic. But they’re often an unfortunate reality for many people taking semaglutide, the active ingredient in Wegovy, Ozempic, and Rybelsus. In clinical trials:
Nearly 24% of people on Wegovy experienced constipation
3%–5% of people on Ozempic experienced constipation
5%–6% of people on Rybelsus experienced constipation
Here are some tips to ease discomfort associated with constipation and get things, ahem, flowing smoothly while your body gets used to the medication.
1. Stay hydrated
Make sure you’re drinking water and other hydrating fluids to prevent your stools from getting too hard. Hard stools are more difficult and painful to pass than soft stools.
Here are some tips to help you hydrate:
If nausea is preventing you from staying hydrated, try having small sips of ice-cold water more often.
Add a squeeze of lemon or lime to make plain water less boring.
Eat foods with a high water content, like watermelon, cucumber, soup, or even popsicles made from pureed fruits and vegetables.
If semaglutide side effects like nausea and vomiting make it too hard to stay hydrated, contact your healthcare provider or seek emergency medical attention if you’re experiencing symptoms of severe dehydration, as you may need IV fluids.
2. Focus on fiber
Aim to get about 25–30 g of fiber a day. Examples of fiber-rich foods include:
Beans
Lentils
Broccoli
Sweet potatoes
High-fiber breakfast cereals like shredded wheat and bran flakes
Not getting enough dietary fiber can cause hard, lumpy stool and constipation. Be sure to pair fiber with adequate water intake, as water helps fiber pass more smoothly through the digestive system. Sip water or other non-sugary drinks shortly before or after getting your daily fill of fiber.
3. Get enough sleep
What does sleep have to do with pooping regularly? Turns out, a lot. Not getting enough quality sleep can increase the risk of constipation, according to a 2024 review.
The smooth muscle movements in the colon align with your body’s circadian rhythm. Movement in the colon gets less active at night (which is why you generally don’t need to poop overnight) and increases during the day. If you’re not sleeping well, your circadian rhythm can get thrown off, and this can lead to digestive problems like constipation.
You can improve your sleep by focusing on healthy sleep hygiene habits.
4. Don’t forget to exercise
Exercise is often a natural remedy for constipation. Although the exact reason isn’t totally understood, it might be because working out can help the smooth muscles in the colon move more, which can help lead to a bowel movement.
Aerobic exercises (e.g., swimming, walking, cycling), appear most effective for helping move stool through the colon.
5. Consider over-the-counter treatments
Over-the-counter (OTC) laxatives or stool softeners can help with semaglutide constipation. However, it’s important to avoid regular or long-term use without guidance, as some laxatives can lead to dependence and worsen constipation over time. Talk with your healthcare provider if you have questions about which option might be best for you or if constipation persists.
There are many types of laxatives, ranging from those that:
Help soften hard stools by drawing water in
Lubricate the stools and intestinal lining for easier passage
Stimulate intestinal muscle contractions to push stool through the digestive tract
Stimulant laxatives in particular should be used sparingly and for short-term relief only, unless directed by a healthcare professional.
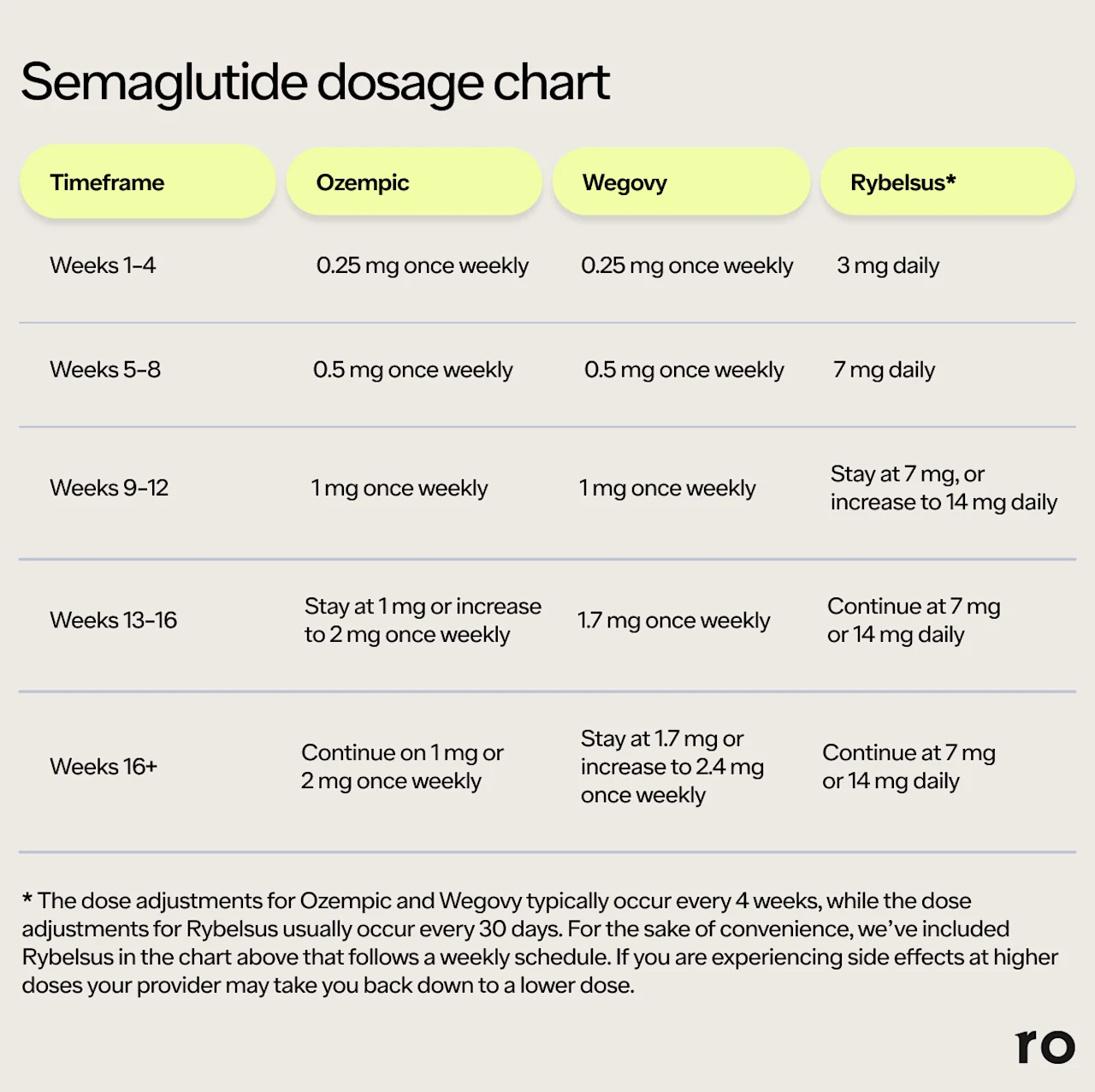
6. Talk to your healthcare provider about dosage
Constipation (and other side effects of semaglutide) can happen more frequently at higher doses. Speak with your healthcare provider if you’re dealing with constipation that’s unbearable or interfering with daily life, as you might need a medication adjustment.
If adjusting your semaglutide dose doesn’t relieve your symptoms, your healthcare provider might end up having you stop semaglutide and switch to a different medication with a lower likelihood of intolerable GI side effects.
How long does semaglutide constipation last?
Semaglutide constipation generally lasts around 47 days on average before improving. Although it’s usually temporary, how long it lasts is different for everyone. Here’s what you should know:
Side effects of semaglutide tend to get better and even disappear as your body gets used to the medication.
But while it usually improves, constipation can still come and go while you’re on semaglutide. You might experience more constipation when you first start the medication and right after dose increases.
People on the highest doses of Wegovy (2.4 mg, injected weekly), Ozempic (2 mg, injected weekly), and Rybelsus (14 mg, taken orally daily) tend to experience semaglutide constipation more often than those on lower doses.
Remember: Semaglutide dosing follows a titration schedule. This is where your healthcare provider gradually increases the dose until the desired effect is achieved without too many side effects. Side effects tend to happen right after a dose adjustment, so give your body a chance to adjust to the medication to see if your side effects improve.
Why does semaglutide cause constipation?
Researchers don’t know precisely why semaglutide and constipation can often go hand-in-hand, but they theorize it’s related to how the medication works on your digestive system:
It slows your digestion: Semaglutide is a glucagon-like peptide-1 receptor (GLP-1) agonist that delays gastric emptying — the movement of food from your stomach into your intestines. Slowing down your digestive system can result in more constipation.
You’re dehydrated: Delayed gastric emptying means you feel satisfied with less food, which can lead to reduced eating and drinking. Not getting enough fluids can cause constipation.
You’re nauseated: Nausea is the most common side effect of semaglutide medications. When you feel nauseous, you tend to reach for bland foods like rice and toast — foods that tend to be low in fiber. Less fiber equals less bulk, which makes it harder for stools to pass through the colon.
Semaglutide constipation treatment options: when to contact a healthcare provider
The interventions above work well for many people, but you may need further treatment if you have any of the following symptoms:
Severe stomach pain
Abdominal swelling
Rectal bleeding
Inability to pass gas
Vomiting
These symptoms could indicate a more serious GI issue that requires medical treatment, so seek medical attention if you experience them, or if you have other side effects you’d like to discuss.
Do other weight loss medications cause constipation?
Yes, other weight loss medications can also cause constipation, though orlistat (Xenical) usually causes increased urge to defecate or oily stools instead. The following are medications the United States Food and Drug Administration (FDA) has approved for weight loss. Here’s what to know about the risk of constipation with each:
Tirzepatide (Mounjaro): Constipation happens in about 6%–7% of people taking Mounjaro, depending on the dose, though some studies report an even higher percentage.
Phentermine-topiramate (Qsymia): Constipation happens in 8%–16% of people on Qsymia, depending on the dose.
Naltrexone-bupropion (Contrave): Constipation has been reported in over 19% of people taking Contrave.
Liraglutide (Saxenda): Constipation happens in about 19% of people taking Saxenda.
Orlistat (Xenical): This drug doesn’t appear to cause constipation, but it does cause other GI side effects like oily stools and urgency with bowel movements.
Bottom line
Does semaglutide make you constipated? In some cases, yes. Let’s recap:
Semaglutide may cause mild-to-moderate, temporary constipation. The median length of semaglutide constipation is about 47 days, as the body adjusts to the medication. Individual experiences may vary.
The severity of the GI side effects of semaglutide depends on the dose. Higher doses tend to cause constipation more often than lower doses.
Semaglutide slows down digestion, so you might have fewer bowel movements. Feeling nauseous and not having as much of an appetite can also make you consume less water and fiber, which can contribute to constipation as well.
Lifestyle changes can help with constipation. Staying hydrated, eating more fiber-rich foods, and exercising can help relieve constipation.
Tell your healthcare provider if constipation and other side effects are severe or persistent. Your dosage might need to be adjusted, or your provider might recommend switching to a new treatment. In severe cases, emergency medical treatment might be required.
Frequently asked questions (FAQs)
How do you prevent constipation on semaglutide?
You can decrease your chances of experiencing constipation on semaglutide by staying hydrated, eating fiber-rich foods, and exercising regularly.
Do Ozempic and Wegovy cause constipation?
Yes, Ozempic and Wegovy can cause constipation. Ozempic and Wegovy both contain the active ingredient semaglutide, a GLP-1 that slows down gastric emptying. Constipation is a common side effect of Ozempic and Wegovy, but the good news is this side effect tends to improve over time as the body adjusts to the medication.
Can Ozempic or Wegovy cause a bowel blockage?
Ozempic and Wegovy are GLP-1 drugs that slow gastric emptying, which can increase the rare but serious risk of a bowel blockage. It’s important to tell your healthcare provider if you experience symptoms such as severe abdominal pain, vomiting after eating, a swollen-appearing abdomen, or a complete inability to pass gas or stool.
How do you get rid of GLP-1 constipation?
There are several ways to get rid of GLP-1 constipation, including lifestyle changes like drinking enough water, eating more fiber, getting enough sleep, and exercising. You can also try OTC laxatives or stool softeners, though you should speak with your healthcare provider before using these medications regularly. Sometimes, your semaglutide dose might need to be adjusted, since higher doses can cause more constipation.
Can you take laxatives while on semaglutide?
Yes, you can take laxatives while on semaglutide. It’s always a good idea to run new medications (prescription or OTC) by your healthcare provider. Also, let your provider know if OTC treatments or lifestyle changes aren’t helping with your constipation. You might need a dose adjustment of your semaglutide or a different weight management strategy.
What simple trick empties your bowels immediately?
There really isn’t a simple trick to immediately empty your bowels. But taking OTC laxative stimulants can help you have a bowel movement in a few hours, though you shouldn’t resort to stimulant laxatives on a regular basis. You can also try getting into a better position for pooping, elevating the feet on a foot stool to put your legs into a squatting position. This can help reduce straining.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
GLP-1 Important Safety Information: Read more about serious warnings and safety info.
Mounjaro Important Safety Information: Read more about serious warnings and safety info.
Saxenda Important Safety Information: Read more about serious warnings and safety info.
References
Amato, A., Baldassano, S., Liotta, R., et al. (2014). Exogenous glucagon-like peptide 1 reduces contractions in human colon circular muscle. The Journal of Endocrinology, 221(1), 29–37. doi: 10.1530/JOE-13-0525. Retrieved from https://joe.bioscientifica.com/view/journals/joe/221/1/29.xml
Bashir, A. & Sizar, O. (2024). Laxatives. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537246/
DailyMed. (2025). Ozempic- semaglutide injection, solution. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=adec4fd2-6858-4c99-91d4-531f5f2a2d79
DailyMed-a. (2024). Rybelsus- oral semaglutide tablet. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=27f15fac-7d98-4114-a2ec-92494a91da98
DailyMed-b. (2024). Wegovy- semaglutide injection, solution. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=ee06186f-2aa3-4990-a760-757579d8f77b
Diaz, S., Bittar, K., Hashmi, M. F., & Mendez, M. D. (2023). Constipation. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513291/
Duboc, H., Coffin, B., & Siproudhis, L. (2020). Disruption of circadian rhythms and gut motility: an overview of underlying mechanisms and associated pathologies. Journal of Clinical Gastroenterology, 54(5), 405–414. doi: 10.1097/MCG.0000000000001333. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32134798/
Gao, R., Tao, Y., Zhou, C., et al. (2019). Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scandinavian Journal of Gastroenterology, 54(2), 169–177. doi: 10.1080/00365521.2019.1568544. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30843436/
Gorgojo-Martínez, J. J., Mezquita-Raya, P., Carretero-Gómez, J., et al. (2022). Clinical recommendations to manage gastrointestinal adverse events in patients treated with Glp-1 receptor agonists: a multidisciplinary expert consensus. Journal of Clinical Medicine, 12(1), 145. doi: 10.3390/jcm12010145. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9821052/
Gudin, B., Ladhari, C., Robin, P., et al. (2020). Incretin-based drugs and intestinal obstruction: A pharmacovigilance study. Therapie, 75(6), 641–647. doi: 10.1016/j.therap.2020.02.024. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32418731/
Kommu, S. & Whitfield, P. (2024). Semaglutide. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK603723/
McKeown, N. M. & Slavin, J. (2022). Fibre intake for optimal health: How can healthcare professionals support people to reach dietary recommendations? The BMJ, 378, e054370. doi: 10.1136/bmj-2020-054370. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9298262/
MedlinePlus. (2017). Bowel Obstruction. Retrieved from https://medlineplus.gov/intestinalobstruction.html
MedlinePlus. (2024). Fiber. Retrieved from https://medlineplus.gov/ency/article/002470.htm
Parkman, H. P., Sharkey, E., McCallum, R. W., et al. (2022). Constipation in patients with symptoms of gastroparesis: analysis of symptoms and gastrointestinal transit. Clinical Gastroenterology and Hepatology : The Official Clinical Practice Journal of the American Gastroenterological Association, 20(3), 546–558.e5. doi: 10.1016/j.cgh.2020.10.045. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8079462/
Smits, M. M. & Van Raalte, D. H. (2021). Safety of semaglutide. Frontiers in Endocrinology, 12. doi: 10.3389/fendo.2021.645563. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8294388/
Tantawy, S. A., Kamel, D. M., Abdelbasset, W. K., et al. (2017). Effects of a proposed physical activity and diet control to manage constipation in middle-aged obese women. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 10, 513–519. doi: 10.2147/DMSO.S140250. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5734236/
Taylor, K. & Tripathi, A. K. (2025). Adult dehydration. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK555956/
Tian, M., Song, Y., & Guo, Y., et al. (2024). Association between sleep disorders and constipation risk: a systematic review and meta-analysis. Journal of Clinical Neuroscience, 126, 12-20. doi: 10.1016/j.jocn.2024.05.030. Retrieved from https://www.sciencedirect.com/science/article/pii/S0967586824002182
U.S. Department of Agriculture (USDA). (2019). Food Sources of Dietary Fiber. Retrieved from https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials/food-sources-select-nutrients/food-0
U.S. Food and Drug Administration (FDA-a). (2025). Contrave (naltrexone hydrochloride and bupropion hydrochloride) extended-release tablets, for oral use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/200063s024s026lbl.pdf
U.S. Food and Drug Administration (FDA-b). (2025). Mounjaro (tirzepatide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/215866s034lbl.pdf
U.S. Food and Drug Administration (FDA-c). (2025). Ozempic (semaglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/209637s025lbl.pdf
U.S. Food and Drug Administration (FDA-a). (2024). Qsymia (phentermine and topiramate extended-release capsules), for oral use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/022580s029lbl.pdf
U.S. Food and Drug Administration (FDA-b). (2024). Rybelsus (semaglutide) tablets, for oral use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/213051Orig1s020,213051Orig1s021lbl.pdf
U.S. Food and Drug Administration (FDA-d). (2025). Saxenda (liraglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/206321s022lbl.pdf
U.S. Food and Drug Administration (FDA-c). (2024). Wegovy (semaglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/215256s015lbl.pdf
U.S. Food and Drug Administration (FDA). (2022). Xenical (orlistat) Capsules, for oral use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/020766s038lbl.pdf
Weir, S. B. & Adkhondi, H. (2023). Bland diet. StatPearls. Retrieved on Jul. 1, 2025 from https://www.ncbi.nlm.nih.gov/books/NBK538142/
Wharton, S., Calanna, S., Davies, M., et al. (2021). Gastrointestinal tolerability of once‐weekly semaglutide 2.4 mg in adults with overweight or obesity, and the relationship between gastrointestinal adverse events and weight loss. Diabetes Obesity and Metabolism, 24(1), 94–105. doi: 10.1111/dom.14551. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9293236/














