Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
People are often concerned about their testosterone (T) levels and how it affects their health. Are my levels high enough? Would my sex drive be better if I had higher T levels? Would I finally lose those extra pounds if I had higher T levels? Would I be more assertive at work and finally get that promotion I’ve been gunning for? These are just some of the questions people may ask themselves.
On the flip side, some are concerned that taking testosterone may hurt them because of what they’ve heard or read. Does testosterone cause heart disease? What about high T levels in women? Does high T cause or exacerbate acne? Stay tuned as we demystify testosterone and answer these and other questions for you.
What is testosterone?
We often think of testosterone only as an androgen or “male hormone,” but it’s an important hormone in both men and women. Hormones are chemicals that travel through the blood and act as messengers in the body. Testosterone is a sex hormone, meaning it’s a hormone that affects sexual development and reproduction (Nassar, 2021).
Testosterone is a key male sex hormone with both androgenic and anabolic functions. Androgenic refers to its effects on male sexual characteristics, and anabolic refers to its tissue-building functions. During puberty, T levels increase in males and are responsible for (Nassar, 2021):
An increase in the size of the penis and testicles
Higher muscle mass
A deepening of the voice and facial hair development
Strengthening of bones
Increase in height
Increase in sex drive and aggression
Testosterone levels usually begin to decline slowly at around age 30 and continue to go down over time. Aside from aging, there are many other causes of low testosterone levels.
If you have low testosterone, it’s important to be evaluated by a healthcare provider for the cause instead of jumping straight to treat the low testosterone. If and when a cause is found, treating it directly can sometimes help the testosterone levels normalize.
How is testosterone made?
In males, Leydig cells, special cells in the testicles, are responsible for producing testosterone. This happens through the following steps:
After puberty, the hypothalamus (a part of the brain) releases a hormone called gonadotropin-releasing hormone (GnRH) in pulses.
GnRH stimulates the pituitary gland (also in the brain) to release luteinizing hormone (LH).
LH reaches the testicles through the blood, where it stimulates the Leydig cells to produce testosterone from cholesterol through a process involving several enzymes.
High levels of testosterone signal the hypothalamus and pituitary to stop releasing GnRH and LH, respectively, keeping tight control of the system.
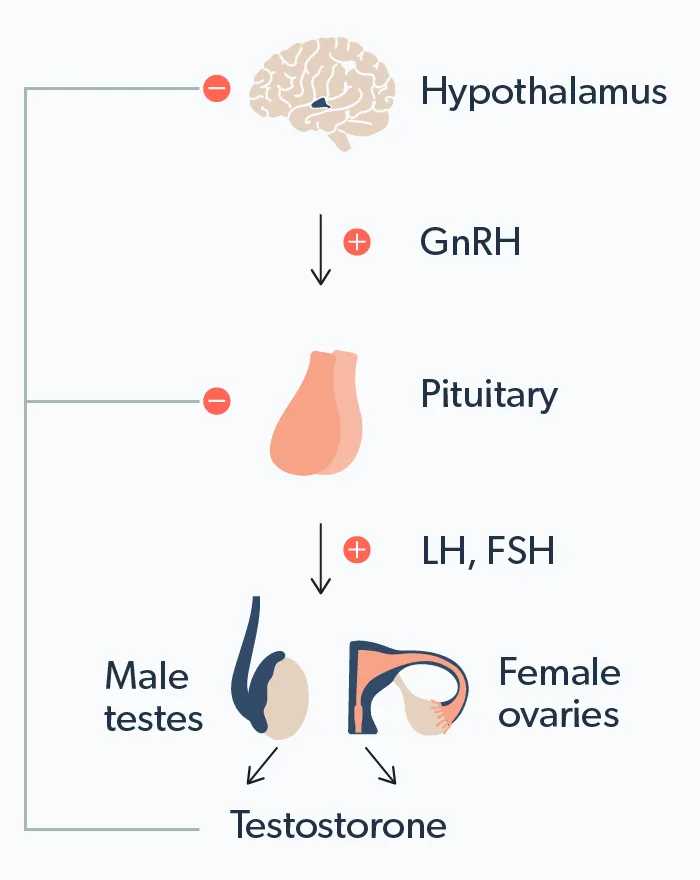
Males typically have 20–25 times the amount of testosterone as females. In females, testosterone is made by the theca cells of the ovary, but most of it is converted to estrogen by an enzyme called aromatase. Despite these lower levels, testosterone is still crucial for normal female sexual function (Fabbri, 2016).
In both sexes, a small amount of testosterone is also made in the adrenal glands, which are part of the endocrine system and sit on top of the kidneys.
What does testosterone do?
While testosterone is important during puberty for developing sexual maturity in males, it continues to be important in men and women throughout life. In men, testosterone plays a major role in:
Libido (sex drive)
Erectile function
Sperm production
Maintaining bone density and muscle mass
Red blood cell production
Growth of facial and body hair
Mood regulation
Testosterone is also important in women, playing roles in (Tyagi, 2017):
Sex drive (libido)
Maintaining muscle mass and bone density
Mood and energy levels
Fertility
It’s no wonder abnormal testosterone levels can cause so many different symptoms! In both males and females, it’s important to have testosterone levels that are within a normal range. T levels that are too high or too low can cause different side effects in males and females.
Low testosterone
Testosterone levels typically start to drop in your 30s and 40s. Your levels normally vary quite a bit throughout the day, being highest in the morning. They can also change day to day depending on many factors.
Most providers typically check two early-morning testosterone levels (usually 8–10 am) on different days before diagnosing low testosterone (aka hypogonadism). Repeatedly low morning testosterone levels suggest that you may have chronic and ongoing testosterone deficiency.
A low level is usually defined as being <300 ng/dL. In addition to aging, medical conditions that cause low T include (Sizar, 2021):
Sleep problems, like sleep apnea
Genetic diseases (e.g., Klinefelter syndrome)
Certain types of infections (e.g., mumps, HIV)
Drugs (e.g., glucocorticoids)
Treatments like chemotherapy and radiation
Pituitary problems (e.g., prolactinomas)
Trauma
A healthcare provider will take a detailed history, perform a physical exam, order specific blood tests, and sometimes recommend imaging to determine any underlying causes for your low T.
Symptoms of low testosterone
Since testosterone affects so many bodily functions, low levels can have a wide range of seemingly unrelated signs and symptoms, such as (Sizar, 2021):
Decreased libido
Erectile dysfunction (with loss of morning erections)
Fatigue
Loss of muscle mass
Increased body fat
Anemia
Loss of bone mass (osteoporosis)
Depressed mood
Fertility issues (e.g., low sperm count)
Too much testosterone
Having too much testosterone is also not a good thing, and it can happen to both men and women. In men, the most common source of too much testosterone is using anabolic steroids or taking too high a dose of testosterone prescribed by a healthcare provider.
Anabolic steroids are drugs made from testosterone but designed to affect muscle and tissue growth rather than sexual functions. It may seem counterintuitive, but taking these drugs inhibits the body’s own natural testosterone production, causing the body’s testosterone hormone levels to decrease (Ganesan, 2021).
Symptoms of high testosterone
When men take too much testosterone (or anabolic steroids), they can experience symptoms like (Ganesan, 2021):
Acne, including body acne (aka “backne” when it appears on the back)
Enlarged prostate
Breast enlargement (gynecomastia) due to some of the testosterone being converted to estrogen by a process called “aromatization.”
Increased cholesterol levels
Higher risk of heart disease
Weight gain
Decreased testicle size
Erectile dysfunction
Women can suffer from hyperandrogenism, a condition where testosterone or other androgens (such as DHEA) are too high. Several conditions cause hyperandrogenism in females, including (Nassar, 2021):
Polycystic ovary syndrome (PCOS)
Ovarian or adrenal tumors
Cushing syndrome
Certain drugs
The most common cause of high testosterone levels in women is PCOS, which occurs in up to 12% of women and is the most common female endocrine disorder. Some common signs of hyperandrogenism in females include (Rasquin, 2021):
Menstrual irregularities
Infertility
Hirsutism (excess facial and body hair)
Acne
People with these symptoms should see their healthcare provider for a physical exam and testing to determine the cause of hyperandrogenism—treatment often depends on the cause.
Treatment of low testosterone
Your provider will look for potential causes of your low T before recommending a treatment option—identifying a cause helps develop a targeting treatment plan. Examples would be weight loss in people with obesity and treating sleep apnea in affected people.
If you and your provider cannot pinpoint a specific cause for your low T, there are some drug options out there.
Clomiphene citrate is a drug known as a selective estrogen receptor modulator (SERM). Clomiphene works by tricking the pituitary into making more luteinizing hormone (LH) and follicle-stimulating hormone (FSH), two compounds that affect testosterone and sperm production in testicles. Since taking testosterone can worsen sperm count, people with low T who want to preserve their fertility may benefit from clomiphene (Krzastek, 2019).
Clomiphene Important Safety Information: Read more about serious warnings and safety info.
Another potentially surprising drug that may help increase T levels is human chorionic gonadotropin (hCG). HCG is a hormone found in high levels during pregnancy and is what’s tested in pregnancy tests. HCG serves other functions in the body, though, and taking it may increase testosterone in people with low T and functioning testicles (Salonia, 2019).
Testosterone replacement therapy (TRT) is used for people who cannot manufacture their own T and no longer desire fertility. It comes in various forms, including:
Injections
Topical gels
Mouth patch or troche (a small lozenge that dissolves in the cheek or under the tongue)
Pellets implanted under the skin
A new oral formulation (FDA, 2019)
All testosterone products have a boxed warning that they may increase the risk of cardiovascular disease, including heart attacks and strokes. This was based on some studies showing that TRT may increase these risks. Other studies have shown that TRT did not increase the risks of cardiovascular events and may even reduce these risks (Cheetham, 2017). There is a need for ongoing research to determine the true cardiovascular effects of testosterone therapy.
Before starting low T treatment or testosterone therapy, consult your healthcare provider and discuss your symptoms and concerns—together with your provider, you can discover the path that is right for you.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Cheetham, T. C., An, J., Jacobsen, S. J., Niu, F., Sidney, S., Quesenberry, C. P., et al. (2017). Association of testosterone replacement with cardiovascular outcomes among men with androgen deficiency. JAMA Internal Medicine , 177 (4), 491–499. doi: 10.1001/jamainternmed.2016.9546. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28241244/
Fabbri, E., An, Y., Gonzalez-Freire, M., Zoli, M., Maggio, M., & Studenski, S., et al. (2016). Bioavailable testosterone linearly declines over a wide age spectrum in men and women from the Baltimore longitudinal study of aging. Journals of Gerontology Series A: Biological Sciences and Medical Sciences , 71 (9), 1202-1209. doi: 10.1093/gerona/glw021. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26921861/
Ganesan, K., Rahman, S., & Zito, P. M. (2021). Anabolic steroids. [Updated 2021, Jun 4]. In: StatPearls [Internet]. Retrieved on Jan. 6, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK482418/
Krzastek, S. C., Sharma, D., Abdullah, N., Sultan, M., Machen, G. L., Wenzel, J. L., et al. (2019). Long-term safety and efficacy of clomiphene citrate for the treatment of hypogonadism. The Journal of Urology , 202 (5), 1029–1035. doi: 10.1097/JU.0000000000000396. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31216250/
Nassar, G. N. & Leslie, S. W. (2021). Physiology, testosterone. [Updated 2021, Jan 9]. In: StatPearls [Internet]. Retrieved on Jan. 6, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK526128/
Rasquin Leon, L. I., Anastasopoulou, C., & Mayrin, J. V. (2021). Polycystic ovarian disease. [Updated 2021 Jul 21]. In: StatPearls [Internet]. Retrieved on Jan. 6, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK459251/
Salonia, A., Rastrelli, G., Hackett, G., Seminara, S. B., Huhtaniemi, I. T., Rey, R. A., et al. (2019). Paediatric and adult-onset male hypogonadism. Nature Reviews Disease Primers , 5 (1), 38. doi: 10.1038/s41572-019-0087-y. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6944317/
Sizar, O. & Schwartz, J. (2021). Hypogonadism. [Updated 2021, Jun 29]. In: StatPearls [Internet]. Retrieved on Jan. 6, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK532933/
Tyagi, V., Scordo, M., Yoon, R. S., Liporace, F. A., & Greene, L. W. (2017). Revisiting the role of testosterone: are we missing something?. Reviews in Urology , 19 (1), 16–24. doi: 10.3909/riu0716. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5434832/
U.S. Food & Drug Administration (FDA). (2019, March 27). FDA approves new oral testosterone capsule for treatment of men with certain forms of hypogonadism. Retrieved on Jan. 5, 2022 from https://www.fda.gov/news-events/press-announcements/fda-approves-new-oral-testosterone-capsule-treatment-men-certain-forms-hypogonadism










