Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Heart arrhythmias are a broad category of conditions where the heart rate or the rhythm of the heartbeat is abnormal.
These conditions occur because of a change in the normal flow of electrical impulses that trigger the heart to squeeze (contract) and relax irregularly. The heart may beat too fast, too slow, skip a beat, or it can have extra beats. Arrhythmias are common and not dangerous for most people, however, some cases can have life-threatening consequences. The heart needs to pump normally to push blood throughout the body to nourish your tissues and organs, and it can be dangerous when an arrhythmia interferes with that ability.
How does the heart work? The heart is made up of four chambers: two smaller chambers (left and right atria) and two larger chambers (left and right ventricles). Blood enters the atria of the heart, and then a series of coordinated actions occurs:
A collection of specialized cells in the right atrium, called the sinoatrial (SA) node, sends an electrical impulse that spreads to both the left and right atria, telling them to contract. This SA node is sometimes referred to as the “natural pacemaker” of the heart (AHA-a, 2016).
When the atria contract, they force the blood from the atria into the corresponding ventricles.
Another node, the atrioventricular (AV) node, gets activated and sends an impulse to both ventricles telling them to contract.
When the two ventricles contract, it forces blood out of the heart and into the major arteries where it travels to other parts of the body.
This cycle repeats itself with each heartbeat to keep the blood circulating regularly. In a healthy resting adult, the heart beats 60–100 times per minute (AHA-a, 2016). Since so much happens in such a short amount of time (the span of a heartbeat), you can see why it is vital for the heart to pump regularly to circulate blood efficiently.
What are the different types of arrhythmias?
Arrhythmias are categorized based on whether they cause the heart to beat too fast or too slow, whether they are due to a problem in the atria or ventricles, and whether they are regular or irregular.
Supraventricular tachycardias (SVTs)
Supraventricular tachycardias (SVTs) refer to arrhythmias that start in the atria and cause the heart to beat faster than 100 beats per minute; types of SVTs include:
Atrial fibrillation: The most common form of arrhythmia is atrial fibrillation (also called afib); approximately 2.7 million Americans are living with atrial fibrillation, according to the American Heart Association (AHA). Atrial fibrillation is a form of tachycardia, in which the heart beats much faster than normal, often 175 beats per minute or higher (AHA-b, 2016). The atria of the heart are contracting irregularly and too quickly to allow the heart to fill up with blood in between beats; this can cause blood pooling in the atria, which leads to blood clots, heart attacks, strokes, heart failure, and other complications. Atrial fibrillation is more common in older people and people with high blood pressure.
Atrial flutter: This is another type of tachycardia that involves the atria of the heart. Unlike atrial fibrillation, which is irregular, atrial flutter is a fast and regular heart rhythm. In atrial flutter, when the SA node sends out the electrical impulse, part of it gets caught in a loop pathway around the right atrium. This impulse loop causes the atria to beat faster than the ventricles. Rapid electrical signals cause the muscles in the atria to contract quickly, leading to a steady, atrial rate of 250–320 beats per minute. Fortunately, the AV node does not allow the ventricles to contract this quickly, and people with atrial flutter can have fast (150 beats per minute) or normal heart rates (ventricular rates)—depending on the function of their AV node. Again, when the atria beat too quickly, they cannot squeeze out the blood, leading to blood pooling and blood clots. Atrial flutter is more common in people with heart disease or who have had a previous heart attack or heart surgery.
Paroxysmal supraventricular tachycardia (PSVT): In PSVT, electrical signals that start in the atria travel to the ventricles and cause extra heartbeats. This arrhythmia starts and stops suddenly and can happen during physical exertion. It is usually not dangerous and tends to occur in young people, especially ones who suffer from anxiety. Also, it is more common in children, women, and people who drink large amounts of alcohol or caffeinated beverages.
Ventricular arrhythmias
Ventricular arrhythmias start in the ventricles and usually cause the heart to beat too fast.
Ventricular tachycardias: In ventricular tachycardia, the electrical signals originating in the ventricles are firing faster than normal and are interfering with the impulses coming from the SA node. This leads to a heartbeat that is faster than normal; this rapid heartbeat keeps the atria and ventricles from filling up with blood and decreases the amount of blood pumped to the rest of the body. A few beats of ventricular tachycardia often do not cause problems, but episodes that last for more than a few seconds can be dangerous. It usually occurs in people with a history of coronary artery disease or heart attack. If it is not treated appropriately, it can lead to very fast and prolonged tachycardias that do not effectively pump blood around the body, or it can turn into ventricular fibrillation, a life-threatening condition.
Ventricular fibrillation (V-fib): The most dangerous arrhythmia is ventricular fibrillation. In this condition, disorganized electrical signals make the ventricles quiver instead of pumping regularly. If the ventricles cannot pump blood to the rest of the body, sudden cardiac arrest and death can occur within minutes. This type of arrhythmia is life-threatening and a medical emergency.
Bradycardias
Bradycardias are arrhythmias that cause a slow heart rate—slower than 60 beats per minute. Some people, especially people who are healthy young adults and elite athletes, can have slow heart rates normally. Your heart rate can also drop below 60 beats per minute when you are asleep. However, for some people, especially older adults, bradycardia can decrease the amount of blood flowing into the body; this leads to the symptoms of fatigue, lightheadedness, shortness of breath, fainting, and cardiac arrest (in extreme cases).
Sick sinus syndrome: This is a specific type of bradycardia where the SA node is not firing correctly, causing a slower heart rate. Because the SA is not acting normally, people with this condition can have heart rates that alternate between being too slow and too fast.
Conduction disorders or heart block: Bradycardia can occur because the electrical impulses are not getting from the atria to the ventricles; the signals are blocked, and this leads to a slower heart rate. A block can occur anywhere along the electrical pathways of the heart. Certain kinds of heart block may not result in a slow heart rate but need to be treated anyway because they are unstable.
Premature ventricular contraction (PVC)
Most people have had the sensation that their heart has “skipped a beat.” This is called premature ventricular contraction (PVC) and happens when the signal to beat comes early and starts in the ventricles, rather than in the atria like usual; this feels like your heart skipped a beat. This extra heartbeat interferes with your normal rhythm, creating a pause which is followed by a stronger beat when your heartbeat goes back to normal. Occasional PVCs are normal in adults and are common in children and teenagers; usually, they go away on their own.
Causes of arrhythmias
Several factors can cause arrhythmias; they can be caused by damage to heart tissue, or they can occur suddenly due to physical exertion, stress, medication, or problems with the electrical signaling pathways in the heart. Sometimes the cause of an arrhythmia is unclear. Known causes of arrhythmias include:
A heart attack or scarring from a prior heart attack
Coronary artery disease (plaque buildup in the arteries that feed the heart)
Conditions that affect your heart’s overall structure, like cardiomyopathy
High blood pressure
Thyroid problems
Dehydration
Abnormal levels of electrolytes like potassium, magnesium, sodium, or calcium in your blood
Certain over-the-counter medicines, such as allergy and cold medicines
Smoking
Drinking too much alcohol or caffeine
Drug abuse, especially amphetamines and cocaine
Genetics
Signs and symptoms of arrhythmias
Arrhythmias do not always cause symptoms and are sometimes discovered during a routine checkup. Sometimes they can be hard to detect during checkups because the symptoms come and go and may not be present while you are with your doctor. Common signs and symptoms of arrhythmias include:
Fluttering or quivering heartbeat (palpitations)
A racing heartbeat or a slow heartbeat
Chest pain or pressure
Shortness of breath
Weakness, dizziness, and lightheadedness
Fainting (syncope)
Confusion
Fatigue
Collapse and sudden cardiac arrest in extreme cases
Diagnosis of arrhythmias
The diagnosis of arrhythmias disease begins with a physical exam by your healthcare provider. Your provider will check your pulse, listen to your heart (to check for a heart murmur), listen to your lungs (to see if there is any fluid buildup), and check your feet for any swelling. You may need to be referred to a cardiology specialist (a provider who specializes in diseases of the heart) for additional testing, including:
Electrocardiogram (ECG or EKG): This is the most common test used to diagnose arrhythmias; it looks at the electrical activity of the heart to see if the heart is beating irregularly or at an abnormal rate.
Holter monitors or event monitors: These are portable ECGs that provide information about how your heart is functioning during daily activities.
Tilt table test: This test is used, especially if you have had fainting spells. You lie flat on the table, and your provider checks your heart rate and blood pressure. Then the table is tilted so that you are positioned as if you were standing up. Your provider continuously monitors your heart rate and blood pressure to see how they change when you are in different positions. This information can help your provider determine if your fainting spells are due to position changes vs. arrhythmias.
Electrophysiology study (EPS): This study looks at the electrical activity of your heart by inserting thin catheters tipped with electrodes into the heart. With these catheters, your provider can see how electrical impulses travel across the heart. Your provider can also trigger and stop arrhythmias with these catheters, allowing for more accurate information about your arrhythmia, such as where it occurs, what may be causing it, and what therapies may treat it.
Stress test: You are asked to exercise on a treadmill or are given medications to make your heart beat faster to simulate exercise, while pictures are taken of your heart to see how it functions under stress.
Echocardiogram: Echocardiograms use sound waves to create a picture of your heart and how well the heart is pumping blood, and if there is any pooling of blood or blood clots.
Blood tests: Using these tests, your provider can look for thyroid problems, electrolyte imbalances, or other conditions that may lead to arrhythmias.
Treatment of arrhythmias
According to the AHA, there are several goals that your provider may use to guide your treatment plan:
Preventing blood clots from forming to reduce stroke risk, especially if you have atrial fibrillation
Keeping your heart rate within a healthy range
Restoring your heart’s normal rhythm
Treat any existing heart disease/condition as it may be causing or contributing to your arrhythmia
Decreasing other risk factors for heart disease and stroke
One thing that you can do for yourself to improve your overall heart health is to adopt a heart-healthy lifestyle:
Diet low in sodium and saturated fat and rich in fruits and vegetables
Keep a healthy weight; obesity is a risk factor for heart disease
Minimize stress
Exercise several times a week
Quit smoking
Avoid too much caffeine, which can increase your heart rate
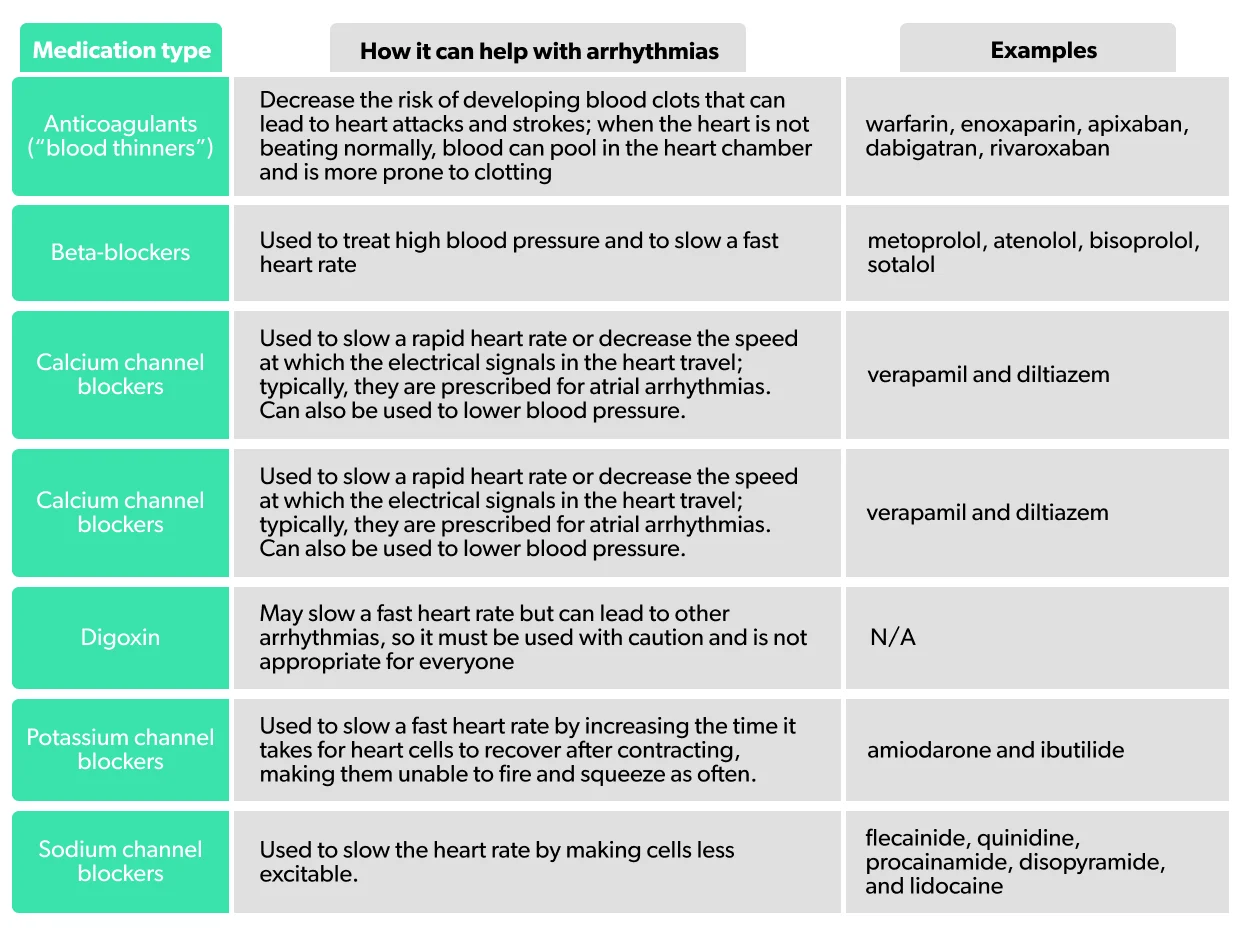
While some arrhythmias may not cause any symptoms, they may put you at risk of serious complications, including stroke, heart failure, worsening arrhythmias, and sudden cardiac arrest. For this reason, in some people, treatment may include medications, procedures, or both. You should be aware that some drugs used to treat arrhythmias (antiarrhythmics) can trigger arrhythmias if the dose is too high; be sure to talk to your provider about any symptoms you may have after starting these medications.
For some people, like those with bradycardia (slow heart rate), there are no medications that reliably increase the heart rate; for others, medication is not sufficient to control their arrhythmia. These cases may require the implantation of a pacemaker or an implantable cardiac defibrillator (ICD). A pacemaker is a small electrical device that is implanted into the body and regulates the heartbeat. It is implanted under the skin of the chest with wires that travel to the heart; when it senses that the heartbeat is too fast or too slow, it sends an electrical impulse to the heart to restore the normal rate and rhythm. An ICD is similar to a pacemaker in that it is also a small electrical device implanted under the skin with wires running to the heart. The ICD continuously monitors your rhythm, and if it notices that your heart has an abnormal rhythm, it gives a small shock to reset the heart rhythm. This type of device is used in people who have a high risk of developing a dangerously fast or irregular heartbeat, like ventricular tachycardia or ventricular fibrillation, as these arrhythmias can lead to sudden cardiac arrest and death.
Another option for treating your arrhythmia is resetting your heart rhythm back to its regular rhythm (also called normal sinus rhythm); this process is called cardioversion and can be accomplished via medication or a procedure. In the procedure, a brief, low-energy electrical shock is delivered to your heart through patches (electrodes) on your chest; this shock allows your heart’s electrical activity to reset to normal sinus rhythm.
For some, surgical procedures, like a catheter ablation or maze procedure, may be needed. Ablation kills the heart tissue that is causing the abnormal electrical signals or isolates the abnormal cells by creating a scar around them that does not conduct electrical activity. In catheter ablation, a thin tube is inserted into a blood vessel in your groin and guided into your heart. Once in place, the catheter tip destroys the areas of the heart that are producing the abnormal electrical signals and causing the arrhythmias. During a maze procedure, the surgeon performs open-heart surgery and makes several cuts in abnormal heart tissue, creating scars that interfere with the irregular electrical impulses. Since scar tissue stops the electrical impulses, this procedure allows the heart to return to a normal rhythm.
If you have any underlying conditions contributing to your arrhythmia (like an electrolyte imbalance, high blood pressure, heart disease, sleep apnea, or thyroid disease), these will need treatment as well.
Lastly, there are specific techniques that you can do on your own, under the guidance of your physicians, to slow a fast heart rate if it is caused by certain rhythms. These maneuvers affect the vagus nerve, which helps control the heart rate and can stimulate the body’s relaxation response. These movements, called vagal maneuvers, include:
Holding your breath and bearing down (also called the Valsalva maneuver)
Coughing
Putting a towel dipped in ice-cold water over your face or dunking your face in ice-cold water
In conclusion
Arrhythmias can be scary, but they are manageable. See your provider for regular checkups and take all of your medication as prescribed. Learn how to monitor your pulse and manage your risk factors. Be sure to maintain open lines of communication; tell your healthcare provider right away if you experience any new or worsening symptoms.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
American Heart Association (AHA-a). (2016, September 30). About Arrhythmia. Retrieved Nov. 27, 2019 from https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia
American Heart Association (AHA-b). (2016, July 31). What is Atrial Fibrillation. Retrieved Nov. 27, 2019 from https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af