Key takeaways
Semaglutide, the active ingredient in Ozempic, may be linked to a lower risk of dementia and cognitive decline compared to other medications that lower blood sugar, according to the findings of a new study.
The researchers also found that people taking semaglutide had a lower risk of 20 other brain and psychological disorders, when compared to other diabetes drugs.
While this is just one study, the research suggests that semaglutide may have more impacts on the brain beyond regulating appetite.
Here's what we'll cover
Here's what we'll cover
Key takeaways
Semaglutide, the active ingredient in Ozempic, may be linked to a lower risk of dementia and cognitive decline compared to other medications that lower blood sugar, according to the findings of a new study.
The researchers also found that people taking semaglutide had a lower risk of 20 other brain and psychological disorders, when compared to other diabetes drugs.
While this is just one study, the research suggests that semaglutide may have more impacts on the brain beyond regulating appetite.
The list of conditions Ozempic (semaglutide) can treat continues to grow. From weight loss to improving type 2 diabetes to lowering cardiovascular risk, it’s clear Ozempic is a powerful medication.
Soon, there may be yet another condition to add to the list. People taking Ozempic for type 2 diabetes had a lower risk of cognitive decline and dementia compared to sitagliptin and glipizide (two other anti-diabetic medications) , according to the results of a recent study.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
What is semaglutide?
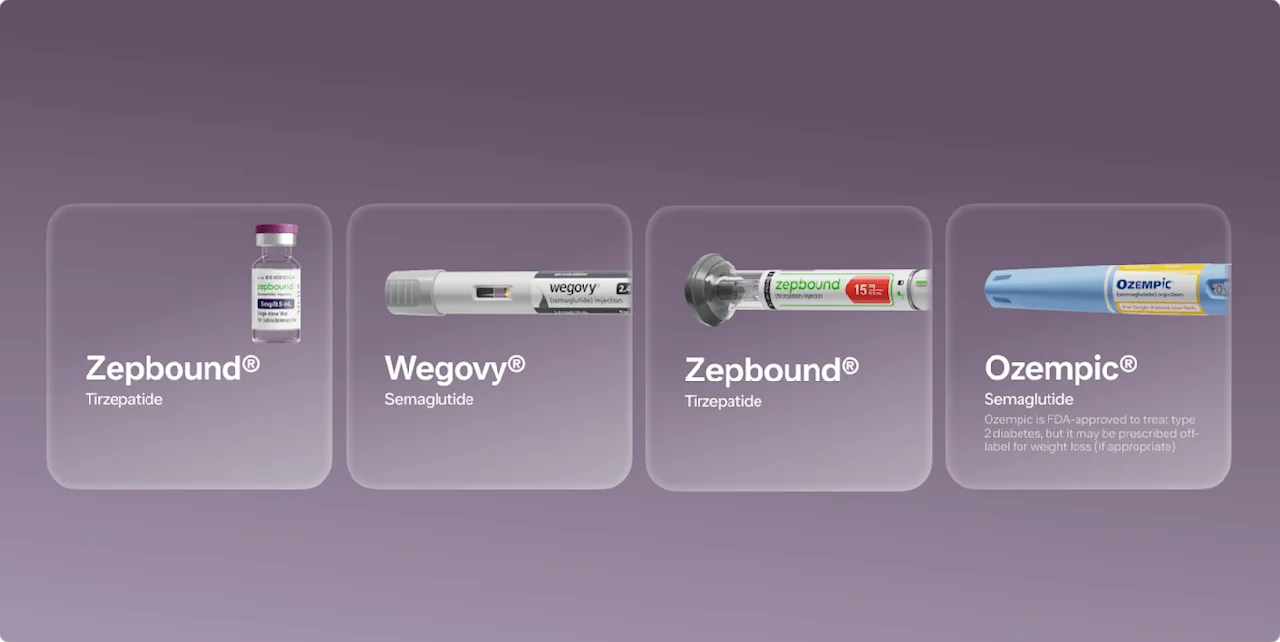
Semaglutide is the active ingredient in the GLP-1 drugs Ozempic, Wegovy, and Rybelsus. Ozempic and Rybelsus are both FDA-approved to help control blood sugar in people with type 2 diabetes, while Ozempic is additionally FDA-approved to lower cardiovascular risk in people with type 2 diabetes and heart disease. Wegovy, which contains higher dosage strengths of semaglutide, is FDA-approved for weight loss in people with obesity and overweight who also have weight-related medical problems.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
Can semaglutide (Ozempic) lower the risk of cognitive decline?
Potentially when compared with other blood glucose-lowering medications, according to the results of a study published in The Lancet last month.
The study reviewed the medical records of over 100 million patients taking semaglutide (Ozempic) vs. other diabetes medications, including empagliflozin (Jardiance), glipizide (Glucotrol), and sitagliptin (Januvia), between December 2017 and May 2021. The researchers found that, when compared to other diabetes drugs, people taking Ozempic had a lower risk of developing more than 20 neurological and psychiatric disorders within a 12-month period.
Specifically, people taking semaglutide had a:
28% lower risk of cognitive decline compared to sitagliptin and glipizide
48% lower risk of dementia compared to sitagliptin
18%–28% lower risk of nicotine misuse compared to glipizide and empagliflozin
The full list of neuropsychiatric disorders studied included:
Parkinson’s disease
Cognitive decline
Dementia
Epilepsy and seizure disorders
Migraine
Insomnia
Stroke
Alcohol, opioid, cannabis, stimulants, and nicotine addiction or abuse
Psychosis
Bipolar disorder
Obsessive compulsive disorder
Suicidality
When compared to the other three diabetes drugs studied, the people taking Ozempic had a lower risk of developing nearly all of the disorders above within a 12-month period. The only exception was migraine. The findings are also notable because they did not find that Ozempic raised the risk of depression, anxiety, or suicidal thoughts. There has been some concerns about the link between GLP-1 drugs and suicidal thoughts or behavior, and the FDA has received some reports of suicidal thoughts in people taking Wegovy and other GLP-1 drugs. Currently, however, these warnings only apply to Wegovy and Saxenda, but not Ozempic.
When it comes to Ozempic and a lower risk of dementia, it’s worth noting that the research findings were based on medical records rather than a randomized controlled trial. And it’s important to remember that we can’t say for sure whether Ozempic lowers the risk of these disorders. All we have observed in the study, is that compared to other diabetes medications taking Ozempic appeared to have a lower risk of some of the neurocognitive side effects.
Further research is still needed to see if the same can be said of other GLP-1s or of people without type 2 diabetes.
With those caveats out of the way, the findings are still quite exciting, especially given that previous research has shown that people with obesity and dementia—both conditions that semaglutide treats—have a higher risk of dementia and cognitive decline.
“These findings are fascinating and do not completely surprise me,” said Dr. Rachel Goldman, PhD, FTOS, FASMBS-IH, Licensed Psychologist and Clinical Assistant Professor at NYU Grossman School of Medicine. “With more research coming out each day, we are going to continue to learn new things about these medications and the impact they have on our health, including our brain health.”
Saxenda Important Safety Information: Read more about serious warnings and safety info.
Can semaglutide affect memory?
“As seen by the results of this study, there is evidence that semaglutide is associated with lower risk of cognitive decline, but more research is needed to fully understand this association,” said Dr. Goldman. “We do know though that these medications are impacting the brain, as [semaglutide is] decreasing food noise, causing people to have less appetite [and] less cravings, but how this is really impacting brain health and cognition is still being studied.”
The GLP-1 receptors semaglutide activates are prominent in the brain, and several early studies from the 2000s have shown that GLP-1 has neuroprotective effects. For example, while GLP-1 signaling in the hippocampus and hypothalamus has been shown to reduce appetite, it’s also shown to improve memory function. “There have been some studies in mice that showed semaglutide can increase the expression levels of SIRT1 and GLUT4 in the hippocampus, which was associated with improvements in learning and memory,” said Dr. Goldman. “Some are saying this is related to how semaglutide is improving nerve cells and inflammation which could be related to lowering the risk of cognitive decline, dementia, and Alzheimer's disease.”
There is a difference between prevention and treatment. The research on semaglutide’s effects on memory is still developing, so we won’t know Ozempic’s potential for treating Alzheimer’s disease or dementia for some time. But, Novo Nordisk, the maker of Ozempic and Wegovy, is currently conducting two clinical trials to specifically study the effects of semaglutide on early Alzheimer’s disease. The results are expected to be published in 2025.
Can semaglutide cause confusion?
“In terms of [semaglutide] causing confusion, like anything else that impacts our brain, it's possible,” said Dr. Goldman. “But more research is needed to understand this association and if Ozempic is really "causing" it or if there are other factors involved, such as consuming less food or being dehydrated.”
Another possible cause may be low blood sugar, which can be a side effect of Ozempic. Confusion can be a symptom of low blood sugar, or hypoglycemia, along with dizziness, headache, blurred vision, and a rapid heartbeat. However, low blood sugar can occur with other diabetes medications that lower blood sugar, too, so this isn’t necessarily exclusive to Ozempic. If you are taking other medications that can lower blood sugar, be sure to tell your healthcare provider before starting semaglutide because doses may need to be adjusted accordingly.
GLP1s, such as semaglutide, and the brain
This latest study is part of a growing body of research exploring the effects of GLP-1s, particularly semaglutide, on brain health and function. Some researchers have suggested that semaglutide’s ability to fight inflammation in the brain may have neuroprotective effects that could have benefits for Alzheimer’s, Parkinson’s disease, and dementia. These findings could be powerful, especially given the link between obesity and diabetes (which semaglutide treats) and dementia.
Obesity is considered a risk factor for diabetes, as well as Alzheimer’s disease and other types of dementia. And, people with obesity and diabetes both have a higher risk of dementia.
Fortunately, treating obesity and diabetes (which GLP-1s like semaglutide can help with) may be able to reduce the risk of cognitive decline and dementia. Studies have found that people who take medication like metformin to manage their type 2 diabetes have a lower risk of developing dementia. Moreover, those who take metformin on a longer-term basis have an even lower risk. Diet and exercise, both considered cornerstone treatments for both obesity and diabetes, have also been shown to stave off dementia.
Bottom line
This latest study suggests that taking Ozempic (semaglutide) does not increase an individual’s risk of dementia or other disorders when compared to other diabetes medications.. In fact, when compared to other diabetes medications, semaglutide may actually reduce the risk of cognitive decline and dementia.
“We know that individuals with obesity have a higher risk of developing diabetes and those with diabetes have an increased risk of developing a cognitive disorder, such as dementia,” said Dr. Goldman. “It would make sense that if we are treating someone's obesity and diabetes (regardless of which treatment option), that they would then have a lower risk of developing cognitive disorders, including dementia.”
“There are several treatment options available for both diabetes and obesity, including medication (such as GLP-1s), but there's also bariatric surgery, as well as lifestyle change,” said Dr. Goldman.
Keep in mind that this study suggests semaglutide leads to a lower risk of cognitive issues than other medications that lower blood sugar. Further research is needed to check whether this still holds true when comparing people who use semaglutide to people who do not use any blood glucose-lowering medication.
For many people, treatment paired with lifestyle changes is needed to manage obesity, says Goldman. If you’re interested in learning more about GLP-1 medication and whether you may qualify, Ro healthcare providers can meet with you to discuss your goals and decide whether medication may be right for you.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Blundell, J., Finlayson, G., Axelsen, M., et al. (2017). Effects of once-weekly semaglutide on appetite, energy intake, control of eating, food preference and body weight in subjects with obesity. Diabetes, Obesity & Metabolism, 19(9), 1242–1251. doi: 10.1111/dom.12932. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5573908/
ClinicalTrials.gov-a. (2024). A Research Study Investigating Semaglutide in People With Early Alzheimer's Disease (EVOKE). National Library of Medicine. Retrieved Jul. 25, 2024 from https://clinicaltrials.gov/study/NCT04777396
ClinicalTrials.gov-b. (2024). A Research Study Investigating Semaglutide in People With Early Alzheimer's Disease (EVOKE Plus). National Library of Medicine. Retrieved Jul. 25, 2024 from https://clinicaltrials.gov/study/NCT04777409
De Giorgi, R., Koychev, I., Adler, A. I., et al. (2024). 12-month neurological and psychiatric outcomes of semaglutide use for type 2 diabetes: a propensity-score matched cohort study. EClinicalMedicine, 102726. doi: 10.1016/j.eclinm.2024.102726. Retrieved from https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(24)00305-5/fulltext
Flores-Cordero, J. A., Pérez-Pérez, A., Jiménez-Cortegana, C., et al. (2022). Obesity as a Risk Factor for Dementia and Alzheimer's Disease: The Role of Leptin. International Journal of Molecular Sciences, 23(9), 5202. doi: 10.3390/ijms23095202. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9099768/
Kopp, K. O., Glotfelty, E. J., Li, Y., et al. (2022). Glucagon-like peptide-1 (GLP-1) receptor agonists and neuroinflammation: Implications for neurodegenerative disease treatment. Pharmacological Research, 186, 106550. doi: 10.1016/j.phrs.2022.106550. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9712272/
Ma, Y., Ajnakina, O., Steptoe, A., et al. (2020). Higher risk of dementia in English older individuals who are overweight or obese. International Journal of Epidemiology, 49(4), 1353–1365. doi: 10.1093/ije/dyaa099. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7660153/
Reich, N. & Hölscher, C. (2022). The neuroprotective effects of glucagon-like peptide 1 in Alzheimer's and Parkinson's disease: An in-depth review. Frontiers in Neuroscience, 16, 970925. doi: 10.3389/fnins.2022.970925. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9475012/
Selman, A., Burns, S., Reddy, A. P., et al. (2022). The Role of Obesity and Diabetes in Dementia. International Journal of Molecular Sciences, 23(16), 9267. doi: 10.3390/ijms23169267. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9408882/
US Food & Drug Administration (FDA-a). (2023). Highlights of Prescribing Information: Ozempic (semaglutide) injection, for subcutaneous use. Retrieved Jul. 8, 2024 from https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/209637s020s021lbl.pdf
US Food & Drug Administration (FDA-a). (2024). Highlights of Prescribing Information: Rybelsus (semaglutide) tablets, for oral use. Retrieved Jul. 8, 2024 from https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/213051s018lbl.pdf
US Food & Drug Administration (FDA-b). (2023). Highlights of Prescribing Information: Saxenda (liraglutide) injection, for subcutaneous use. Retrieved Jul. 8, 2024 from https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/206321s016lbl.pdf
US Food & Drug Administration (FDA-b). (2024). Highlights of Prescribing Information: Wegovy (semaglutide) injection, for subcutaneous use. Retrieved Jul. 8, 2024 from https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/215256s011lbl.pdf
Wang, Z. J., Li, X. R., Chai, S. F., et al. (2023). Semaglutide ameliorates cognition and glucose metabolism dysfunction in the 3xTg mouse model of Alzheimer's disease via the GLP-1R/SIRT1/GLUT4 pathway. Neuropharmacology, 240, 109716. doi: 10.1016/j.neuropharm.2023.109716. Retrieved from https://pubmed.ncbi.nlm.nih.gov/37730113/
Zheng, B., Su, B., Ahmadi-Abhari, S., et al. (2023). Dementia risk in patients with type 2 diabetes: Comparing metformin with no pharmacological treatment. Alzheimer's & Dementia: The Journal of the Alzheimer's Association, 19(12), 5681–5689. doi: 10.1002/alz.13349. Retrieved from https://pubmed.ncbi.nlm.nih.gov/37395154/