Insurance Support
Navigating benefits and leveraging scaled insights to help patients secure coverage of GLP-1 medications

Benefits verification and cost estimates
Optimized prior authorizations
Scaled coverage insights
Simplifying insurance coverage and approvals
Patients benefit from end-to-end insurance navigation that maximizes their treatment access and helps providers put together the best possible care plan.
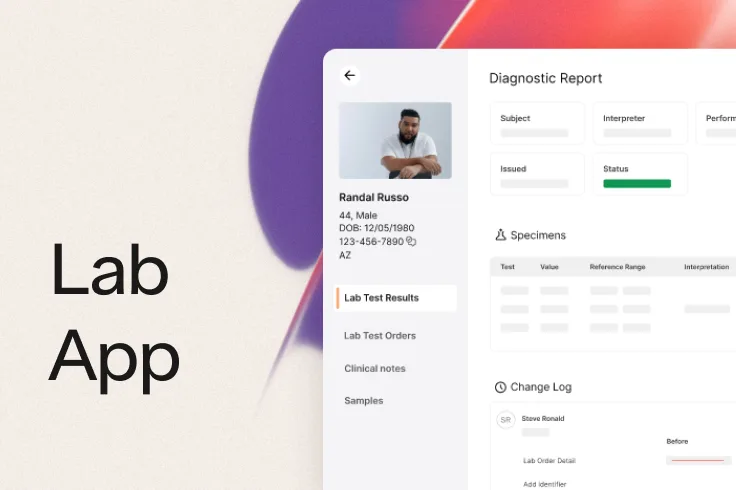
Benefits verification and cost estimates
When a patient wants to use insurance, Ro takes on benefits verification and clearly communicates their treatment options, coverage details, and transparent cost estimates when available.


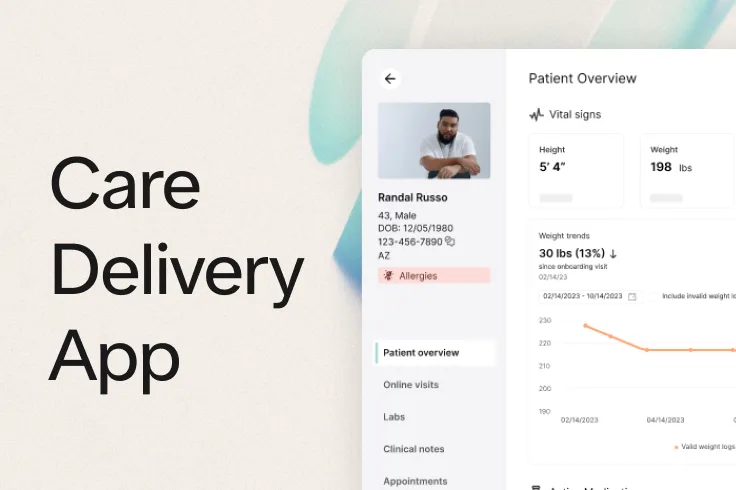
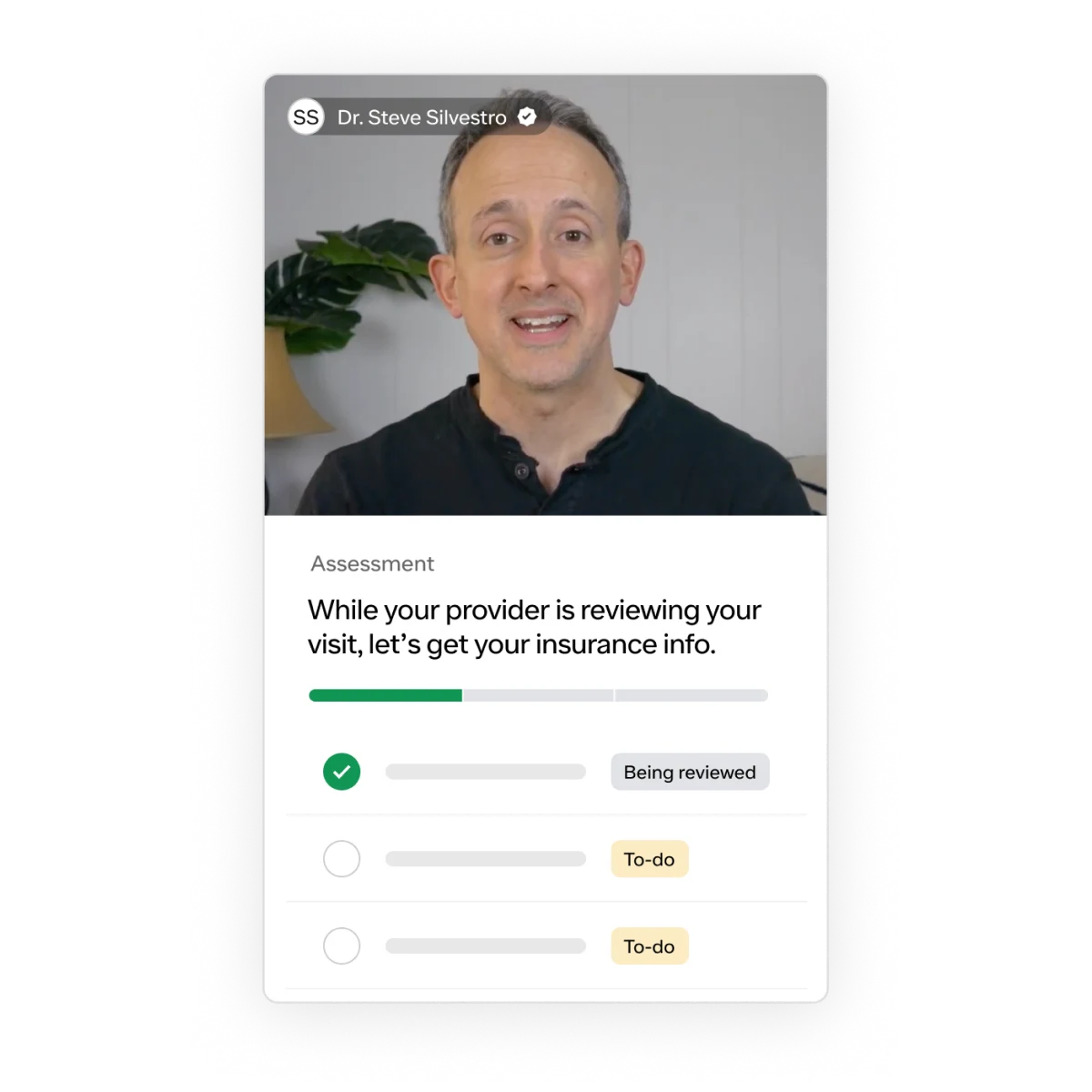
Optimized prior authorizations
Ro’s intake visits and check-ins collect the information that providers use for treatment decisions, as well as the details that payers require to approve coverage. With this information, our external pharmacy partner submits comprehensive prior authorization requests that help optimize patients’ chances for coverage.
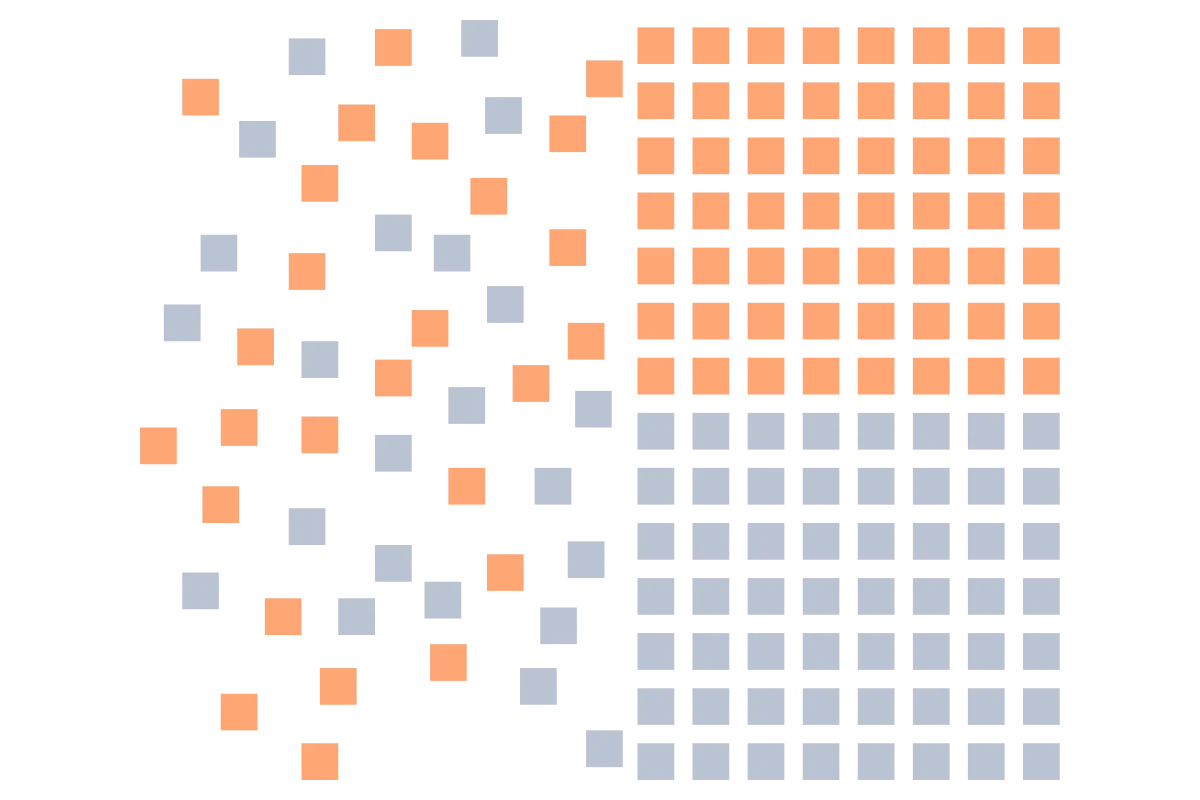
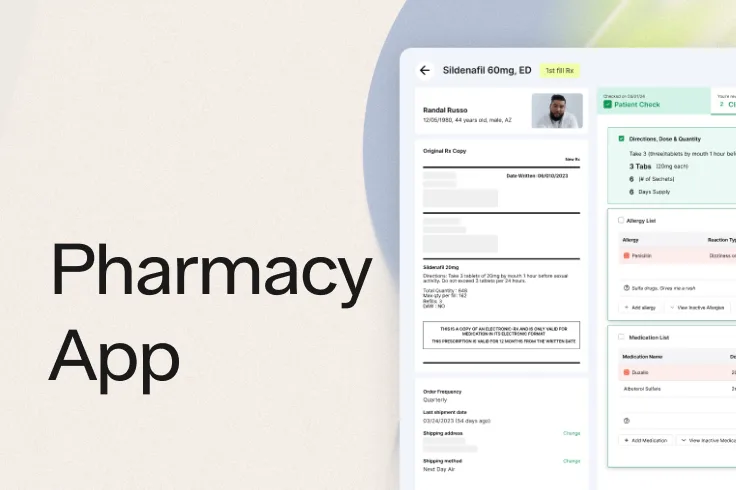
Scaled coverage insights
Ro analyzes insurance coverage trends and prior authorization results at scale to continually improve our processes. The result is better tools to help patients and providers understand benefits and increase the likelihood of getting treatment covered.