Key takeaways
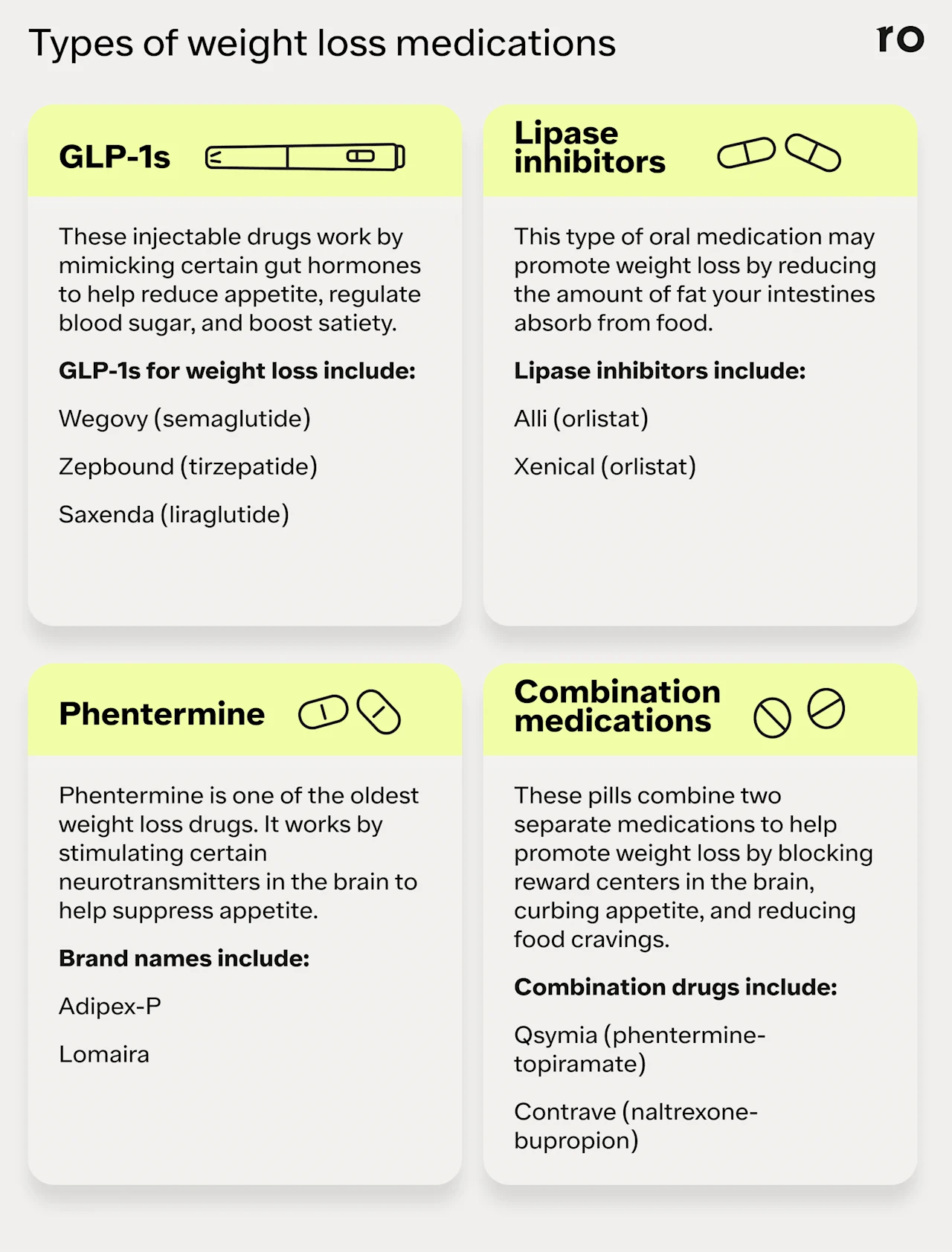
GLP-1 agonists like Wegovy and Zepbound, lipase inhibitors such as Xenical and Alli, phentermine, and combination medications like Qsymia and Contrave are medications that may help aid in weight loss.
Each of these medicines can help promote weight loss via a different mechanism, and each has its own set of side effects and risks.
Regular monitoring while on a weight loss drug is important to check for side effects, assess effectiveness, and make changes to the medication or dose, if needed.
To maximize effectiveness, work with a knowledgeable healthcare provider and pair weight loss medications with lifestyle changes such as diet and exercise.
Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
Key takeaways
GLP-1 agonists like Wegovy and Zepbound, lipase inhibitors such as Xenical and Alli, phentermine, and combination medications like Qsymia and Contrave are medications that may help aid in weight loss.
Each of these medicines can help promote weight loss via a different mechanism, and each has its own set of side effects and risks.
Regular monitoring while on a weight loss drug is important to check for side effects, assess effectiveness, and make changes to the medication or dose, if needed.
To maximize effectiveness, work with a knowledgeable healthcare provider and pair weight loss medications with lifestyle changes such as diet and exercise.
Weight loss medications like glucagon-like peptide-1 receptor agonists, or GLP-1s—which include Wegovy, Zepbound, and Saxenda — have gotten a lot of attention recently for their ability to help people lose significant amounts of weight and keep it off.
But the GLP-1 drugs are far from the only weight loss medications available.
Healthcare providers can choose from a wide range of weight loss pills and injections, both old and new, to prescribe for their patients. That may include injectable GLP-1s and oral weight loss medications such as:
Phentermine (Adipex, Lomaira)
Phentermine-topiramate (Qsymia)
Naltrexone-bupropion (Contrave)
Other short-term drugs, such as benzphetamine (Didrex) and diethylpropion (Tenuate), are approved for weight loss but are rarely used due to potential risks like dependence or exacerbating existing cardiovascular health issues.
While these medications can be helpful tools for weight management, it's important to have realistic expectations going into the process if your provider prescribes one of them for you. Understand that any medication you take has both benefits and risks, and there's no quick fix for losing weight.
"Obesity is a chronic, complex disease influenced by genetic, metabolic, and environmental factors," explains Andres Acosta, MD, PhD, associate professor of medicine at Mayo Clinic and co-founder of Phenomix Sciences.
"Without addressing the underlying causes — whether through lifestyle changes, behavioral interventions, or personalized treatment — weight loss may not be sustainable,” he adds. “These medications work best when combined with long-term, individualized strategies."
If you've been contemplating weight loss drugs, this guide is a good place to start. In this article, we'll walk you through the different types of weight loss medications, how they work, their benefits and risks, and how they fit into an overall weight reduction strategy.
GLP-1 receptor agonists
This group of medicines is used to treat type 2 diabetes and overweight/obesity. In recent years, these medications have also been approved by the US Food and Drug Administration (FDA) to help protect heart health, reduce the risk for chronic kidney disease, and treat conditions like obstructive sleep apnea.
FDA-approved GLP-1 receptor agonists for weight loss include:
Wegovy pill (semaglutide) is a daily oral tablet you take in the morning on an empty stomach, at least 30 minutes before any food, water, or other medications. It’s available in four dosage strengths: 1.5 mg, 4 mg, 9 mg, and 25 mg. Oral Wegovy is FDA-approved for weight loss in adults with obesity or overweight and one weight-related medical condition. It’s also approved to reduce cardiovascular risk in adults with heart disease and either obesity or overweight.
Wegovy is also available as a weekly injection you take on the same day each week. It comes in a single-dose pen that you inject into the skin of the thigh, stomach, or upper arm. Wegovy comes in five dose strengths: 0.25 mg, 0.5 mg, 1 mg, 1.7 mg, and 2 mg. It's FDA-approved for weight loss in adults and children aged 12 and older with obesity and adults with overweight and at least one weight-related medical condition. Wegovy injection is also approved for fatty liver disease and to lower cardiovascular risk in adults with obesity or overweight and heart disease.
Zepbound (tirzepatide)is also a weekly injection. It comes in single-dose pens or single-use vials that you inject with a needle and syringe. Zepbound dose strengths include 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg. Zepbound is only approved for weight loss in adults, though it’s also indicated to treat obstructive sleep apnea (OSA) in adults with obesity.
Saxenda (liraglutide) is also an injectable drug, but unlike other GLP-1s for weight loss, Saxenda is taken daily. It comes in a multi-dose pen, so each time you take it, you select your dose and attach a new needle. Saxenda comes in five dose strengths: 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg, and 3 mg. It's approved for adults with obesity or overweight and children ages 12 and older with obesity.
How they work
GLP-1 receptor agonists can help control blood sugar and promote weight loss by mimicking a natural hormone called glucagon-like peptide 1 that your body makes. This gut hormone helps to promote weight loss in a few ways:
Regulating blood sugar
Slowing stomach emptying, which can help you stay full after you eat
Reducing hunger cues and “food noise” in the brain, which may lead to consuming fewer calories
Tirzepatide is a dual GLP-1 and GIP receptor agonist. It mimics two hormones — GLP-1 and GIP — that can aid in blood sugar control and weight management. This dual-action mechanism may make tirzepatide more effective for weight loss than other similar medications, though more research is needed.
With each medication, your healthcare provider will likely start you at the lowest dose. From there, they may gradually increase your dose over time (depending on how well you tolerate the medication) until you reach a maintenance dose for weight loss.
Cost and insurance
The cost of weight loss injections can vary depending on insurance coverage, eligibility for savings programs, coupons, and other discounts.
In general, GLP-1s can cost around $1,000 per month without insurance coverage. The high cost of some weight-loss medications can make them unaffordable.
Health insurance may not cover the cost of weight loss medications, but you have the right to appeal the decision if your insurer denies coverage. You can also look for manufacturer copay cards and patient prescription programs that make these drugs more affordable.
Wegovy pill has a cash price of $149–$299 depending on dose through Ro and a list price of $1,349.02.
Wegovy. The monthly cost for Wegovy is about $1,349.02 before insurance or other savings programs. People paying cash for their prescription may also access Wegovy for $199 per month for the first two months, then $349 per month thereafter. (FYI, the $199 per month offer is only available through March 31, 2026, and for 0.25 mg and 0.5 mg doses.)
Zepbound. The list price for Zepbound can vary. Zepbound pens are about $1,086.37 per month before insurance, discounts, or other savings. For people with commercial insurance that doesn’t cover weight loss medication, Eli Lilly offers Zepbound pens for $650 per month. Zepbound vials are also available through Ro. The cost for Zepbound vials is $299–$449 per month, depending on the dose.
Saxenda. The list price of Saxenda is $1,349.02 per month before insurance or other savings programs. Since Saxenda comes in a multi-use pen, you’ll also need to pay for a 30-day supply of disposable needles, which can cost around $60 or more each month.
Weight loss results
In a 2022 review of 22 studies that included more than 17,000 people with or without type 2 diabetes:
More than 50% of participants treated with either semaglutide or liraglutide lost 5% or more of their starting weight after an average of 26 weeks on the medicine
About 17% of participants lost 10% or more of their body weight in the same period
Another phase 3 clinical trial studied treatment with tirzepatide in people with obesity and found that it produced “substantial and sustained” weight loss at various dose strengths. After 72 weeks:
Participants taking 5 mg of tirzepatide lost an average of 10% of their body weight
Participants taking 10 mg and 15 mg weekly doses lost 15%-20%, respectively
Side effects and risks of GLP-1s
The most common side effects from these medicines are mild gastrointestinal (GI) issues, such as:
Vomiting
Diarrhea
Abdominal pain
Rare but serious side effects of GLP-1s may include:
Pancreatitis, or inflammation of the pancreas
Gallbladder disease (including gallstones or gallbladder inflammation)
Low blood sugar (hypoglycemia) in people who also take insulin for diabetes
Severe allergic reactions
Kidney damage in people who have kidney issues
Diabetic retinopathy complications in people with this eye disease
These medicines also carry a black box warning because they increased the risk for thyroid C-cell tumors in studies of rats. Although there's no evidence that GLP-1 medications cause the same effects in humans, they aren't recommended for people with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome 2 (MEN 2).
Lipase inhibitors
Lipase inhibitors are a group of medications that disrupt certain enzymes in the intestines. Orlistat is currently the only FDA-approved lipase inhibitor for weight loss.
Orlistat is the active ingredient in two brand-name drugs for weight loss:
Xenical comes in a 120 mg pill that you take three times a day with each main meal containing fat (either during or up to one hour after the meal). It was first approved for weight loss in 1999 and is only available by prescription. Xenical is indicated for weight loss and weight management in adults and was recently approved for obesity management in children aged 12 and older.
Alli is a lower-dose version of Xenical that you can get over the counter (OTC). It comes in a 60 mg capsule that you take with each meal containing fat, up to (but not more than) three pills per day. Alli is only approved for use in adults aged 18 and older.
How they work
Alli and Xenical work to promote weight loss by blocking an enzyme called lipase. Lipase helps break down fat from food and reduces the amount of fat your intestines absorb.
When used at the highest dosage (120 mg), orlistat can reduce the amount of fat your body absorbs by about 30%. That dietary fat is then removed as waste in your bowel movements.
Cost and insurance
Orlistat medications tend to be less expensive than GLP-1s, but the price can vary depending on the medication.
Alli costs about $55 for 90 capsules, or about a one-month supply.
Xenical can cost more than $600 for 90 capsules without insurance, though discounts, coupons, or opting for generic orlistat may help lower the cost.
Weight loss results
In a review of six studies that lasted 1-2 years, participants who took 120 mg of orlistat (the dosage of Xenical) three times a day lost between 6.5% and 10.2% of their initial weight. Participants in these studies also received advice on diet and behavioral changes.
A smaller study looked at weight loss treatment with 60 mg of orlistat, which is the dosage of Alli. After 24 weeks (about five months), people taking orlistat lost roughly 13 pounds and also reduced visceral abdominal fat — a type of belly fat that accumulates deep within the abdomen and around vital organs — by nearly 16% compared to the placebo group.
Side effects and risks of lipase inhibitors
The most common side effects of orlistat are gastrointestinal, including:
Loose, greasy stools
Diarrhea
Gas (flatulence)
Leakage of feces (poop) onto underwear or clothes
Abdominal pain
Tears in the anus
Because orlistat works by blocking fat absorption and removing excess fat as waste, these side effects may be more common after eating high-fat foods or meals. Following a low-fat diet may help reduce or minimize these side effects.
In rare cases, orlistat has been linked to liver damage. The drug might increase the risk of osteoporosis by preventing absorption of the bone-strengthening nutrients calcium and vitamin D. Animal studies found an increased risk for colorectal cancer, although that risk hasn't been shown in humans.
Phentermine and combination medications
Phentermine is the oldest of the prescription weight loss drugs. It was approved in 1959 as a short-term treatment for obesity, but its use has since been expanded to long-term weight management.
Today, phentermine is prescribed on its own or in combination with the anti-seizure drug topiramate.
Naltrexone-bupropion is another combination anti-obesity medicine. It combines an opioid blocker (naltrexone) with an antidepressant (bupropion).
These medications are available under several brand names:
Adipex-P and Lomaira (phentermine). Adipex-P comes in a 37.5 mg oral capsule or tablet that you take daily with breakfast. Lomaira comes in an 8 mg oral capsule that you take three times per day with food. Both medications are approved for adults with obesity or overweight and are not indicated for use in children.
Qsymia (phentermine-topiramate) comes in 3.75 mg, 7.5 mg, 11.25 mg, or 15 mg extended-release oral capsules that you take once daily. The recommended dosing schedule starts at the lowest dose strength for 1-2 weeks before moving to 7.5 mg for the next few months. From there, your healthcare provider may move you to higher dose strengths to help maximize weight loss. Qsymia is approved for adults and children aged 12 and older with obesity or adults with overweight and a weight-related health condition.
Contrave (naltrexone-bupropion) comes in an 8 mg tablet you take daily. The recommended dosing schedule is one tablet each morning for the first week before gradually increasing to a maximum dosage of four tablets per day (two in the morning and two at night). Contrave is only approved for use in adults with obesity or overweight.
How they work
Phentermine medications like Adipex-P and Qsymia work by stimulating certain neurotransmitters in the brain to help suppress appetite, reduce food cravings, and help you feel full more quickly.
Contrave works by blocking reward centers in the brain, which helps to curb appetite and cravings.
Cost and insurance
The cost of phentermine and combination medications can vary. But they tend to be more affordable than other weight loss drugs, both with and without insurance.
Adipex-P can cost $100 or more per month, but coupons or buying generic phentermine can significantly reduce the monthly cost.
Lomaira costs about $25-$45 each month before coupons or discounts.
Qsymia costs $98 without insurance for a 30-day supply. The average retail price with insurance is $80 for a 30-day supply.
Contrave may cost $99 or less per month, regardless of your insurance coverage, through the manufacturer’s CurAccess Patient Support Program.
Weight loss results
Combination medicines do have the potential to produce weight loss, although not as much as newer GLP-1 drugs.
A review of obesity medications published in JAMA included both of these combination medicines.
Qsymia was associated with 8% more weight loss than placebo in five randomized controlled trials that included 3,407 participants.
Contrave led to a 4.1% greater weight loss than placebo in six randomized controlled trials with 9,949 participants.
Another review found that people taking 15 mg of Qsymia lost roughly 10% of their body weight over 56 weeks (just over one year), and the weight loss helped improve certain risk factors for heart disease and type 2 diabetes.
Side effects and risks of phentermine and combination medications
Common side effects of Qsymia can include:
Prickling, numbness, and tingling sensations in the skin
Constipation
Dry mouth
Increased heart rate
Dizziness
Metallic, bitter, or other unpleasant taste
Insomnia
Rare but serious side effects of Qsymia may include:
Sudden onset of suicidal thoughts or behaviors
Nearsightedness
Closed-angle glaucoma, a rare condition in which fluid builds up and creates pressure in the eye
Mood changes
Problems with attention, memory, speech, or language
Too much acid in body fluids, called metabolic acidosis
Reduced kidney function
Rash
The most common side effects with Contrave include:
Nausea or vomiting
Constipation
Headache
Dizziness
Insomnia
Dry mouth
Diarrhea
Less common side effects of Contrave may include:
Mood changes, including depression, mania, hallucinations, anxiety, panic, and agitation
High blood pressure and heart rate
Seizures
Liver damage
Closed-angle glaucoma
Low blood sugar in people who also take diabetes medicines
Contrave carries a black box warning about an increased risk of suicidal thoughts and behaviors in children, teens, and young adults taking antidepressants for depression and other psychiatric conditions. People taking Contrave should be regularly monitored for new or worsening suicidal thoughts or behaviors.
Emerging weight loss medications
Researchers are currently studying new and potentially more effective anti-obesity medications. Some of the medicines coming down the pipeline include:
Orforglipron, a new oral GLP-1 drug that could be used for treating obesity and type 2 diabetes
Survodutide, mazdutide, and pemvidutide, weekly injectable drugs that work on both GLP-1 and glucagon receptors to help reduce weight and lower blood sugar
Retatrutide, a triple agonist targeting GLP-1, GIP, and glucagon that comes in a once-weekly injection
Pramlintide and cagrilintide, injectable drugs that work by acting on receptors for amylin, a hormone produced by the pancreas that plays a role in blood sugar control and satiety (fullness)
Bimagrumab, an experimental drug that may help increase lean muscle mass while reducing body fat
How long will I take weight loss medications?
The length of treatment varies based on your goals, response to treatment, and what lifestyle changes you implement along with the medication.
According to Raj Singh, MD, FACP, FASN, an internal medicine specialist, nephrologist, and obesity medicine specialist at Healor Health, people taking GLP-1s should expect to stay on them long-term — or even indefinitely.
"These drugs aren't cures and don't change the underlying factors that cause weight gain," he stresses. "If you stop taking them without making lasting lifestyle changes, there's a good chance the weight will return."
You should have regular follow-up visits with your healthcare provider while on weight loss medication. Your provider can monitor you for side effects and adjust the medicine dosage if necessary.
Since some of these medicines can affect certain organs, routine lab tests of your liver, kidney, and thyroid function are recommended, Dr. Singh adds.
At these visits, your healthcare provider can also evaluate how your weight loss is progressing. "Adjustments, such as dosage changes or switching treatments, may be needed if a patient isn't responding well," Dr. Acosta says.
If you need to stop taking a GLP-1 medication — whether due to cost, availability, or side effects — gradually tapering off the medication may help minimize rebound hunger and weight regain. Work with your provider to find a different weight-loss drug or make lifestyle changes to maintain weight loss.
Factors such as not achieving your goal weight loss, having side effects you can't tolerate, or experiencing rare but serious medication reactions are reasons to stop taking the medicine.
The importance of lifestyle changes with weight loss medication
Weight loss medications can be effective tools, but they aren’t meant to work in isolation. In most clinical trials, participants who lost the most weight combined medication with changes to diet and regular exercise.
"Medications can help with weight loss, but they don't replace the need for long-term behavior changes," Dr. Acosta says.
Adopting these lifestyle changes may help you achieve your weight loss goals while on weight loss medication, help you maintain your weight loss if you decide to stop treatment, and help to improve your overall health.
Diet and nutrition. Eat a well-balanced diet with a mix of fruits and vegetables, whole grains, and lean protein. You may also want to reduce portion sizes and limit fat, sugar, and processed foods to cut calories.
Physical activity. Regular exercise can help support your weight loss goals and improve heart health, blood sugar control, and other measures of health. A combination of cardio and strength training can help build muscle and burn calories. Aim for 150 minutes of exercise each week with aerobic exercises like walking or bike riding, and add in strength training moves with weights, exercise bands, or your body weight for resistance.
Sleep and stress management. Chronic or uncontrolled stress may cause weight gain through the release of hormones like cortisol and by changing eating habits and fat storage. To help manage stress, practice relaxation techniques like deep breathing or meditation, and help your body recover and repair with at least 7–9 hours of sleep a night.
Who can take weight loss medications?
Ultimately, your healthcare provider will help determine if you are a good candidate for weight loss medications based on things like your age, weight, personal and family health history, any underlying conditions, and more.
In general, weight loss medications are recommended for people who:
Have a body mass index (BMI) of 30 or higher
Have a BMI of 27 or higher, plus a weight-related condition like high blood pressure or type 2 diabetes
Find out how much you could lose
Provide your biometric data to get started.

0.0
Your BMI
Underweight
< 18.5
Healthy weight
18.5 - 24.9
Overweight
24.9 - 29.9
Obesity
> 30
Who should not take weight loss medications?
While FDA-approved weight loss injections and pills have undergone extensive testing and are generally considered safe, they may not be appropriate for everyone.
You may need to avoid weight loss medications if you:
Have a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome type 2 (MEN2)
Have a personal or family history of pancreatitis or gallbladder disease
Are allergic to any of the ingredients in the medication
Are pregnant or breastfeeding
Have a history of eating disorders, substance abuse, addiction, or certain mental health conditions
If you’re interested in weight loss medications, talk to your healthcare provider. Be sure to tell them about your overall health history, as well as any medications or supplements you’re currently taking. They can do a thorough evaluation to help determine if weight loss medicine is a good option for you.
Alternatives to prescription weight loss medications
The only OTC medicine currently FDA-approved for weight loss is Alli.
Natural supplements like caffeine, bitter orange, berberine, and chitosan are often promoted for weight loss. But the research supporting these and other natural weight-loss alternatives is limited.
"They often lack strong, consistent evidence for safe and effective weight loss, and their regulation can be less strict than prescription medications," Dr. Singh says.
Non-medication alternatives
In addition to medication, behavior modification programs may help you lose weight. These may include cognitive behavioral therapy, dietary assessments, and counseling to give you the advice and encouragement you need to get to your goal weight.
For people with a condition called extreme obesity (a BMI of 40+) or obesity plus a weight-related condition like type 2 diabetes or high blood pressure, bariatric surgery may be an option.
This procedure reduces the size of the stomach so that a person can't eat as much food and absorbs less fat and calories from the food they do eat. Surgery can come with risks like bleeding, infection, and blood clots, and it isn't for everyone.
What's the most effective weight loss medication?
GLP-1 receptor agonists like Wegovy and Saxenda and dual GLP-1/GIP drugs like Zepbound have produced some of the most impressive weight-loss results, Dr. Singh says.
In head-to-head studies, Zepbound was shown to produce the most significant weight loss, helping people to lose 20% or more of their body weight.
But in reality, the rate of weight loss varies from person to person. Losing weight is a very individualized process — the "best" medication for you depends on several factors.
"For example, GLP-1s can be a good match for patients who require both blood glucose management and obesity treatment," Dr. Singh says.
Other medications like Xenical, which reduces the absorption of fat, may be a good fit for people who are looking to reduce their calorie intake or who might not tolerate the GLP-1 drugs.
"Contrave could be an option for patients who struggle with cravings and emotional eating, especially if there's a mood component," he adds.
Your healthcare provider can help identify the right medication for you based on factors such as cost, side effects, risks, and your personal health history and weight loss goals. If one medication isn't effective or causes side effects, your provider may recommend switching to another drug or adjusting your treatment plan.
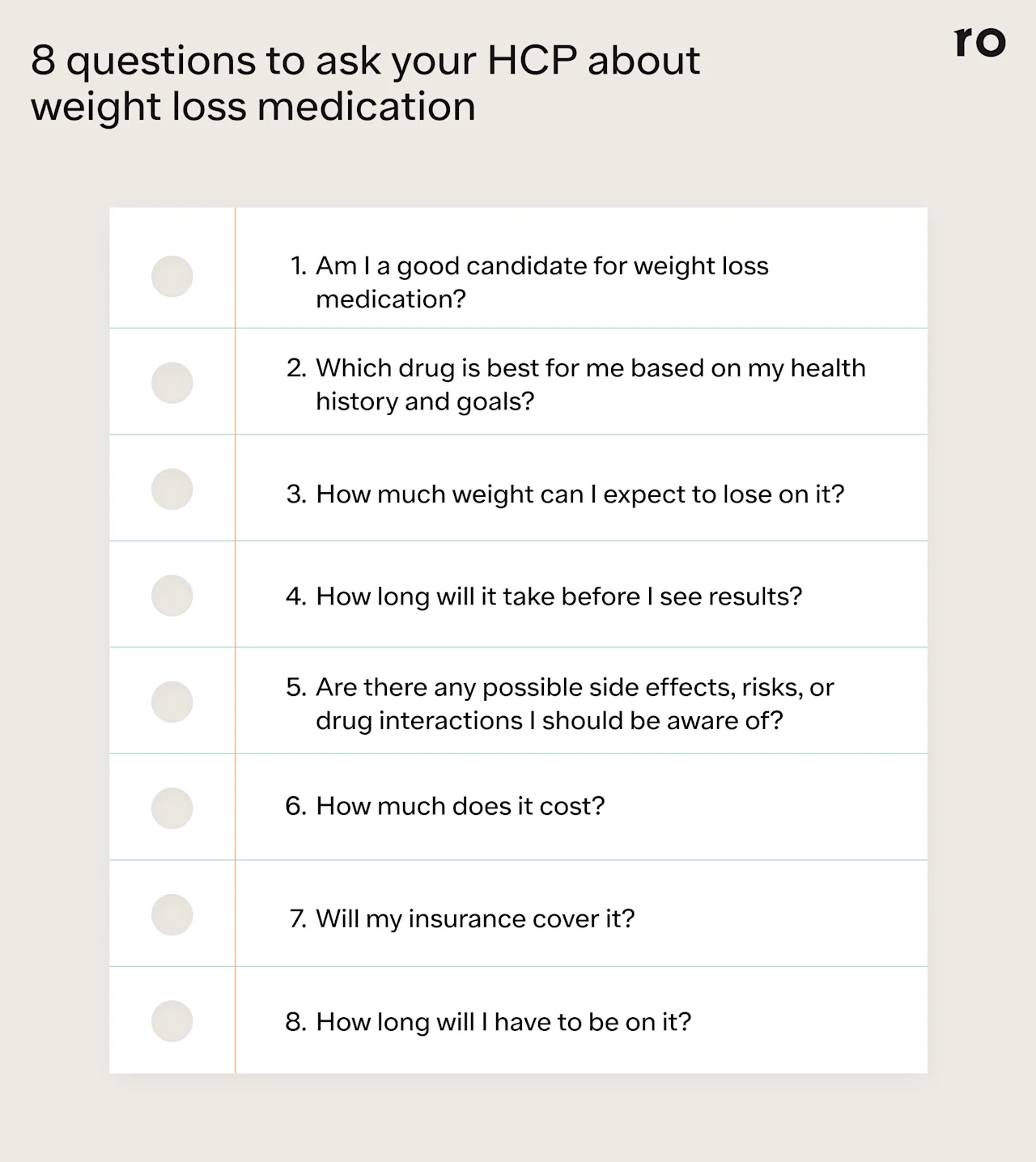
Questions for your healthcare provider about weight loss medications
Here are some questions to ask your healthcare provider if you're interested in trying a weight loss medication:
Am I a good candidate for weight loss medication?
Which drug would be best for me?
How much weight can I expect to lose on it?
How long will it take before I see results?
What are the possible side effects and risks?
How often will you monitor me while I'm taking the weight loss drug?
How much does it cost, and will insurance cover my medication?
How long will I need to stay on the medicine?
Bottom line
There are multiple weight loss medications on the market, from injectable drugs to oral pills and OTC options. But these drugs aren't one-size-fits-all. It's important to work with a knowledgeable healthcare provider who can help you choose the medication that best fits your health needs and weight loss goals.
Several classes of weight loss medications are available. GLP-1 agonists and dual GLP-1/GIP agonists are the newest ones, but older drug classes like lipase inhibitors, phentermine, and combination medications may be appropriate in certain circumstances. These drugs can vary in terms of cost and effectiveness and may come with side effects.
Some weight loss medications may be more effective than others. Most of these drugs may help you lose up to 5% of your body weight when combined with diet and exercise, but Zepbound may produce the most weight loss of the medications on this list, according to clinical trial data.
Weight-loss medication isn't a quick fix. You may need to stay on these drugs long-term, or even indefinitely, and pair them with lifestyle changes like diet and exercise to achieve more significant and sustainable weight loss.
Regular monitoring is key. You'll likely see your healthcare provider for regular check-ups to make sure the drug is working, monitor for possible side effects, and make dosing adjustments as needed.
Frequently asked questions (FAQs)
What is the best drug for weight loss?
The best drug for weight loss is the one that works for you, fits within your budget, and has minimal side effects, Dr. Acosta says.
According to clinical trial data, Zepbound may produce the most weight loss over time, helping people to lose 20% or more of their body weight.
What is the most commonly prescribed weight loss medication?
Phentermine is the most widely used and oldest weight loss medication, according to the Obesity Medicine Association. This may be because phentermine has been on the market longer and is generally less expensive than newer weight loss drugs.
How to lose 50 pounds in 3 months?
Losing 50 pounds in three months isn't advised. "Medically speaking, rapid weight loss is not recommended as it can lead to many negative side effects such as electrolyte issues, gastrointestinal problems, formation of gallstones, and more," Dr. Singh says.
He adds that a safer goal is to lose 1-2 pounds a week or 4-8 pounds per month. This could lead to a weight loss of about 12-24 pounds in three months.
What is the new weight loss drug better than Ozempic?
Ozempic (semaglutide)is a GLP-1 medication for diabetes. While it may promote some weight loss, it’s not FDA-approved for that purpose. Wegovy is the brand-name version of semaglutide approved for weight loss. It comes in two forms: a daily oral pill or a weekly injection.
According to some research, tirzepatide (Zepbound) produces more weight loss than semaglutide (Wegovy). In one study comparing tirzepatide vs. semaglutide for weight loss, people on tirzepatide lost an average of 15.3% of their body weight after 12 months, compared to an 8.3% weight loss on semaglutide.
Which weight loss tablet is best?
There is no one "best" weight loss pill. The best weight loss medicine is the one that works for you and your unique health needs, goals, and budget.
What drug is used for rapid weight loss?
Most experts recommend a slower, sustained weight loss of 1-2 pounds per month instead of rapid weight loss. In addition to diet and exercise, medications may help kickstart the process, but results and timelines are different for each person.
Phentermine may produce weight loss after three months. People taking orlistat may notice weight loss within two weeks, but it can take up to two months or longer to see more significant reductions in weight. GLP-1 receptor agonists and dual GIP/GLP-1 drugs start working right away, but it can take several weeks to see weight loss results as your body adjusts to the medication.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
Zepbound Important Safety Information: Read more about serious warnings and safety info.
Saxenda Important Safety Information: Read more about serious warnings and safety info.
GLP-1 Important Safety Information: Read more about serious warnings and safety info.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
References
Alfaris, N., Minnick, A. M., Hopkins, C. M., et al. (2015). Combination phentermine and topiramate extended release in the management of obesity. Expert Opinion On Pharmacotherapy, 16(8), 1263–1274. doi: 10.1517/14656566.2015.1041505. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25958964/
Bansal, A. G., Patel, P., & Khalili, Y. A. (2024). Orlistat. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542202/
Baxter, S. M., Lund, L. C., Andersen, J., et al. (2025). Glucagon-Like Peptide 1 Receptor Agonists and Risk of Thyroid Cancer: An International Multisite Cohort Study. Thyroid: Official Journal of the American Thyroid Association, 35(1), 69–78. doi: 10.1089/thy.2024.0387. Retrieved from https://pubmed.ncbi.nlm.nih.gov/39772758/
Chauhan, S. S., Arnold, K., Mackenzie, C., et al. (2011). The Influence of Orlistat (Xenical) on Weight Loss in Overweight and Obese Adults: A Systematic Review. (2011). Proceedings of the Nutrition Society. doi: 10.1017/S0029665111000346. Retrieved from https://www.cambridge.org/core/journals/proceedings-of-the-nutrition-society/article/influence-of-orlistat-xenical-on-weight-loss-in-overweight-and-obese-adults-a-systematic-review/BBC3B5700794B184355B9276FCB16496
Currax Pharmaceuticals-a. (n.d.). Contrave dosing. Retrieved from https://contravehcp.com/dosing/
Currax Pharmaceuticals-b. (n.d.). Save on Contrave. Retrieved from https://contrave.com/save/
Eli Lilly and Company-a. (2025). How much should I expect to pay for Zepbound? Retrieved from https://pricinginfo.lilly.com/zepbound
Eli Lilly and Company-b. (2025). Savings options for Zepbound - regardless of insurance status. Retrieved from https://zepbound.lilly.com/coverage-savings
GoodRx-a. (n.d.). Adipex-P. Retrieved from https://www.goodrx.com/adipex-p?label_override=adipex-p
GoodRx-b. (n.d.). Alli. Retrieved from https://www.goodrx.com/alli
GoodRx-c. (n.d.). Lomaira. Retrieved from https://www.goodrx.com/lomaira
GoodRx-d. (n.d.). Novofine. Retrieved from https://www.goodrx.com/novofine
GoodRx-e. (n.d.). Xenical. Retrieved from https://www.goodrx.com/xenical?label_override=xenical
Gudzune, K. A. & Kushner, R. F. (2024). Medications for Obesity: A Review. JAMA, 332(7), 571-584. doi: 10.1001/jama.2024.10816. Retrieved from https://jamanetwork.com/journals/jama/article-abstract/2821290
Heshmati, H. H., Luz, L., Greenway, F. L., et al. (2023). Editorial: Stress-Related Weight Changes. Frontiers in Endocrinology, 14, 1209975. doi: 10.3389/fendo.2023.1209975. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10241186/
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., et al. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. The New England Journal of Medicine, 387(3), 205–216. doi: 10.1056/NEJMoa2206038. Retrieved from https://www.nejm.org/doi/10.1056/NEJMoa2206038
Jensen, S. B. K., Blond, M. B., Sandsal, R. M., et al. (2024). Healthy Weight Loss Maintenance with Exercise, GLP-1 Receptor Agonist, or Both Combined Followed by a Year without Treatment: A Post-Treatment Analysis of a Randomised Placebo-Controlled Trial. eClinicalMedicine, 69. doi: 10.1016/j.eclinm.2024.102475 Retrieved from https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(24)00054-3/fulltext
Johnson, D. B. & Quick, J. (2023). Topiramate and Phentermine. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482165/
KVK-Tech. (n.d.). FAQ - Lomaira. Retrieved from https://lomaira.com/faqs/
KVK-Tech. (2016). Highlights of Prescribing Information for Lomaira. Retrieved from https://lomaira.com/Prescribing_Information.pdf
Lewis, K. H., Fischer, H., Ard, J., et al. (2019). Safety and Effectiveness of Longer-Term Phentermine Use: Clinical Outcomes from an Electronic Health Record Cohort. Obesity (Silver Spring, Md.), 27(4), 591–602. doi: 10.1002/oby.22430. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30900410/
Melson, E., Ashraf, U., Papamargaritis, D., et al. (2024). What is the Pipeline for Future Medications for Obesity? International Journal of Obesity. https://doi.org/10.1038/s41366-024-01473-y. Retrieved from https://www.nature.com/articles/s41366-024-01473-y
National Association of Insurance Commissioners. (2024). Does Insurance Cover Prescription Weight Loss Injectables? Retrieved from https://content.naic.org/article/does-insurance-cover-prescription-weight-loss-injectables
National Institutes of Health Office of Dietary Supplements. (2022). Dietary Supplements for Weight Loss. Retrieved from https://ods.od.nih.gov/factsheets/WeightLoss-HealthProfessional/
Novocare. (2026). Start saving on Wegovy. Retrieved from https://www.novocare.com/patient/medicines/wegovy.html
NovoNordisk-a. (2025). NovoCare Pharmacy. Retrieved from https://www.novocare.com/obesity/products/wegovy/get-product.html
NovoNordisk-b. (2025). What is the list price of Wegovy and will it impact me? Retrieved from https://www.novocare.com/obesity/products/wegovy/let-us-help/explaining-list-price.html
Obesity Medicine Association. (2024). Top Weight Loss Medications. Retrieved from https://obesitymedicine.org/blog/weight-loss-medications/
Rodriguez, P. J., Goodwin Cartwright, B. M., Gratzl, S., et al. (2024). Semaglutide vs. Tirzepatide for Weight Loss in Adults with Overweight or Obesity. JAMA Internal Medicine, 184(9), 1056-1064. doi: 10.1001/jamainternmed.2024.2525. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2821080
Smith, S. R., Stenlof, K. S., Greenway, F. L., et al. (2011). Orlistat 60 mg reduces visceral adipose tissue: a 24-week randomized, placebo-controlled, multicenter trial. Obesity (Silver Spring, Md.), 19(9), 1796–1803. doi: 10.1038/oby.2011.143. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21720429/
Taylor & Francis. (n.d.). Benzphetamine - Knowledge and References. Retrieved from https://taylorandfrancis.com/knowledge/Medicine_and_healthcare/Pharmaceutical_medicine/Benzphetamine/
Tomiyama, A. J. (2019). Stress and Obesity. Annual Review of Psychology, 70, 703–718. doi: 10.1146/annurev-psych-010418-102936. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29927688/
U.S. Food and Drug Administration (FDA). (2012). Highlights of Prescribing Information for Adipex-P. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/085128s065lbl.pdf
U.S. Food and Drug Administration (FDA). (2017). Alli Starter Pack Label. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021887Orig1s009lbl.pdf
U.S. Food and Drug Administration (FDA-a). (2025). Highlights of Prescribing Information: Contrave (naltrexone- hydrochloride and bupropion hydrochloride) extended-release tablets, for oral use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/200063s024s026lbl.pdf
U.S. Food and Drug Administration (FDA). (2024). Highlights of Prescribing Information: Qsymia (phentermine and topiramate extended-release capsules), for oral use, CIV. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/022580s026lbl.pdf
U.S. Food and Drug Administration (FDA-b). (2025). Highlights of Prescribing Information: Saxenda (liraglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/206321s022lbl.pdf
U.S. Food & Drug Administration (FDA-c). (2025). Highlights of Prescribing Information: Wegovy (semaglutide) injection, for subcutaneous use. WEGOVY (semaglutide) injection, for subcutaneous use and WEGOVY (semaglutide) tablets, for oral use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/218316Orig1s000lbl.pdf
U.S. Food and Drug Administration (FDA). (2022). Highlights of Prescribing Information for Xenical (Orlistat). Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/020766s038lbl.pdf
U.S. Food and Drug Administration (FDA). (2020). New Pediatric Labeling Information Database - Xenical. Retrieved from https://www.accessdata.fda.gov/scripts/sda/sdDetailNavigation.cfm?sd=labelingdatabase&id=14CE0322582A1B7DE053564DA8C071F2&rownum=1
Vivus, LLC-a. (n.d.). Prescribing and dosing. Retrieved from https://hcp.qsymia.com/prescribing/
Vivus, LLC-b. (n.d.). Qsymia Patient Savings. Retrieved from https://hcp.qsymia.com/patient-savings/
Vosoughi, K., Roghani, R. S., & Camilleri, M. (2022). Effects of GLP-1 Agonists on Proportion of Weight Loss in Obesity with or without Diabetes: Systematic Review and Meta-Analysis. Obesity Medicine, 35, 100456. Retrieved from https://www.sciencedirect.com/science/article/pii/S2451847622000689















