Key takeaways
The FDA has approved four prescription weight loss pills: phentermine/topiramate (brand name Qsymia), naltrexone/bupropion (brand name Contrave), orlistat (brand names Alli, Xenical), phentermine (brand names Adipex-P, Lomaira).
Of these, Qsymia is the strongest weight loss pill available.
Along with a healthy diet and exercise routine, these drugs can help you lose a modest amount of weight.
If you need to lose a larger percentage of your body weight, injectable weight loss medications (like Wegovy or Zepbound) might be better options.
Here's what we'll cover
Key takeaways
The FDA has approved four prescription weight loss pills: phentermine/topiramate (brand name Qsymia), naltrexone/bupropion (brand name Contrave), orlistat (brand names Alli, Xenical), phentermine (brand names Adipex-P, Lomaira).
Of these, Qsymia is the strongest weight loss pill available.
Along with a healthy diet and exercise routine, these drugs can help you lose a modest amount of weight.
If you need to lose a larger percentage of your body weight, injectable weight loss medications (like Wegovy or Zepbound) might be better options.
Looking for the strongest weight loss pill to help you reach your goals? While injectable medications like Wegovy and Zepbound have gained attention for their effectiveness, not everyone wants to start a weekly injection. Fortunately, there are powerful prescription weight loss pills that can offer real results—no needles required.
When combined with diet and exercise, the best weight loss pills can help you lose weight—and keep it off—by:
Suppressing your appetite (decreasing your desire to eat)
Reducing how much fat you absorb from the foods you eat
Making you feel full faster within a meal and longer in between meals
What is the best weight loss pill for you? That depends. Continue reading to learn more about the strongest weight loss pills available today.
What is the strongest prescription weight loss pill?
The most effective weight loss pill available today is a combination of two drugs, phentermine and topiramate, available under the brand name Qsymia. After taking Qsymia for about a year, people lost about 5–10% of their body weight on average, depending on the dose. The higher the dose, the more weight loss people tend to experience, though as with most drugs, potential side effects are also more common at higher doses.
How does this compare to the strongest injectable weight loss drug?
The drug that gets that title as of this writing is Zepbound (tirzepatide), which has a dual-action mechanism. It’s both a GLP-1 (aka glucagon-like peptide-1 receptor agonist) and a GIP (aka glucose-dependent insulinotropic polypeptide). Studies show people taking Zepbound for about a year and a half can lose around 15–21% of body weight on average, which is also dose-dependent.
That’s a pretty big difference! If you have a needle phobia or can’t tolerate tirzepatide for some other reason, though, 5–10% weight loss on Qsymia is nothing to sneeze at!
Let’s take a look at the other options available to you.
The strongest prescription weight loss pills
Qsymia is the strongest weight loss pill, but it’s not the only one on the market that packs a punch. Some of the strongest weight loss pills available today include:
Phentermine/topiramate (brand name Qsymia)
Naltrexone/bupropion (brand name Contrave)
Orlistat (brand names Xenical, Alli)
Phentermine (brand names Adipex-P, Lomaira)
One thing that’s worth mentioning is all of these medications require a prescription from a licensed healthcare provider—with one exception. Alli, a lower-dose version of orlistat, is sold over the counter. Another thing to know is that all antiobesity medications are most effective when combined with healthy lifestyle changes, such as improving your diet and exercise routine. Making those changes while taking prescription weight loss pills can lead to a significant amount of weight loss—between 3% and 9% (up to 10% in the case of Qsymia, as we mentioned), over the course of one year.
Keep reading to learn more about each of these drugs.
Phentermine/topiramate (brand name Qsymia)
Qsymia (phentermine/topiramate) has been available since 2012, when the FDA approved it, alongside a reduced-calorie diet and exercise, to reduce excess body weight and maintain weight loss long-term in people ages 12 and older with obesity or adults with overweight and a weight-related medical condition. Qsymia comes as an extended-release oral capsule and is usually taken once daily in the morning.
In clinical trials, 70% of people taking phentermine/topiramate lost at least 5% of their body weight within one year, compared with only 21% of those taking a placebo. One observational study of real-world practice found that people lost about 4% of their body weight within five months of starting phentermine/topiramate. After a year of treatment, another study found that people lost up to 10.6% of their body weight. A follow-up study showed that continued treatment with Qsymia helped people maintain their weight loss for up to two years. These results support Qsymia as the strongest weight loss pill available today.
Phentermine/topiramate is a combination of phentermine and the anti-seizure/anti-migraine drug topiramate; using both drugs together works better than either drug alone to reduce appetite and control binge-eating behavior. Because of phentermine’s potential for abuse, the DEA considers it a controlled substance.
You should avoid using phentermine/topiramate if you are pregnant, trying to become pregnant, have glaucoma (i.e., high pressure in the eye that can lead to vision problems), thyroid problems (hyperthyroidism), are taking a monoamine oxidase inhibitor (MAOI) medication, or are allergic to any of the ingredients in Qsymia. Some people should be extra cautious due to a greater risk of side effects, such as those who have kidney problems or a history of kidney stones, seizures, mental health problems, or liver problems.
Common side effects of Qsymia include dry mouth, constipation, paraesthesias (numbness/tingling in your hands, feet, arms, or face), trouble sleeping, changes in your sense of taste, depression, anxiety, and dizziness. Other, serious side effects are rare but possible.
Naltrexone/bupropion (brand name Contrave)
Contrave (naltrexone/bupropion) was FDA-approved in 2014 for long-term weight management, along with a reduced-calorie diet and increased physical activity, in adults with obesity or overweight with at least one weight-related health condition, such as high blood pressure. It comes as an extended-release oral tablet and is typically taken on a twice-daily schedule.
In clinical trials, roughly half of people taking naltrexone/bupropion lost at least 5% of their body weight within one year. That’s twice as many people who implemented lifestyle changes alone. One analysis of these same clinical trials reported the overall average weight loss on naltrexone/bupropion to be a little over 4% relative to placebo.
Naltrexone treats drug and alcohol dependence, while bupropion treats depression and helps people quit smoking. The combination of these two medications may affect dopamine, a brain chemical. By doing so, the combination reduces food cravings and decreases your appetite.
Common side effects of naltrexone/bupropion include nausea, headaches, constipation, insomnia, vomiting, dizziness, and dry mouth. Some people also notice elevations in blood pressure and heart rate while using naltrexone/bupropion. Since this combo medication includes bupropion, an antidepressant, it may increase the risk of suicide in young adults with depression when they first start treatment (a known side effect of antidepressants).
People with uncontrolled high blood pressure, seizure disorders, eating disorders, chronic opioid use, and those who have recently stopped taking certain medications (e.g., benzodiazepines, barbiturates, or antiseizure drugs) should avoid using this drug. Also, anyone who has used monoamine oxidase inhibitors (MAOIs) in the past 14 days should not take naltrexone/bupropion because of the risk of serious side effects and drug interactions. Since Contrave may increase blood pressure and heart rate, it may not be safe for people with a history of heart problems, heart attack, or stroke. And, like other weight loss medications, it isn’t recommended during pregnancy.
Orlistat (brand names Xenical, Alli)
Orlistat has been available since 1999. It’s FDA-approved for weight loss in people with obesity or overweight, alongside diet changes. It’s also approved to help prevent weight regain after someone has lost weight. Orlistat comes as a capsule that’s usually taken three times a day with fat-containing meals.
In one analysis, 44% of people taking orlistat lost at least 5% of their body weight within one year—nearly twice as many as those taking a placebo. Other studies have found that people taking orlistat lose at least 2% of their body weight within five months, and around 3% after one year.
Orlistat works by decreasing the absorption of fats from your food—it reduces fat absorption by up to 30%. Orlistat is available in prescription strength (brand name Xenical) and a lower strength over-the-counter formulation (brand name Alli).
Most of the side effects of orlistat affect your gastrointestinal (GI) system, including stomach rumbling, abdominal cramps, bloating, and constipation. Some of the more distressing GI effects include:
Passing gas (sometimes with oily spotting)
Diarrhea, loose stools, or greasy stools
Frequent bowel movements that are hard to control
Liver damage (rare effect)
Fortunately, most of these issues improve after using it for a while and you may avoid some of them by sticking to a low-fat diet. Other side effects include poor absorption of fat-soluble vitamins (vitamins A, D, E, and K) and kidney stones.
Phentermine (brand names Adipex-P, Lomaira)
Phentermine was one of the first appetite suppressant medications. The FDA approved it for weight loss in 1959 and, unlike the medications we’ve described so far, phentermine is only approved for short-term use. It comes as an oral tablet and an oral capsule. It’s usually taken once daily in the morning.
Even though phentermine is only approved for short-term use, some healthcare providers may prescribe it off-label for longer periods, in some cases using an intermittent schedule (for example, four weeks “on” then four weeks “off”). It’s thought that taking breaks from the medication may lower the risk of losing effectiveness over time.
People taking phentermine can lose over 7% of their body weight, or at least 8 pounds, making it another top contender for the title of strongest weight loss pill.
Phentermine is a nervous system stimulant that suppresses appetite. It’s one of the most commonly prescribed weight loss pills, but it’s only FDA-approved for weight management on a short-term basis (12 weeks). As a stimulant, phentermine is a controlled substance that has a potential risk of abuse and dependence.
People with anxiety disorders, heart disease, a history of seizures, thyroid problems, glaucoma, or uncontrolled high blood pressure should not use phentermine. In addition, you should not take phentermine if you are pregnant, breastfeeding, or have a history of substance use disorder. Phentermine also has serious drug interactions to consider. Side effects include headache, insomnia, dry mouth, dizziness, and increased heart rate and blood pressure.
Brand name(s) | Approved for long-term weight management? | Average weight loss | |
|---|---|---|---|
Naltrexone/bupropion | Contrave | Yes | 5% |
Phentermine/topiramate | Qsymia | Yes | 6.5%–8.5% |
Orlistat | Xenical, Alli | Yes | 3%–3.5% |
Phentermine | Adipex-P, Lomaira | No, only short-term use (3 months) | 7% |
Who is eligible for weight loss medications?
Most weight loss pills are meant for adults over 18 years old with the following, according to current guidelines:
Obesity with a BMI of 30 kg/m2 or more
Overweight with a BMI of 27 kg/m2 or more with at least one weight-related health problem, like high blood pressure, type 2 diabetes, or heart disease
The easiest (albeit imperfect) way to determine your weight category is to measure your Body Mass Index (BMI). BMI is a measurement of your body weight in kilograms (1 kilogram equals 2.2 pounds) divided by your height in meters squared (1 meter equals about 3 feet 3 inches). You can easily calculate your BMI by using a BMI calculator. Using your BMI, you can determine which of the following categories applies to you:
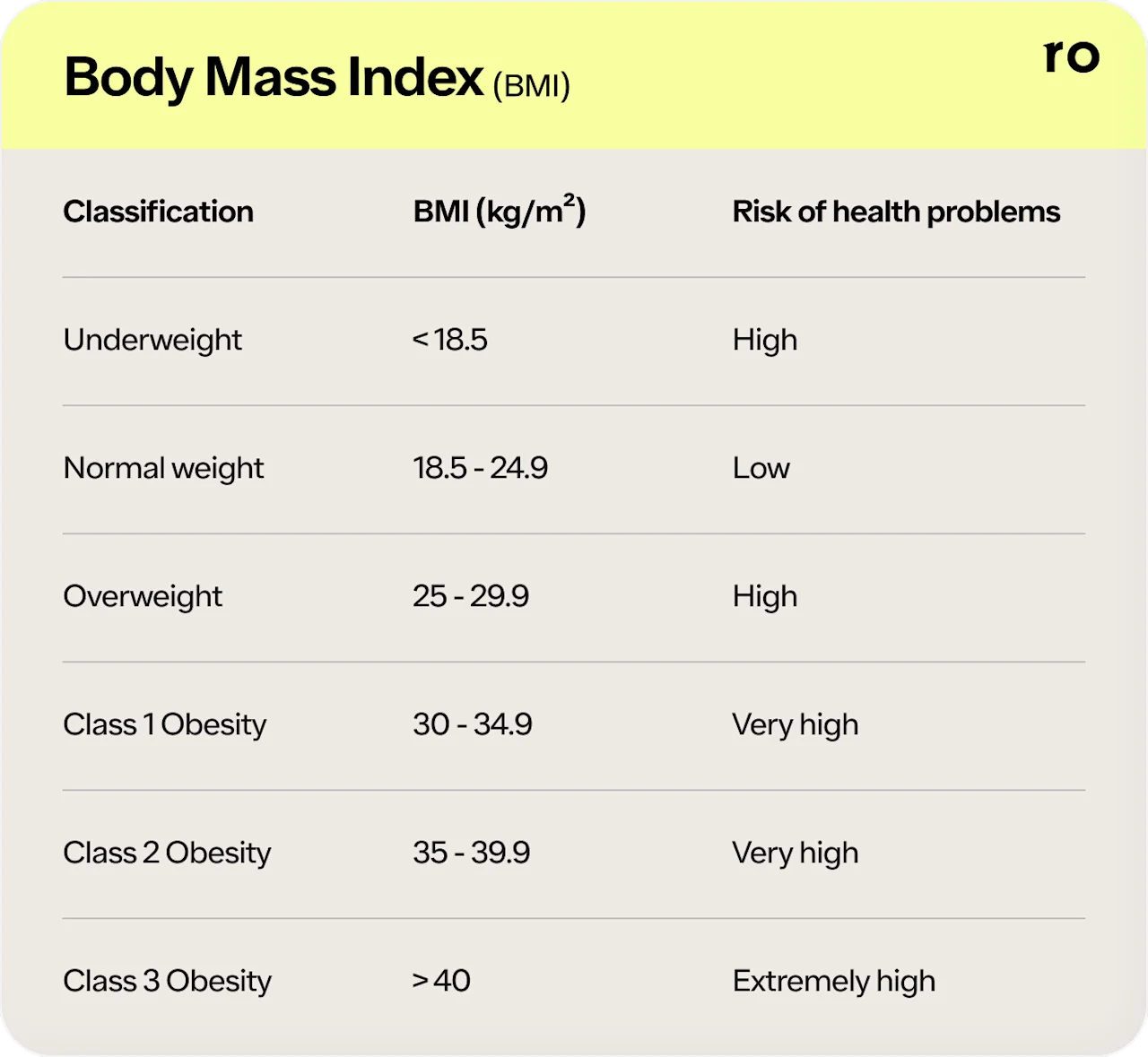
If your BMI is higher than 25, you have an increased risk of several health conditions, including heart disease, stroke, diabetes, and severe COVID-19. Losing as little as 5% of your weight can significantly improve your health. Weight loss medications, in addition to diet, exercise, and lifestyle modifications, are appropriate for some people to help with their weight loss goals.
It’s important to keep in mind that BMI does not account for factors like sex, body composition, and more. Additionally, research to support BMI as an assessment tool lacks racial and ethnic diversity.
Many weight loss pills are contraindicated for people with certain health conditions or taking specific medications. For example, people who are pregnant or breastfeeding should not take weight loss pills. Other common contraindications include uncontrolled high blood pressure and taking MAO inhibitors.
Review the prescribing information for any weight loss pill you are considering, and be sure to tell your healthcare provider about any health conditions you have, as well as any medications you are taking. Sharing this information with them can help them determine the best weight loss pill for you.
Find out how much you could lose
Provide your biometric data to get started.

0.0
Your BMI
Underweight
< 18.5
Healthy weight
18.5 - 24.9
Overweight
24.9 - 29.9
Obesity
> 30
How well do weight loss pills work?
Unfortunately, there is no magic pill to cure obesity (though treatments are becoming increasingly effective over time!). However, weight loss pills can help make your weight loss journey more successful, especially when combined with diet and exercise. The strongest weight loss pills have been tested for efficacy and safety in clinical trials.
The FDA-approved weight loss pills we’ve mentioned have different mechanisms of action, but they all mainly work by suppressing your appetite. Some do so by activating parts of your brain involved in appetite regulation—such as naltrexone/bupropion, phentermine/topiramate, and phentermine—leading to fewer cravings and less hunger. Others, such as orlistat, work by blocking how much fat you absorb from food, so you absorb fewer calories overall.
How much weight you lose on weight loss pills can depend on the medication and other lifestyle changes you make. Improving your diet and increasing your physical activity may lead to more weight loss. In general, people tend to lose between 3% and 9% of their body weight after one year of taking weight loss pills in combination with lifestyle changes.
How long do I need to take weight loss pills?
How long you need to continue taking weight loss pills depends on several factors and will vary from person to person. Depending on the side effects you experience and the rate of your weight loss, your healthcare provider may need to adjust your dosage.
If a weight loss medication works safely and effectively for you, your healthcare provider may recommend taking it long-term to help you keep the weight off. If you take your medication as prescribed and aren’t seeing results, your healthcare provider may prescribe you a different weight loss pill or an injectable weight loss medication, like semaglutide or tirzepatide.
That said, the Food and Drug Administration (FDA) has approved certain weight loss pills for short-term vs. long-term use. As we mentioned above, phentermine alone is only FDA-approved for short-term use (up to 12 weeks). For long-term weight management, the FDA has approved three weight loss pills: phentermine/topiramate (Qsymia), naltrexone/bupropion (Contrave), and orlistat (Xenical, Alli).
What to consider when choosing a weight loss pill
You might be wondering why you’d choose one weight loss pill over another if many of them achieve similar results. It’s generally going to come down to a few key factors, which your healthcare provider will go over with you:
How much weight you need to lose: If you have quite a bit to lose, Qsymia might be the best weight loss pill option for you, since it’s the strongest weight loss pill available.
Side effect tolerance: Everyone tolerates side effects differently, and you may not respond the same way to one medication as you do to another. If you try one medication and can’t tolerate the side effects, your healthcare provider may recommend trying one of the other available options.
Medical conditions or medications: If you have certain medical conditions or take specific medications, that may make you ineligible for some weight loss pills but eligible for others. For example, if you have an anxiety disorder, phentermine wouldn’t be a good option for you but Contrave might be a great fit.
Cost: While some of these medications are available as lower-cost generic drugs, cost may be a factor if your insurance doesn’t cover certain weight loss medications. See your insurance plan’s drug formulary to determine which, if any, medications are covered. To help you save, the following brand-name medications offer savings programs that may help lower the price, if you qualify:
Other medications that may help with weight loss
The drugs mentioned above are the weight loss pills that carry FDA approval. However, other drugs may be used “off-label” to help with weight loss. Off-label simply means that a drug is being used for a condition that it was not originally approved to treat.
Take metformin, for example. It is approved to treat type 2 diabetes but is used off-label to prevent prediabetes from progressing. Nowadays, metformin is also used off-label to treat other conditions, like obesity, where it can cause up to 7% weight loss.
Most antidepressants, drugs used to treat depression or anxiety, are not known for helping with shedding pounds (many have the opposite effect). There’s one exception, though. Bupropion, one of the drugs in the FDA-approved weight loss medicine Contrave, is an antidepressant that may aid weight loss, and in some cases may be recommended off-label for that purpose (generally not without another reason for prescribing it, though).
There is another option for FDA-approved weight loss medication: weight loss injections.
Weight loss injections
Injectable weight loss medications are the closest thing we currently have to a “magic” treatment for overweight and obesity. Some of them work almost as well as gastric bypass surgery!
There are two main types of weight loss injections: GLP-1s and drugs that combine GLP-1 with GIP. The FDA has approved three injectable drugs for weight loss:
Wegovy (semaglutide)—This is a GLP-1 drug with the same active ingredient as Ozempic (approved for diabetes). A large review study showed an average weight loss percentage of 11.8% on a 2.4 mg dose of Wegovy.
Zepbound (tirzepatide)—This drug is a combination GLP-1/GIP medication with the same active ingredient as Mounjaro (approved for diabetes). Participants in a clinical trial lost up to 14.7% of their body weight on average when taking the highest dose of 15 mg.
Saxenda (liraglutide)—This is another GLP-1 drug that can help people lose 5–7% of their body weight.
Ozempic (semaglutide) and Mounjaro (tirzepatide) are both FDA-approved for lowering blood sugar in those with type 2 diabetes, but they are also both used off-label for weight management.
All of these drugs are administered through a tiny needle in a once-weekly injection, and they work similarly. They slow down digestion, keeping you feeling fuller longer, and they also act on the part of the brain that sends hunger signals, keeping you from feeling hungry to begin with.
These drugs also have similar side effects profiles, primarily related to digestion (bloating, diarrhea, constipation, gas, etc.), which is understandable considering their mechanisms of action. For most people, the side effects of GLP-1s are usually mild to moderate and tend to ease over time as your body gets used to the medication.
Other weight loss treatments
Other options are available if prescription weight loss medications aren’t right for you.
Weight loss surgery
While surgery is the most invasive form of weight management, many of these procedures have been shown to help with weight loss, including:
Gastric banding: An inflatable band is placed around the stomach to create a smaller pouch, effectively reducing how much food you can eat and makes you feel fuller faster.
Sleeve gastrectomy: This procedure removes most of your stomach, leaving you with a smaller stomach that requires less food to feel full. It has the added benefit of affecting the gut hormones that play a role in hunger, feeling full, and blood sugar control.
Gastric bypass: Also called Roux-en-Y gastric bypass, this is a complicated surgery that reduces the size of your stomach and rearranges the small intestine to decrease calorie absorption. It can also affect your gut hormones.
Weight loss surgery is an effective option for managing weight, but it does come with a risk of side effects and potential complications, such as nausea, vomiting, heartburn, abdominal pain, and infections. Some of these procedures can increase your risk for nutrient deficiencies, like vitamin B12, iron, and folate deficiencies.
Will I gain weight back if I stop weight loss medication?
Unfortunately, even the strongest weight loss pills only work as long as you take them— when you stop them, you will likely gain some weight back. Think of medications as another tool to manage your weight–just like diet and exercise. If you stop exercising, you are likely to gain weight back; similarly, stopping the medication can result in weight regain as well.
Do weight loss pills replace diet and exercise?
As much as we may wish, weight loss pills shouldn’t replace diet and exercise. Weight loss drugs should be part of a comprehensive treatment plan that includes lifestyle modifications, like diet and exercise, counseling, and behavioral interventions. Shifting to an active, healthy lifestyle may also help you minimize weight regain if you stop taking weight loss medications.
People taking weight loss pills along with lifestyle modifications lose, on average, 7–10% of their initial weight after one year. These compounding effects may lower your risk of weight-related health problems like type 2 diabetes and high blood pressure.
Weight loss pills may be the added boost you need to help you lose weight. However, they’re not for everyone. Talk to your healthcare provider about prescription medications for weight management to determine if any are right for you.
Rx weight loss with Ro
Get access to prescription weight loss medication online
Bottom line
If you’ve struggled to lose weight, weight loss pills or other weight loss medications, along with a healthy diet and exercise routine, might be just the ticket to help you achieve your goals.
The strongest weight loss pills are these four FDA-approved options: phentermine/topiramate (Qsymia), naltrexone/bupropion (Contrave), orlistat (Xenical, Alli), and phentermine (Adipex-P, Lomaira).
These weight loss pills can help you lose anywhere from 5–10% of your body weight.
Weight loss pills are only appropriate for certain people, namely adults with either obesity (BMI >30) or overweight (BMI >25), along with at least one weight-related health condition.
Though not in pill form, injectable weight loss medications (like Wegovy and Zepbound) are another, far more effective (on average) option for weight loss.
Your healthcare provider will help you determine which option is right for you.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Wegovy Important Safety Information: Read more about serious warnings and safety info.
Zepbound Important Safety Information: Read more about serious warnings and safety info.
GLP-1 Important Safety Information: Read more about serious warnings and safety info.
Ozempic Important Safety Information: Read more about serious warnings and safety info.
Mounjaro Important Safety Information: Read more about serious warnings and safety info.
Saxenda Important Safety Information: Read more about serious warnings and safety info.
Alonso-Pedrero, L., Bes-Rastrollo, M., & Marti, A. (2019). Effects of antidepressant and antipsychotic use on weight gain: a systematic review. Obesity Reviews, 20(12), 1680-1690. doi: 10.1111/obr.12934. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31524318/
American Diabetes Association Professional Practice Committee. (2024). 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of care in diabetes–2024. *Diabetes Care 1, 47 *(Supplement_1), S145–S157. doi: 10.2337/dc24-S008. Retrieved from https://diabetesjournals.org/care/article/47/Supplement_1/S145/153942/8-Obesity-and-Weight-Management-for-the-Prevention
Apolzan, J. W., Venditti, E. M., Edelstein, S. L., et al. (2019). Long-term weight loss with metformin or lifestyle intervention in the diabetes prevention program outcomes study. Annals of Internal Medicine, 170(10), 682–690. doi: 10.7326/M18-1605. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31009939/
Apovian, C. M., Aronne, L. J., Bessesen, D. H., et al. (2015). Pharmacological management of obesity: an Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology and Metabolism, 100(2), 342–362. doi: 10.1210/jc.2014-3415. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25590212/
Aronne, L. J., Wadden, T. A., Peterson, C., et al. (2013). Evaluation of phentermine and topiramate versus phentermine/topiramate extended-release in obese adults. Obesity (Silver Spring, Md.), 21(11), 2163–2171. https://doi.org/10.1002/oby.20584. Retrieved from https://onlinelibrary.wiley.com/doi/10.1002/oby.20584
Cohen, J. B. & Gadde, K. M. (2019). Weight Loss Medications in the Treatment of Obesity and Hypertension. Current Hypertension Reports, 21(2), 16. doi: 10.1007/s11906-019-0915-1. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6415530/
DailyMed. (2023). Orlistat- capsule. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f81dfaeb-46d5-47ce-9ef6-19259f5ac61c
DailyMed-a. (2022). Qsymia- phentermine and topiramate capsule, extended release. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=40dd5602-53da-45ac-bb4b-15789aba40f9
DailyMed. (2024). Saxenda- liraglutide injection, solution. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3946d389-0926-4f77-a708-0acb8153b143&audience=consumer
DailyMed-b. (2022). Wegovy- semaglutide injection, solution. Retrieved from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=ee06186f-2aa3-4990-a760-757579d8f77b
Davies, M., Færch, L., Jeppesen, O. K., et al. (2021). Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet, 397(10278), 971–984. doi: 10.1016/S0140-6736(21)00213-0. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33667417/
Dimitriadis, G. K., Randeva, M. S., & Miras, A. D. (2017). Potential hormone mechanisms of bariatric surgery. Current Obesity Reports, 6(3), 253–265. doi: 10.1007/s13679-017-0276-5. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5585994/
Fryar, C. D., Carroll, M. D., & Afful, J. (2020). Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats. Retrieved from https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult.htm
Garvey, W. T., Frias, J. P., Jastreboff, A. M., et al. (2023). Tirzepatide once weekly for the treatment of obesity in people with type 2 diabetes (SURMOUNT-2): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet (London, England), 402(10402), 613–626. doi: 10.1016/S0140-6736(23)01200-X. Retrieved from https://pubmed.ncbi.nlm.nih.gov/37385275/
Gorgojo-Martínez, J. J., Basagoiti-Carreño, B., Sanz-Velasco, A., et al. (2019). Effectiveness and tolerability of orlistat and liraglutide in patients with obesity in a real-world setting: The XENSOR Study. International Journal of Clinical Practice, 73(11), e13399. doi: 10.1111/ijcp.13399. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31397946/
Grabarczyk, T. R. (2018). Observational Comparative Effectiveness of Pharmaceutical Treatments for Obesity within the Veterans Health Administration. Pharmacotherapy, 38(1), 19–28. doi: 10.1002/phar.2048. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29044720/
Greenway, F. L., Aronne, L. J., Raben, A., et al. (2018). A randomized, double‐blind, placebo‐controlled study of gelesis100: A novel nonsystemic oral hydrogel for weight loss. Obesity: A Research Journal, 27(2), 205-216. https://doi.org/10.1002/oby.22347. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/oby.22347
Greenway, F. L., Fujioka, K., Plodkowski, R. A., et al. (2010). Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet (London, England), 376(9741), 595–605. doi: 10.1016/S0140-6736(10)60888-4. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20673995/
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., et al. (2022). Tirzepatide once weekly for the treatment of obesity. The New England Journal of Medicine, 387, 205-216. doi: 10.1056/NEJMoa2206038. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa2206038
Kelly, A. S., Auerbach, P., Barrientos-Perez, M., et al. (2020). A randomized, controlled trial of liraglutide for adolescents with obesity. The New England Journal of Medicine (NEJM), 382(22), 2117–2128. doi: 10.1056/NEJMoa1916038. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32233338/
Khera, R., Murad, M. H., Chandar, A. K., et al. (2016). Association of pharmacological treatments for obesity with weight loss and adverse events. JAMA, 315(22), 2424. doi: 10.1001/jama.2016.7602. Retrieved from https://pubmed.ncbi.nlm.nih.gov/27299618/
LeBlanc, E. S., Patnode, C. D., Webber, E. M., et al. (2018). Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA, 320(11), 1172–1191. doi: 10.1001/jama.2018.7777. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30326501/
Lupoli, R., Lembo, E., Saldalamacchia, G., et al. (2017). Bariatric surgery and long-term nutritional issues. World Journal of Diabetes, 8(11), 464–474. doi: 10.4239/wjd.v8.i11.464. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5700383/
Marso, S. P., Daniels, G. H., Brown-Frandsen, K., et al. (2016). Liraglutide and cardiovascular outcomes in type 2 diabetes. The New England Journal of Medicine, 375(4), 311–322. doi: 10.1056/NEJMoa1603827. Retrieved from https://pubmed.ncbi.nlm.nih.gov/27295427/
MedlinePlus. (n.d.). Obesity. Retrieved from https://medlineplus.gov/obesity.html
Onakpoya, I.J., Lee, J.J., Mahtani, K.R., et al. (2020). Naltrexone-bupropion (Mysimba) in management of obesity: A systematic review and meta-analysis of unpublished clinical study reports. British Journal of Clinical Pharmacology, 86(4), 646–667. doi: 10.1111/bcp.14210. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31918448/
Perreault, L. (2021) Obesity in adults: Drug therapy. UpToDate. Retrieved from https://www.uptodate.com/contents/obesity-in-adults-drug-therapy
Pullman, J., Darsow, T., & Frias, J. P. (2006). Pramlintide in the management of insulin-using patients with type 2 and type 1 diabetes. Vascular Health and Risk Management, 2(3), 203-212. doi: 10.2147/vhrm.2006.2.3.203. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1993989/
Qin, W., Yang, J., Deng, C., et al. (2023). Efficacy and safety of semaglutide 2.4 mg for weight loss in overweight or obese adults without diabetes: An updated systematic review and meta-analysis including the 2-year STEP 5 trial. Diabetes, Obesity and Metabolism, 26(3), 911-923. doi: 10.1111/dom.15386. Retrieved from https://dom-pubs.pericles-prod.literatumonline.com/doi/10.1111/dom.15386
Rubino, D., Abrahamsson, N., Davies, M., et al. (2021). Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults With overweight or obesity: The STEP 4 Randomized Clinical Trial. JAMA, 325(14), 1414–1425. doi: 10.1001/jama.2021.3224. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33755728/
Smith, S. M., Meyer, M., & Trinkley, K. E. (2013). Phentermine/topiramate for the treatment of obesity. Annals of Pharmacotherapy, 47(3), 340-349. doi: 10.1345/aph.1R501. Retrieved from https://journals.sagepub.com/doi/10.1345/aph.1R501
Tchang, B. G., Aras, M., Kumar, R. B., et al. (2024). Pharmacologic Treatment of Overweight and Obesity in Adults. In K. R. Feingold (Eds.) et. al. Endotext. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25905267/
U.S. Food and Drug Administration (FDA). (2020). FDA requests the withdrawal of the weight-loss drug Belviq, Belviq XR (lorcaserin) from the market. Retrieved from https://www.fda.gov/drugs/drug-safety-and-availability/fda-requests-withdrawal-weight-loss-drug-belviq-belviq-xr-lorcaserin-market
U.S. Food and Drug Administration (FDA). (2024). Saxenda (liraglutide) injection, for subcutaneous use. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/206321s019lbl.pdf
Wadden, T. A., Chao, A. M., Moore, M., et al. (2023). The role of lifestyle modification with second-generation anti-obesity medications: comparisons, questions, and clinical opportunities. Current Obesity Reports, 12(4), 453–473. doi: 10.1007/s13679-023-00534-z. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10748770/
Wilding, J. P. H., Batterham, R. L., Calanna, S., et al. (2021). Once-weekly semaglutide in adults with overweight or obesity. The New England Journal of Medicine, 384(11), 989–1002. doi: 10.1056/NEJMoa2032183. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33567185/
Yanovski, S. Z. & Yanovski, J. A. (2014). Long-term Drug Treatment for Obesity. JAMA, 311(1), 74. doi: 10.1001/jama.2013.281361. Retrieved from https://pubmed.ncbi.nlm.nih.gov/24231879/
Yerevanian, A. & Soukas, A. A. (2019). Metformin: mechanisms in human obesity and weight loss. Current Obesity Reports, 8(2), 156-164. doi: 10.1007/s13679-019-00335-3. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6520185/
Zheng, M., Soumya, Begum, M., et al. (2023). Do patients with prediabetes managed with metformin achieve better glycaemic control? A national study using primary care medical records. Diabetic Medicine: A Journal of the British Diabetic Association, 40(9), e15170. doi: 10.1111/dme.15170. Retrieved from https://pubmed.ncbi.nlm.nih.gov/37381113/