Here's what we'll cover
Here's what we'll cover
You may not realize it, but ejaculation is a complicated process. When things are running smoothly, it’s kind of like breathing—something you don’t have to think about at all. But when things don’t run smoothly, you can develop ejaculation problems like premature ejaculation and retrograde ejaculation. Retrograde ejaculation, while it won’t hurt you, may lead to male infertility. Let’s take a closer look at retrograde ejaculation.
What is retrograde ejaculation?
During normal ejaculation, semen (ejaculate) is pushed out of the penis (by traveling through the urethra then through the penis via the bladder sphincter). Retrograde ejaculation happens when semen is pushed into the bladder instead of out of the penis (think of a “reverse ejaculation”). A retrograde ejaculation might produce a small amount of semen or none at all. It's also known as a "dry orgasm" (Parnham, 2016).
Retrograde ejaculation is different from semen retention, where people intentionally prevent their semen from exiting the penis. With semen retention, you can press on your perineum, the area between the scrotum and anus, to prevent semen from exiting (which forces the semen into the bladder). For the remainder of this article, we will focus on the medical condition, retrograde ejaculation, and not intentional semen retention.
Retrograde ejaculation symptoms
Many people with this condition don’t have any symptoms. When present, retrograde ejaculation signs and symptoms include:
Dry orgasm: a lack of semen (or very little semen) exiting the penis with orgasm
Cloudy urine: after orgasm, you may notice cloudy urine caused by semen mixing with urine in the bladder
Infertility: difficulty getting someone pregnant
Retrograde ejaculation causes
Before talking about retrograde ejaculation causes, it’s worth mentioning the normal process of ejaculation. During ejaculation, sperm moves from the testicles to the urethra via a tube called the vas deferens. Along the way, the sperm pass into the prostate and mix with the fluids that create semen. As semen moves from the prostate to the urethra, the muscle at the opening of the bladder (the bladder neck muscle or sphincter) tightens to prevent semen from entering the bladder during the muscle contractions of orgasm and semen expulsion.
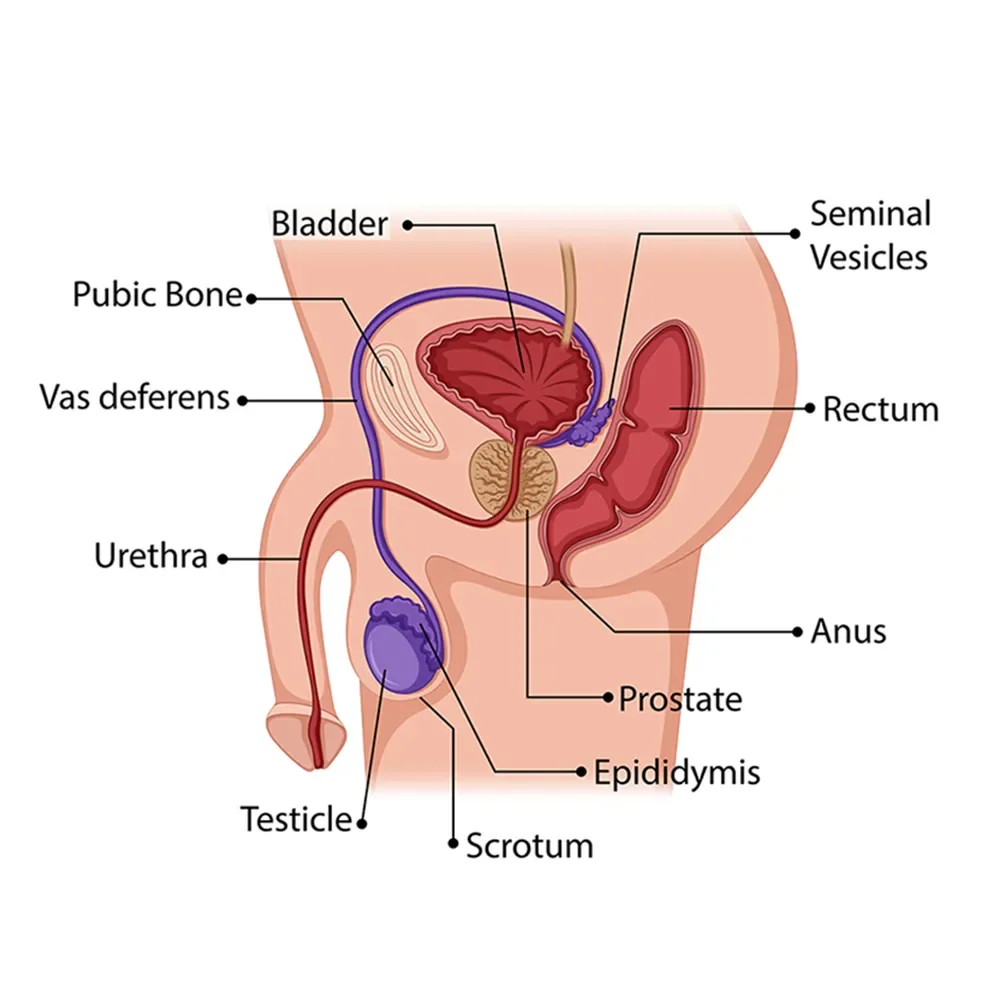
In retrograde ejaculation, the sphincter doesn't tighten sufficiently, either because it's weak or because the nerves controlling the muscle have been damaged. The weakened muscle allows semen to move backward into the bladder. This means that semen doesn’t come out of the penis with the pressure of a normal orgasm and expulsion.
There are several potential causes of retrograde ejaculation, including (Parnham, 2016):
Damage to the nervous system: This can be due to medical conditions (like diabetes, multiple sclerosis, Parkinson’s disease) or trauma (like a spinal cord injury) (Bronner, 2017).
Medications: Drugs that impair the nervous system, including some medicines for depression and alpha-blockers (used to treat high blood pressure and certain prostate conditions), may have retrograde ejaculation as a side effect.
Surgery: Prostate surgery, such as transurethral resection of the prostate (TURP) or retroperitoneal lymph node dissection after testicular cancer, can cause retrograde ejaculation.
Radiation: Radiation therapy to the pelvic area for cancer treatment can have this effect.
Risk factors for retrograde ejaculation
Medical conditions that affect your nervous system and muscle functions increase your risk of developing retrograde ejaculation, including (Parnham, 2016):
Diabetes and diabetic neuropathy
Multiple sclerosis
Parkinson’s disease
Certain drugs have the same effect on the bladder muscle. Medication risk factors for retrograde ejaculation include (Parnham, 2016):
Alpha-blockers used for blood pressure (e.g., doxazosin) or benign prostatic hyperplasia (BPH) (e.g., tamsulosin)
Antidepressants, like duloxetine (Cymbalta) or potentially other selective serotonin reuptake inhibitors (SSRIs) (Egilmez, 2018)
Antipsychotics, like risperidone or thioridazine (Shanmugasundaram, 2019)
How to diagnose retrograde ejaculation
To diagnose the underlying cause of retrograde ejaculation, your provider may perform a urinalysis (checking a urine sample) to look for sperm. You can also check the urine for fructose, a sugar found in semen that is not normally present in urine (Parnham, 2016).
Retrograde ejaculation treatment
Several treatment options may help your retrograde ejaculation.
If your retrograde ejaculation comes from nerves weakened by conditions like diabetes or multiple sclerosis, then medications may help. Some drugs stimulate bladder neck muscle tightening to keep it closed during ejaculation, including (Mostafa, 2021):
Imipramine
Midodrine
Pseudoephedrine
Brompheniramine
However, these drugs won’t help if your problems are due to surgeries or spinal cord injuries that affect your anatomy.
If retrograde ejaculation is causing infertility issues, several sperm retrieval techniques can extract the sperm for in vitro fertilization (IVF) treatment or artificial insemination, including (Parnham, 2016):
Testicular sperm aspiration (TESA), in which a needle is inserted into the testicle and sperm are retrieved;
Percutaneous epididymal sperm aspiration (PESA), in which a needle extracts sperm from the epididymis;
Testicular sperm extraction (TESE), in which a small incision is made in the testes to examine them for the presence of sperm
Rather than trying to get the semen from internal structures, some have had success getting sperm from the urine instead. Talk to your healthcare provider about your treatment options.
Prevention of retrograde ejaculation
You may be able to lower your risk of medically-induced retrograde ejaculation by trying different treatments for BPH (an enlarged prostate). Common medications for BPH relax the bladder neck muscle, which can lead to retrograde ejaculation.
Your healthcare provider may also try to limit medications with a higher risk of causing retrograde ejaculation, including some medicines for high blood pressure, mood disorders, and nerve injuries.
Discuss the risks with your provider before surgery if you need surgery near your bladder or prostate or other surgery that may increase your risk of developing retrograde ejaculation. If your ability to have kids in the future is a concern, talk to your provider about options for saving your sperm for future use before your procedure.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Bronner, G., & Korczyn, A. D. (2017). The role of sex therapy in the management of patients with Parkinson’s disease. Movement Disorders Clinical Practice , 5 (1), 6–13. doi: 10.1002/mdc3.12561. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6174387/
Egilmez OB, Orum MH. (2018). Duloxetine use can result in retrograde ejaculation. Dusunen Adam The Journal of Psychiatry and Neurological Sciences ; 31 : 324-325. doi: 10.5350/DAJPN2018310314. Retrieved from https://dusunenadamdergisi.org/article/68
Mostafa, T., & Abdel-Hamid, I. A. (2021). Ejaculatory dysfunction in men with diabetes mellitus. World Journal of Diabetes , 12 (7), 954–974. doi: 10.4239/wjd.v12.i7.954. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8311479/
Parnham, A., & Serefoglu, E. C. (2016). Retrograde ejaculation, painful ejaculation and hematospermia. Translational Andrology and Urology , 5 (4), 592–601. doi: 10.21037/tau.2016.06.05. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5002007/
Shanmugasundaram, N., Nivedhya, J., Karthik, M. S., & Ramanathan, S. (2019). Risperidone-induced retrograde ejaculation and lurasidone may be the alternative. Industrial Psychiatry Journal , 28 (1), 152–154. doi: 10.4103/ipj.ipj_8_19. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6929214/