Here's what we'll cover
Here's what we'll cover
Here's what we'll cover
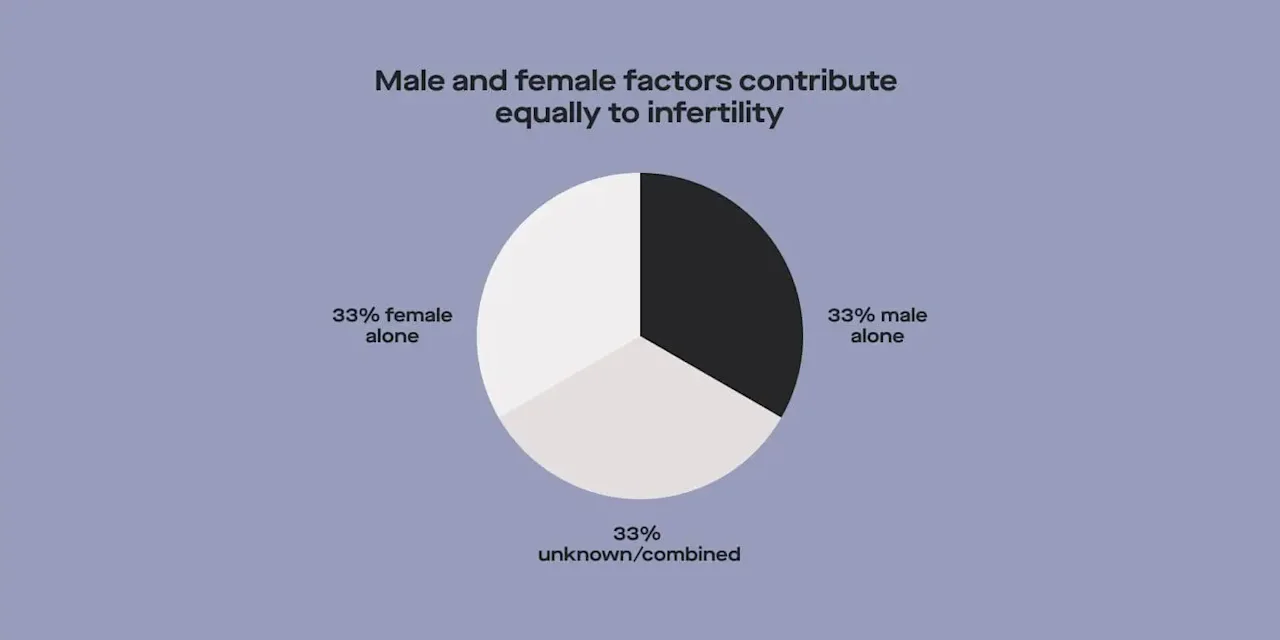
Sperm issues are a major cause of male infertility. Semen analysis is a great tool for understanding the male side of the fertility equation, whether you’re trying for kids now or are planning to try in the future. Male-factor infertility contributes to the inability to conceive about half of the time, so there’s a good reason for people with sperm to get tested.
Read on to learn more about semen analysis, the factors included in a semen analysis, and what to do with your results.
What is a semen analysis?
A semen analysis test gives you a snapshot of sperm quality and quantity. Several different factors can be measured to understand how well sperm can do its job — which is to navigate through the uterus and fallopian tubes and fertilize an egg.
The “factors” (i.e., what’s tested) included in a semen analysis vary. The most basic tests only include sperm count, but many other factors tie into the overall health of sperm.
Before a person can get a semen analysis, they need to provide a sperm sample via masturbation (either in a clinic or using an at-home test kit). For best results, you should maintain a minimum of 3 days and a maximum of 7 days of abstinence before providing this sample. The sample is sent to a lab for analysis, and a report is generated about the different factors tested.
What fertility factors are included in a semen analysis?
Before diving into all of the factors that may be included in a semen analysis, it’s important to understand what a “low” parameter means. These numbers are defined by the World Health Organization (WHO), and having a low parameter doesn’t mean it’s impossible to get a partner pregnant. Rather, it means that there may be a higher likelihood of fertility issues.
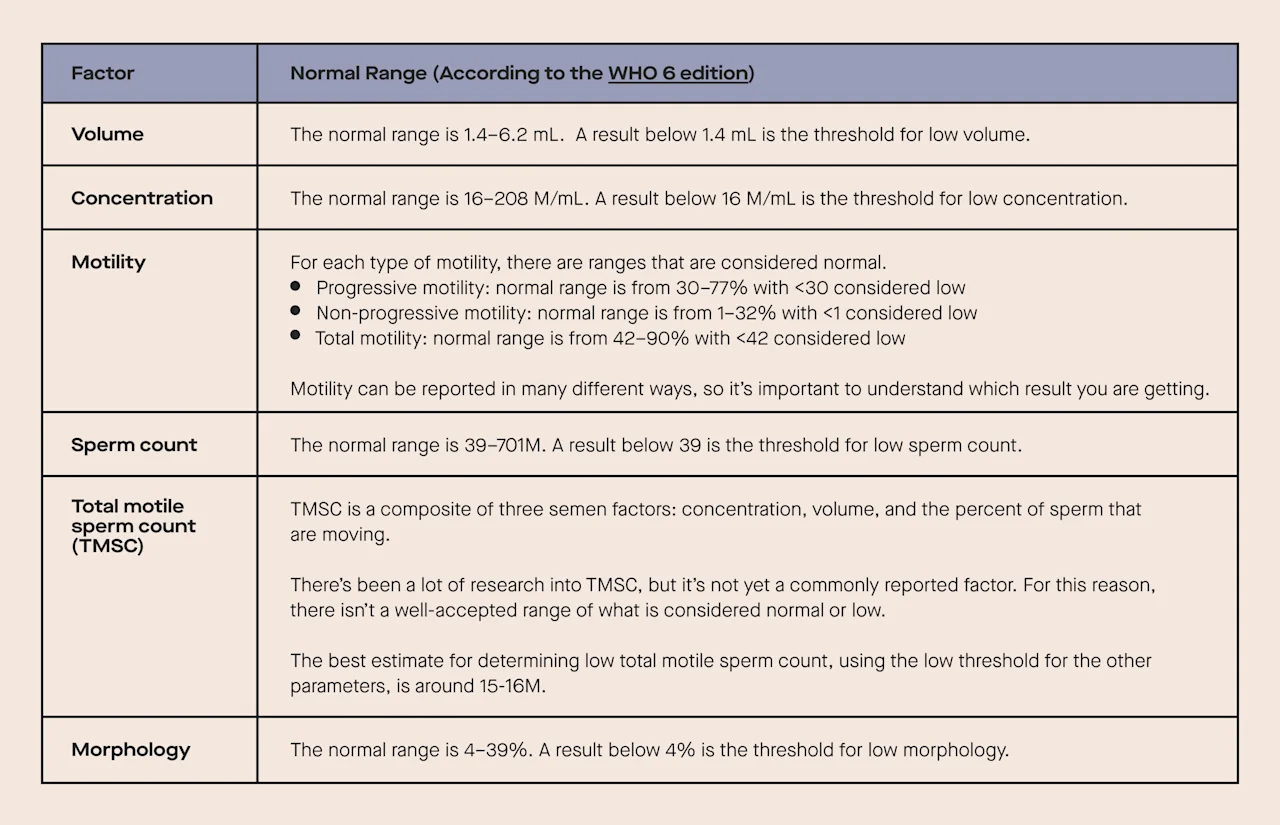
Semen volume
Semen is made up of both sperm cells and seminal fluid. Semen volume is pretty straightforward — it refers to the total amount of fluid in the ejaculate. Anything below 1.5 milliliters (mL) is considered low. Compared to some of the other semen parameters, semen volume doesn’t affect fertility as much. Semen volume naturally declines as men age. However, a low semen volume may suggest underlying issues.
A common reason for low semen volume is not getting the entire sample in the collection cup during the collection, or not abstaining from ejaculating for enough time before the collection. In some cases, low semen volume may be due to medical conditions, like retrograde ejaculation (semen enters the bladder instead of being ejaculated). If the semen volume is low, a second analysis should be performed, taking care to make sure any potential collection issues are addressed. If both results are low, follow up with your healthcare provider to rule out conditions that may cause low volume.
Sperm concentration
Concentration refers to the number of sperm cells per mL of semen and is sometimes referred to as sperm count. Because there are so many sperm in a single milliliter of semen, it’s reported in units of millions per mL (M/mL) and the normal reference range is from 12–16 M/mL. Factors that affect sperm concentration include smoking, overweight/obesity, and heavy alcohol consumption.
Keep in mind that a single low sperm concentration does not mean it’s impossible to conceive with your partner. However, it’s important to discuss the result with your doctor. A low semen concentration usually prompts a repeat semen analysis (in the case of extremely low concentrations, your provider may order additional testing). If the concentration is consistently low, it may take longer for couples to conceive naturally since there are fewer sperm to fertilize the egg.
Sperm motility
Motility refers to how well sperm move. Sperm have to travel through the uterus and fallopian tubes for natural conception to occur. Motility measurements typically refer to the percent of sperm that are moving and are broken down into two types: progressive motility (sperm moving forward) and non-progressive (sperm continues to move but without forward progress). Add these two together and you get total motility.
Progressive motility: 32%
Total motility (progressive + non-progressive): 40%
It is common for some sperm to not be motile, but when the proportion of total moving sperm drops below 40% (or progressive drops below 32%) it may take longer to conceive. Sperm motility is a common contributing factor to male infertility and may be affected by:
Varicocele (enlargement of the veins in the scrotum)
Genetics
Anti-sperm antibodies (an immune response to sperm)
Environmental factors (heat exposure, radiation, etc.)
Lifestyle factors (diet, exercise, weight, drug use, etc.)
The research on methods for improving sperm motility is somewhat limited. Varicocele has been associated with lower sperm motility (along with other parameters), and surgery may be able to help address this issue. Some studies suggest that smoking may adversely impact multiple semen parameters, including motility. Avoiding heat exposure (like hot tubs) while you’re trying to conceive may help motility. Achieving a healthy BMI, eating a nutritious diet, and engaging in regular exercise may also benefit.
Sperm Count
Sperm count is the total number of sperm in the ejaculate and is calculated by multiplying the sperm concentration of a semen sample by its volume. The threshold for low sperm count is 39 million sperm per ejaculate.
The more sperm in the sample, the higher the chances that one of them makes it to the egg to achieve pregnancy. Some studies suggest that Total Motile Sperm Count (TMSC), which refers to the total number of moving sperm in the ejaculate, might be a better measure of fertility than just motility or count alone since it’s a composite of three different semen factors. TMSC comes from multiplying the concentration of a semen sample by its volume and then factoring in the percent of sperm that are moving. While it’s been the subject of several studies, it has yet to make it into the list of commonly reported factors. Because of that, there isn’t a well-accepted range of what is considered normal or low. Several of the factors that affect sperm concentration also influence sperm count, including a high BMI, smoking, drug/alcohol use, stress, and testosterone supplements. This last one might be surprising, but external testosterone can cause the body to stop producing natural testosterone which inhibits sperm production.
Morphology
Sperm morphology refers to the overall shape and structure of individual sperm cells. Morphology is a bit controversial when it comes to its relationship with fertility. So far, studies have not demonstrated a clear link between abnormal morphology and the ability to conceive. Having below 4% of sperm with normal morphology is considered low. However, even people with 0% normal sperm shape can be successful at natural conception.
Research suggests that lifestyle factors do not seem to have much impact on sperm morphology. But given all of the other semen factors discussed, following a healthy lifestyle is a good option for people concerned about fertility.
What to do with your results
Overall, a normal semen analysis is a sign that (as far as the parameters included in the semen analysis go) there aren’t any red flags that are expected to interfere with conception. A normal semen analysis isn’t a guarantee that there won’t be any issues with conception. Remember that fertility is complex, as there are both male and female factors at play. Similarly, an abnormal sperm analysis isn’t a guarantee that there will be issues.The clinical definition of infertility is not achieving a pregnancy after 12 months of unprotected sex if your female partner is <35 and 6 months if your partner is 35 or older.
If one or more of your semen analysis results are abnormal, the current standard of care is to perform a second test, to account for natural variability. If your first test was an at-home test, consider performing the repeat analysis in a lab where it can be analyzed promptly. In addition, your lifestyle leading up to collection can impact test results (for example, using a hot tub frequently before testing).
Your healthcare provider or fertility specialist can help you confirm a diagnosis of infertility and walk you through your options, including further testing, treatment, fertility preservation, or assisted reproductive technologies, like in vitro fertilization (IVF).
The bottom line
Doing a semen analysis is one of the best ways to get insight into male fertility — but semen analysis alone can’t tell you if you’re fertile or infertile. It only gives you a snapshot of your sperm, but can’t tell you *why* you have the parameters you do. That’s where your healthcare provider can help. When it comes to fertility, the more info you have, the more options you have.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
References
Agarwal, A., Sharma, R., Harlev, A., et al. (2016). Effect of varicocele on semen characteristics according to the new 2010 World Health Organization criteria: a systematic review and meta-analysis. Asian Journal of Andrology, 18 (2), 163–170. doi:10.4103/1008-682X.172638. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4770480/
Sun, B., Messerlian, C., Sun, Z. H., et al. (2019). Physical activity and sedentary time in relation to semen quality in healthy men screened as potential sperm donors. Human Reproduction, 34 (12), 2330–2339. doi:10.1093/humrep/dez226. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31858122/
Boeri, L., Capogrosso, P., Ventimiglia, E., et al. (2019). Heavy cigarette smoking and alcohol consumption are associated with impaired sperm parameters in primary infertile men. Asian Journal of Andrology, 21 (5), 478–485. doi:10.4103/aja.aja_110_18. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6732890/
Danis, R. B. & Samplaski, M. K. (2019). Sperm morphology: history, challenges, and impact on natural and assisted fertility. Current Urology Reports, 20 (8), 43. doi:10.1007/s11934-019-0911-7. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31203470/
Dcunha, R., Hussein, R. S., Ananda, H., et al. (2022). Current insights and latest updates in sperm motility and associated applications in assisted reproduction. Reproductive Sciences, 29 (1), 7–25. doi:10.1007/s43032-020-00408-y. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33289064/
Hamilton, J. A., Cissen, M., Brandes, M., et al. (2015). Total motile sperm count: a better indicator for the severity of male factor infertility than the WHO sperm classification system. Human Reproduction, 30 (5), 1110–1121. doi:10.1093/humrep/dev058. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25788568/
Oostingh, E. C., Steegers-Theunissen, R. P., de Vries, J. H., et al. (2017). Strong adherence to a healthy dietary pattern is associated with better semen quality, especially in men with poor semen quality. Fertility and Sterility, 107 (4), 916–923.e2. doi:10.1016/j.fertnstert.2017.02.103. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28292616/
Pacey, A. A., Povey, A. C., Clyma, J. A., et al. (2014). Modifiable and non-modifiable risk factors for poor sperm morphology. Human Reproduction, 29 (8), 1629–1636. doi:10.1093/humrep/deu116. Retrieved from https://pubmed.ncbi.nlm.nih.gov/24899128/
Patel, A. S., Leong, J. Y., Ramos, L., et al. (2019). Testosterone is a contraceptive and should not be used in men who desire fertility. The World Journal of Men's Health, 37 (1), 45–54. doi:10.5534/wjmh.180036. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6305868/
Practice Committee of the American Society for Reproductive Medicine. (2018). Smoking and infertility: a committee opinion. Fertility and Sterility, 110 (4), 611–618. doi:10.1016/j.fertnstert.2018.06.016. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30196946/
Salas-Huetos, A., Maghsoumi-Norouzabad, L., James, E. R., et al. (2021). Male adiposity, sperm parameters and reproductive hormones: An updated systematic review and collaborative meta-analysis. Obesity Reviews : an official journal of the International Association for the Study of Obesity, 22 (1), e13082. doi:10.1111/obr.13082. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32705766/
Sunder, M. & Leslie, S. W. (2022). Semen analysis. StatPearls . Retrieved on Mar. 16, 2023 from https://www.ncbi.nlm.nih.gov/books/NBK564369/
WHO laboratory manual for the examination and processing of human semen, sixth edition. Geneva: World Health Organization; 2021. Retrieved from https://www.who.int/publications/i/item/9789240030787
Schlegel, P. N., Sigman, M., Collura, B., et al. (2021). Diagnosis and treatment of infertility in men: AUA/ASRM Guideline Part I. The Journal of Urology, 205 (1), 36–43. doi:10.1097/JU.0000000000001521. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33295257/