Here's what we'll cover
Here's what we'll cover
Every person is so much more than their weight. Sure, weight might be one aspect of your overall health, but it’s not the whole picture. What constitutes a healthy weight is different for everyone. That said, understanding where your weight falls on the medical spectrum—underweight, normal, overweight, obese, or morbidly obese—can help you get a better idea of your risk for potential health problems down the line.
So, what is morbid obesity? Continue reading to learn more about this condition, its risk factors, and what morbid obesity potentially means for your overall health, both now and in the future.
What is obesity?
In simple terms, obesity means having too much fat on the body. Weight comes from a variety of sources, including muscle, bone, water, and body fat. While body fat is needed to maintain proper health, too much body fat can potentially cause certain weight-related health problems (Medline Plus, n.d.).
But how do you know how much body fat is too much? Healthcare providers often use body mass index (BMI) to determine where a person's weight falls on the medical spectrum. BMI is calculated with a formula that considers height and weight, but it doesn't take other factors like muscle mass, bone density, body composition, and ethnic/racial background into account. Additionally, data to support BMI is pulled almost entirely from white populations. So your BMI is not the only factor to consider in the diagnosis of obesity.
That being said, BMI scores are divided into four categories:
Underweight (BMI below 18.5)
Normal (BMI of 18.5 to 24.9)
Overweight (25 to 29.9)
Obese (BMI of 30 or above)
According to the National Institutes of Health (NIH), one in three adults is considered to be obese, and one in 11 adults is considered to be morbidly obese in the United States (NIDDK-a, 2021).
Find out how much you could lose
Provide your biometric data to get started.

0.0
Your BMI
Underweight
< 18.5
Healthy weight
18.5 - 24.9
Overweight
24.9 - 29.9
Obesity
> 30
What is morbid obesity?
A person is considered obese if their BMI is higher than 30. There are different levels of obesity, broken down into three main categories:
Class 1: BMI is 30 to 34.9
Class 2: BMI is 35 to 39.9
Class 3: BMI is 40 or above
According to the U.S. Centers for Disease Control and Prevention (CDC), morbid obesity, also known as Class 3 obesity, is a BMI above 40 (CDC-a, 2022).
Risk factors for morbid obesity
A simplified explanation for morbid obesity is that a person eats more calories than they expend through activity (although many other factors, including medical, lifestyle, and otherwise contribute to weight gain). The amount of calories each person should eat per day is dependent on their age and lifestyle. For example, someone who exercises a lot will need to eat more than someone who doesn't exercise at all. Recommended calorie intake is typically somewhere around 1,600 to 2,400 calories per day for biological adult women and 2,000 to 3,000 calories per day for biological adult men (HHS, 2022).
In addition to eating more calories than burned, here are some other factors shown to affect weight gain:
Family history and genetics
Your genetics can have an impact on your chances of developing morbid obesity.
Children born to obese parents are more likely to be obese than children with one or more lean parents. One study found that boys who have overweight parents are 1.7 times more likely to be overweight than their peers with non-overweight parents—and the results were similar for girls (Bahreynian, 2017).
Lifestyle
Weight gain is not only influenced by the number of calories you eat, but how many you burn off each day. According to current guidelines, adults should get 150 minutes of moderate-intensity physical activity and two days of muscle strengthening activity each week (HHS, 2018).
While ideal, these goals aren’t reasonable for every person. Jobs, pets, children, and other responsibilities mean we don’t always have two and a half hours a week to devote to exercise. The good news is, when it comes to exercise, something is always better than nothing! So find an exercise that you enjoy and stick with it.
Age
Morbid obesity can develop at any stage of life, but hormonal changes that come with age—coupled with decreased activity—can be a contributing factor. Recent statistics show that obesity levels increase as a person ages. Data shows that almost 45% of middle-aged adults aged 40–59 and nearly 43% of adults aged 60 or older have obesity (NIH, 2022).
Certain medical conditions
Multiple disorders and conditions have the potential to cause weight gain. For example, hypothyroidism—a condition that causes a person's metabolism to work slower than normal—can have an impact on weight (Sanyal, 2016).
Another condition linked to weight gain is polycystic ovarian syndrome (PCOS). PCOS currently affects approximately five million people in the U.S. of childbearing age. The imbalance of hormones in people with PCOS often contributes to weight gain (CDC-b, 2022).
Certain medications
A number of medications prescribed by healthcare providers are shown to cause, or contribute to, weight gain.
Some medications used to treat depression and anxiety are shown to cause a modest increase in weight over time. Other medications shown to be related to weight gain include certain diabetes medications, medications to treat certain mental illnesses, birth control pills, some seizure medications, and corticosteroids.
Signs and symptoms of morbid obesity
You can't tell if a person has morbid obesity simply by looking at them. However, a large buildup of excess fat—especially around the stomach and hips—may be one part of the screening process to determine if a person has morbid obesity.
People with morbid obesity often have other physical symptoms due to the accumulation of excess fat, including difficulty with physical activities like walking. They may also have trouble breathing and get easily winded.
How is morbid obesity diagnosed?
Morbid obesity is most often diagnosed by healthcare providers using BMI.
Some providers will also use other measurements like body fat percentage, waist circumference, waist-to-hip ratio, and waist-to-height ratio to diagnose obesity.
Health risks associated with morbid obesity
While having morbid obesity doesn't automatically mean a person will develop health issues, it is a risk factor for many chronic diseases.
Type 2 diabetes
High levels of body fat is one of the strongest risk factors for developing diabetes. Morbid obesity increases the risk of developing the disease, but research suggests that it may go into remission after a person loses as little as 10 percent of their body weight (Dambha-Miller, 2019).
Heart disease
Having morbid obesity increases a person's risk of developing cardiovascular disease, including heart attacks, peripheral artery disease, arrhythmias, and heart failure. Not only that, but a high BMI can cause heart disease at a younger age (Khan, 2018).
Stroke
Having obesity is a major risk factor for strokes (Shiozawa, 2021). Strokes occur when the blood supply to the brain is blocked and can result in muscle weakness, brain damage, or even death.
High blood pressure
Studies suggest that obesity may be the cause of high blood pressure in 65–78% of people (Shariq, 2020).
Sleep apnea
Morbid obesity is shown to cause sleep apnea because excess weight puts pressure on the upper airways, which makes breathing more difficult. Losing a small percentage of body weight can decrease the severity of sleep apnea (Schwartz, 2008).
Arthritis
Arthritis (osteoarthritis) is a syndrome that causes joint degeneration and affects more people than any other type of joint disease.
Morbid obesity is one of the risk factors of osteoarthritis because weight-bearing joints—like the knees—aren't made to carry around excessive weight. Research shows that U.S. adults with obesity are almost 7 times more likely to develop osteoarthritis of the knee than people without obesity (King, 2013).
Some cancers
People with obesity are shown to have consistent low-level inflammation, which can cause DNA damage over time. This can lead to certain cancers. Esophageal, thyroid, liver, kidney, endometrial, pancreatic, and colon cancers are among some of the cancers linked to obesity (NIH, 2022).
Treatment for morbid obesity
Morbid obesity can be reversed, but it takes time and effort to go from morbidly obese to a healthy weight. Treatment options range from lifestyle changes to surgery—and each comes with advantages and disadvantages.
Diet and exercise
Losing just 5 to 10 percent of body weight can decrease the chances of developing obesity-related health problems (Medline Plus, n.d.).
Weight loss medications
While there is no magic pill to help you lose weight, there are certain medications shown to help reduce weight when used with a healthy diet and exercise routine.
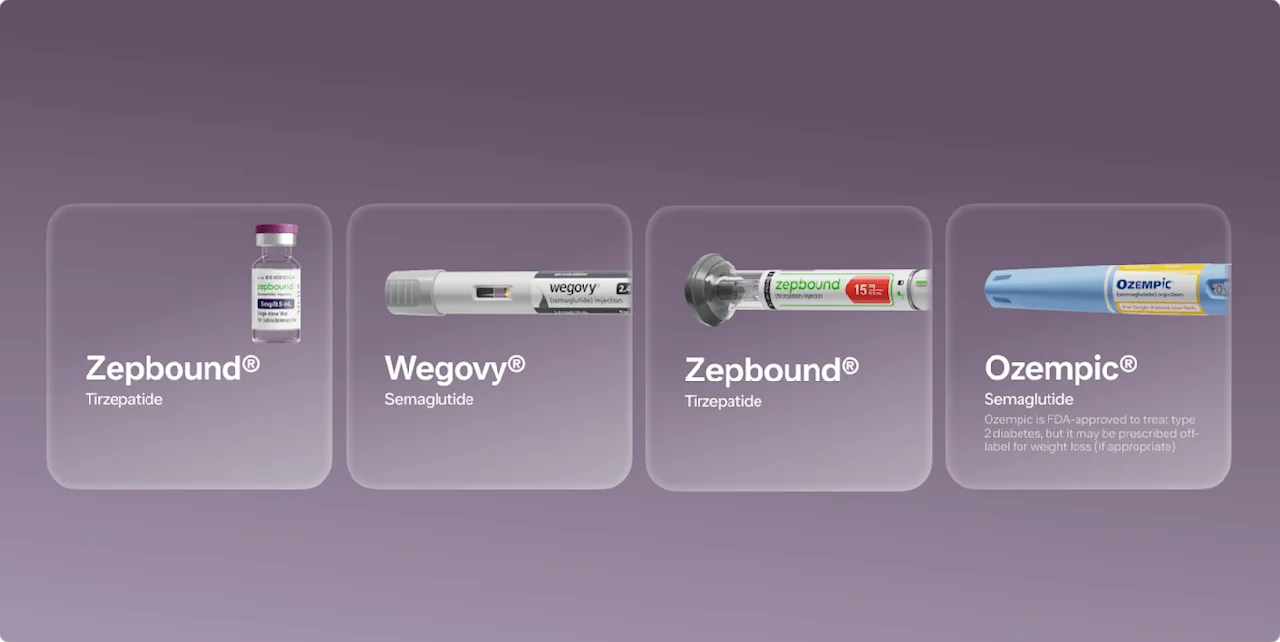
The U.S. Food and Drug Administration (FDA) has approved six medications for weight loss: semaglutide (Wegovy; see Important Safety Information), orlistat (Xenical), setmelanotide (Imcivree), phentermine-topiramate (Qsymia), naltrexone-bupropion (Contrave), and liraglutide (Saxenda). Each FDA-approved weight loss medication has its own benefits and side effects (NIDDK-b, 2021).
Weight loss surgeries
Weight-loss surgery—also called bariatric surgery—is shown to be one of the most effective treatments for people with morbid obesity. Along with weight loss, surgery can help reduce the risk of obesity-related health problems and increase life expectancy (Arterburn, 2020).
You should always seek guidance from a healthcare provider before embarking on a weight loss journey. Your healthcare provider can evaluate your health to determine which weight loss method (if any) is right for you.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Arterburn, D. E., Telem, D. A., Kushner, R. F., et al. (2020). Benefits and risks of bariatric surgery in adults: a review. JAMA, 324 (9), 879–887. doi:10.1001/jama.2020.12567. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32870301/
Bahreynian, M., Qorbani, M., Khaniabadi, B. M., et al. (2017). Association between obesity and parental weight status in children and adolescents. Journal of Clinical Research in Pediatric Endocrinology, 9 (2), 111–117. doi: 10.4274/jcrpe.3790. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28008863/
Dambha-Miller, H., Day, A. J., Strelitz, J., et al. (2019). Behaviour change, weight loss and remission of Type 2 diabetes: a community-based prospective cohort study. Diabetic Medicine : a Journal of the British Diabetic Association , 37 (4), 681–688. doi:10.1111/dme.14122. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31479535/
Khan, S. S., Ning, H., Wilkins, J. T., et al. (2018). Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiology, 3 (4), 280. doi:10.1001/jamacardio.2018.0022. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29490333/
King, L. K. & Anandacoomarasamy, A. (2013). Obesity & osteoarthritis. Indian Journal of Medical Research, 138 (2), 185–193. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3788203/
MedlinePlus. (n.d.). Obesity. Retrieved from https://medlineplus.gov/obesity.html
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2021-a). Overweight & Obesity Statistics. Retrieved from https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2021-b). Prescription Medications to Treat Overweight and Obesity. Retrieved from https://www.niddk.nih.gov/health-information/weight-management/prescription-medications-treat-overweight-obesity
National Institutes of Health (NIH). (2022). Obesity and Cancer Fact Sheet. Retrieved from https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet
Sanyal, D. & Raychaudhuri, M. (2016). Hypothyroidism and obesity: an intriguing link. Indian Journal of Endocrinology and Metabolism, 20 (4), 554. doi: 10.4103/2230-8210.183454. Retrieved from https://pubmed.ncbi.nlm.nih.gov/27366725/
Schwartz, A. R., Patil, S. P., Laffan, A. M., et al. (2008). Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proceedings of the American Thoracic Society, 5 (2), 185–192. doi:10.1513/pats.200708-137mg. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2645252/
Shariq, O. A. & McKenzie, T. J. (2020). Obesity-related hypertension: a review of pathophysiology, management, and the role of metabolic surgery. Gland surgery, 9 (1), 80–93. doi:10.21037/gs.2019.12.03. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7082272/
Shiozawa, M., Kaneko, H., Itoh, H., et al. (2021). association of body mass index with ischemic and hemorrhagic stroke. Nutrients, 13 (7), 2343. doi:10.3390/nu13072343. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34371853/
U.S. Centers for Disease Control and Prevention (CDC). (2022-a). Defining adult overweight & obesity. Retrieved from https://www.cdc.gov/obesity/basics/adult-defining.html
U.S. Centers for Disease Control and Prevention (CDC). (2022-b). PCOS (Polycystic Ovary Syndrome) and Diabetes. Retrieved from https://www.cdc.gov/diabetes/basics/pcos.html
U.S. Department of Agriculture (USDA) and U.S. Department of Health and Human Services (HHS). (2022). Dietary Guidelines for Americans, 2020-2025. 9th Edition. Retrieved from https://DietaryGuidelines.gov .
U.S. Department of Health and Human Services (HHS). (2018). Physical activity guidelines for Americans, 2nd edition. Washington, DC: U.S. Retrieved from https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf